Abstract
Introduction
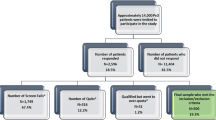
This cross-sectional survey was conducted with National Psoriasis Foundation (NPF) to capture treatment perspectives and expectations in patients with psoriasis (PsO) using Patient Needs Questionnaire (PNQ) of Patient Benefit Index (PBI).
Methods
Adult participants with self-reported diagnosis of PsO responded to the PNQ portion of PBI by indicating how much they valued different treatment attributes. All the treatment goals were captured on a five-point Likert scale (0 = “Not important”, 4 = “Very important”). Treatment goals were obtained for overall population and subgroups based on severity of disease Patient Global Assessment (PGA), age, gender, and Dermatology Life Quality Index (DLQI) total score. All data were expressed as mean and standard deviation [SD].
Results
A total of 1200 participants completed the survey (mean age 51.5 years). Top treatment goal in the overall population was “to have confidence in the therapy” (3.46 [1.01]). Unique to the higher severity subgroup (PGA ≥ 3), “to find a clear diagnosis and therapy” was a top five goal and “to get better skin quickly” was for those with lesser severity (PGA < 3). “To be free of itching” (3.36 [0.99]) was the unique goal in the < 40 age group whereas it was “to get better skin quickly” (3.27 [1.12]) in the ≥ 40 group. In women and men, “to be free of itching” (3.38 [1.13]) and “to get better skin quickly” (3.20 [1.09]) were top five goals, respectively. Patients with ≥ 10 DLQI scores expressed higher treatment goal “to regain control of the disease” (3.66 [0.67]) compared to those with ≤ 10 DLQI scores who expressed “to have confidence in the therapy” (3.40 [1.11]) as the topmost treatment goal.
Conclusion
Our results suggest that in patients with PsO, treatment preferences can vary with different characteristics such as age, severity, and gender as measured by using PNQ. Further exploration of this data will help inform treatment decisions and optimize patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
A wide range of treatment goals using the Patient Needs Questionnaire (PNQ) as part of the Patient Benefit Index (PBI) have been explored in patients with moderate-to-severe psoriasis (PsO), and/or nail PsO in European studies. |
However, assessment of patient treatment goals in PsO using the PNQ has not been studied in the USA. |
Therefore, this cross-sectional survey was conducted with the National Psoriasis Foundation (NPF) to capture treatment perspectives and expectations in patients with PsO using the PNQ of PBI. |
What was learned from the study ? |
Top five treatment goals in the overall study population were “to have confidence in the therapy”, “to regain control of the disease”, “to have no fear that the disease will become worse”, “to get better skin quickly”, and “to be free of itching”. |
Further exploration of this data will help inform treatment decisions and optimize patient outcomes. This approach may improve treatment satisfaction, adherence, and long-term outcomes. |
Introduction
Psoriasis (PsO) is a chronic, immune-mediated, systemic inflammatory skin condition, affecting 1–3% of the world’s population [1, 2]. Besides causing significant disease burden, PsO also impairs quality of life (QoL), emotional, and physical well-being [1, 2]. Depending on PsO severity, the condition is often treated with topical medications, phototherapy, and systemic drugs such as methotrexate, cyclosporine, and acitretin [3]. More recently approved biologic therapies for PsO vary widely in their benefit/risk profiles, as well as in other aspects related to convenience [3].
Dermatologists are guided by many evidence-based guidelines for making treatment choices; however, the treatment goals are usually based on measures such as Body Surface Area (BSA) or Psoriasis Area and Severity Index (PASI) [4]. Furthermore, research shows that patients with PsO focus more on symptoms such as itch, pain, scaling, and flaking [5], whereas dermatologists focus on objective measures such as clearance of lesions [6].
In this view, joint guidelines from the American Academy of Dermatology (AAD) and National Psoriasis Foundation (NPF) recommend tailoring treatment to the individual needs of patients [7]. In addition, understanding preferences of patients for treatment attributes can lead to greater treatment satisfaction and adherence [8,9,10,11].
Since PsO affects all elements of QoL [12, 13], it is important to address treatment goals representing different health domains to understand patient-relevant benefits of various therapies. In this regard, the Patient Benefit Index (PBI) is a validated, disease-specific patient-reported outcomes instrument to assess treatment benefit while considering the importance of patients’ treatment goals [14].
The importance of the treatment objectives in PsO can be measured using the Patient Needs Questionnaire (PNQ), the first part of the Patient Benefit Index (PBI), where the patients rate the importance of each goal on a five-point Likert scale (or choose “does not apply to me”) from a list of 25 different treatment goals [15]. Treatment goals using the PNQ as part of the PBI have been explored in patients with moderate-to-severe PsO, and/or nail PsO in European studies [10, 16, 17]. However, assessment of patient treatment goals in PsO using the PNQ has not been studied in the USA.
To further our understanding of how PsO and its treatments impact on patients’ lives, the current survey was conducted with the NPF, a USA-based psoriatic disease patient advocacy group using the PNQ of PBI. This survey was designed to capture the perspectives of patients with PsO by using PNQ in the USA.
Methods
Study Design and Patient Population
This was an online cross-sectional survey-based analysis, where participants responded to the PNQ portion of PBI by indicating how much the patients valued different treatment attributes. The NPF recruited survey participants using emails and social media.
Patients (18 years of age or older) with self-reported diagnosis of PsO, a US resident with ability to read and understand English, and willing to give written informed consent approval were included. On the other hand, any respondent unwilling or unable to provide informed consent was excluded from this study.
The study protocol was approved by the Genetic Alliance Institutional Review Board (protocol approval# NPF1801) This study was conducted in accordance with the Helsinki Declaration 1964, and its later amendments, Good Pharmacoepidemiology Practices, and applicable laws and regulations of the USA. All patients provided informed consent for participation.
Patient Benefit Index and Patient Needs Questionnaire
The PBI consists of two parts: in the PNQ, patients rate the perceived importance of different treatment goals before initiating therapy; in the Patient Benefit Questionnaire (PBQ), patients rate the achievement of these treatment goals following therapy [16, 18].
The PBI total score is the arithmetic mean of all PBQ items weighted by the relative importance of each corresponding need item derived from the PNQ for each patient.
The current study focused on PNQ responses in all patients who participated in the NPF survey. The PNQ consists of a list of 25 items to capture the treatment goals along with an exploratory item (added particularly for this survey) on importance of reducing PsO to ≤ 1% BSA. Each goal was scored on a five-point Likert scale: 0 = “Not important”, 4 = “Very important”. For each treatment goal item in the PNQ, mean importance at baseline was determined.
Psoriasis Symptom Severity Items
The survey assessed the severity of four PsO symptoms (itch, pain, burning, and scaling) each using a 0–10 numeric rating scale format (0 = none, 10 = severe). The patient was asked to rate the worst level of severity of each symptom in the past 24 h.
Statistical Analysis
Patient demographics, disease characteristics, and treatment goals were summarized for all patients enrolled using descriptive statistics expressed as mean and standard deviation (SD). Descriptive statistics on the mean for answers to each of the items were conducted for the overall study population and for various subgroups based on severity of disease (Patient Global Assessment [PGA] < 3 vs. PGA ≥ 3), age (< 40 vs. ≥ 40 years), gender (female vs. male), Dermatology Life Quality Index (DLQI) total score (≤ 10 vs. > 10), and for those who used biologics in the last 6 months.
Results
A total of 1200 participants completed the survey. Detailed demographic and clinical characteristics are shown in Table 1. The study included 416 (34.7%) men and 784 (65.3%) women with mean (SD) age of 51.5 (13.9) years. A total of 46.4% patients had psoriatic arthritis with mean (SD) disease duration of 22.8 (17.3) years. Most of the patients (43.4%) had self-described moderate PsO (BSA ≤ 2).
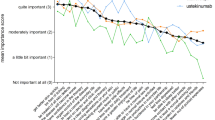
Detailed therapy goals and their mean scores are presented in Table 2. The top five treatment goals with the highest mean (SD) score were “to have confidence in the therapy” (3.46 [1.01]), “to regain control of the disease” (3.46 [1.03]), “to have no fear that the disease will become worse” (3.41 [1.03]), “to get better skin quickly” (3.27 [1.11]), and “to be free of itching” (3.27 [1.19]) (Table 2). All the top five treatment goals were considered important/very important as graded by more than 75% of the overall population.
The treatment goals were further explored across different subgroups. In the lesser severity subgroup (PGA < 3, N = 698), “to have confidence in the therapy” (3.40 [1.12]) was the topmost treatment goal, whereas in patients with higher severity of PsO (PGA ≥ 3, N = 502), it was “to regain control of the disease” (3.61 [0.77], Fig. 1a). “To get better skin quickly” was a unique top five goal of the lesser severity group whereas it was “to find a clear diagnosis and therapy” in those with higher severity.
In both age subgroups (< 40 and ≥ 40 years), “to have confidence in therapy”, “to have no fear that the disease will become worse”, and “to regain control of the disease” were the common treatment goals (Fig. 1b). In younger patients (< 40 years), “to reduce the amount of psoriasis covering your skin to ≤ 1% BSA” (3.36 [1.02]) and “to be free of itching” (3.36 [0.99]) were unique “top five” goals, whereas “to find a clear diagnosis and therapy” (3.27 [1.26]) and “to get better skin quickly” (3.27 [1.12]) were unique goals in older patients.
The top five treatment goals in the women (N = 784) and men (N = 416) are represented in Fig. 1c. Women expressed higher expectations from therapy across all goals when compared to male counterparts. “To regain control of the disease” (3.55 [0.98], 3.28 [1.11]), “to have confidence in therapy” (3.51 [1.00], 3.37 [1.02]), and “to have no fear that the disease will become worse” (3.50 [0.98], 3.23 [1.09]) were the common “top five” goals in women and men, respectively.
Patients with ≥ 10 DLQI scores (N = 422) expressed higher treatment goal expectations. “To be able to lead a normal day life” (3.61 [0.76]) and “to experience a greater enjoyment of life” (3.59 [0.83]) were the unique treatment goals in the higher DLQI group, whereas it was “to be healed of all skin lesions” (3.12 [1.20]) and “to get better skin quickly (3.14 [1.21])” in the lower DLQI group (Fig. 1d).
“To be able to lead a normal day life” (3.49 [0.88]) and “to find a clear diagnosis and therapy” (3.41 [0.99]) were unique treatment goals in patients who reported use of biologics within the previous 6 months (N = 291) when compared to those with no biologic use within the previous 6 months (N = 909) who reported “to be healed of all skin lesions” (3.26 [1.14]) and “to get better skin quickly” (3.25 [1.14]) as one of the “top five” treatment goals (Fig. 1e).
In a subgroup of patients who indicated that they started biologic therapy at the time of the study (N = 297), “to regain control of the disease” (3.54 [0.81]), “to have no fear that the diseases will become worse” (3.51 [0.84]), “to have confidence in the therapy” (3.46 [0.92]), “to be able to lead a normal day life” (3.40 [0.98]), and “to be free of itching (3.41 [0.94]) were the “top five” treatment goals (data not shown).
Treatment goals based on treatment class (biologics, non-biologic systemic therapy, phototherapy, non-topical steroids, and topical steroids) are presented in the Supplementary Table 1. “To have confidence in the therapy” and “to regain control of the disease” were the common “top five” treatment goals across all treatment classes.
Discussion
To our knowledge, this is the first study that fully explored treatment goals important to patients, as measured by the PNQ in a US population with PsO. To have confidence in the therapy, to regain control of the disease, to have no fear that the disease will become worse, to get better skin quickly, and to be free of itching were among the top five needs for the overall survey population in this study. Overall, “to be free of itching” was found to be a frequent treatment goal in our study, which is in line with previous reports indicating the high prevalence of itch in PsO [19]. Our findings also show that PsO treatment preferences can differ between patients with different characteristics such as PsO severity, age, and gender. Specifically, to find a clear diagnosis and therapy was among the top needs for female patients; reducing PsO coverage to 1% or less BSA was a top goal of younger patients and male patients.
The study entry requirements did not include PsO severity criteria, though there was a goal to recruit approximately 40% who indicated they were using biologic therapy in the treatment of their PsO. Likely owing to the recruitment goal, the majority of patients in our study reported moderate to severe PsO (≥ 3% BSA) while 43% reported mild PsO (BSA ≤ 2%). Our study population is not representative of the general PsO population as reported in a large National Health and Nutrition Examination Survey using a similar severity classification that found the majority (approximately 82%) of patients had “little/no” to “mild” PsO [20].
Results from a previous survey on patients with low disease activity have reported treatment goals such as “to have confidence in therapy”, “be healed of all skin defects”, and “be free of itching” as their top priorities and were ranked as “quite” to “very” important (78.5%) [21]. Another study by Maul et al. reported that in a cohort with high disease activity (mean PASI 14.2 ± 9.7, DLQI 11.3 ± 7.2), “to get better skin quickly” and “to be healed of all skin defects” were most important to patients [22]. Thus, irrespective of disease severity, these treatment goals remain the top requisites of patients and are in corroboration with our findings.
Although not reported as “top five”, “to have confidence in therapy” was an important therapy expectation in patients as reported in another study using the PNQ [22]. However, the meaning of confidence as expressed by the patients was neither defined in the current or the reference study.
There was variation in relative rank order in treatment goals from our study to the reported literature. “To have fewer out-of-pocket-expenses” was the 10th goal in our study, whereas it was the 25th and 16th goal in other cohorts [21, 22]. The variation observed could plausibly be due to the differences in healthcare systems across geographies [23].
Our results show that, on average, women have different treatment needs and expectations than men. This might possibly be driven by aesthetic and social expectations that women experience in everyday life [24, 25]. “To feel less depressed” and “to be more comfortable showing yourself in public” were significantly more important treatment goals reported by female patients compared to male patients in other survey results that applied PNQ [21, 24]. In our study, female patients perceived “to have no fear that the disease will become worse” as a top five treatment goal, suggesting that various psychological factors might be playing a role during exacerbation of flares, especially in women, and therefore must be taken into treatment consideration [22].
The needs of patients in PsO and their correlation with age have not been studied sufficiently [10, 26]. Similar to our data, Maul et al. reported that older patients (≥ 65 years) attributed more importance “to have confidence in the therapy” compared to the younger population (< 65 years) [22].
Application of PNQ in this study facilitates communication related to treatment goals and that the PNQ is a helpful and more accurate tool when defining patients’ needs [15]. Accurate information concerning patients’ needs can be helpful in selecting specific drugs that best fit the profile of the respective patient, thus resulting in a more personalized treatment approach. Further exploration of this data will help inform treatment decisions and optimize patient outcomes. PsO treatment guidelines also recognize the importance of tailoring treatment to the needs of the individual patient [7, 27].
Our study had certain limitations. The study data was entirely patient reported, including the diagnosis (by a healthcare professional) of PsO and the severity of PsO; patient-reported disease characteristics may not be reliable. Since patients were recruited from an online panel, they might not have represented the overall population of patients with PsO in the USA. This was a cross-sectional survey and did not have PBQ follow-up data, which measures the extent to which the treatment needs have been fulfilled by therapy. Importantly, not all the survey population were initiating therapy; some had been on therapy for various lengths of time others were not on therapy at all.
Conclusions
This study shows that to have confidence in the therapy, get better skin quickly, and to be free of itching were among the top needs for patients with PsO. Understanding and meeting patient expectations for a therapy may improve treatment satisfaction, adherence, and long-term outcomes.
References
Feldman SR, Regnier SA, Chirilov A, et al. Patient-reported outcomes are important elements of psoriasis treatment decision making: a discrete choice experiment survey of dermatologists in the United States. J Am Acad Dermatol. 2019;80:1650–7.
Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70:512–6.
Gorelick J, Shrom D, Sikand K, et al. Understanding treatment preferences in patients with moderate to severe plaque psoriasis in the USA: results from a cross-sectional patient survey. Dermatol Ther (Heidelb). 2019;9:785–97.
Svoboda SA, Ghamrawi RI, Owusu DA, et al. Treatment goals in psoriasis: which outcomes matter most? Am J Clin Dermatol. 2020;21:505–11.
Lebwohl MG, Bachelez H, Barker J, et al. Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol. 2014;70:871-881.e871-830.
Ersser SJ, Surridge H, Wiles A. What criteria do patients use when judging the effectiveness of psoriasis management? J Eval Clin Pract. 2002;8:367–76.
Menter A, Strober BE, Kaplan DH, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80:1029–72.
Belinchón I, Rivera R, Blanch C, et al. Adherence, satisfaction and preferences for treatment in patients with psoriasis in the European Union: a systematic review of the literature. Patient Prefer Adherence. 2016;10:2357–67.
Bewley A, Burrage DM, Ersser SJ, et al. Identifying individual psychosocial and adherence support needs in patients with psoriasis: a multinational two-stage qualitative and quantitative study. J Eur Acad Dermatol Venereol. 2014;28:763–70.
Blome C, Gosau R, Radtke MA, et al. Patient-relevant treatment goals in psoriasis. Arch Dermatol Res. 2016;308:69–78.
Strober BE, van der Walt JM, Armstrong AW, et al. Clinical goals and barriers to effective psoriasis care. Dermatol Ther (Heidelb). 2019;9:5–18.
Kimball AB, Jacobson C, Weiss S, et al. The psychosocial burden of psoriasis. Am J Clin Dermatol. 2005;6:383–92.
Stern RS, Nijsten T, Feldman SR, et al. Psoriasis is common, carries a substantial burden even when not extensive, and is associated with widespread treatment dissatisfaction. J Investig Dermatol Symp Proc. 2004;9:136–9.
Feuerhahn J, Blome C, Radtke M, et al. Validation of the patient benefit index for the assessment of patient-relevant benefit in the treatment of psoriasis. Arch Dermatol Res. 2012;304:433–41.
Blome C, Augustin M, Behechtnejad J, et al. Dimensions of patient needs in dermatology: subscales of the patient benefit index. Arch Dermatol Res. 2011;303:11–7.
Augustin M, Radtke MA, Zschocke I, et al. The patient benefit index: a novel approach in patient-defined outcomes measurement for skin diseases. Arch Dermatol Res. 2009;301:561–71.
Blome C, Costanzo A, Dauden E, et al. Patient-relevant needs and treatment goals in nail psoriasis. Qual Life Res. 2016;25:1179–88.
Topp J, Augustin M, von Usslar K, et al. Measuring patient needs and benefits in dermatology using the patient benefit index 2.0: a validation study. Acta Derm Venereol. 2019;99:211–7.
Szepietowski JC, Reich A. Itch in psoriasis management. Curr Probl Dermatol. 2016;50:102–10.
Helmick CG, Lee-Han H, Hirsch SC, et al. Prevalence of psoriasis among adults in the U.S.: 2003–2006 and 2009–2010 National Health and Nutrition Examination Surveys. Am J Prev Med. 2014;47:37–45.
van Muijen ME, Atalay S, van Vugt LJ, et al. Unmet personal patient needs in psoriasis patients with low disease activity on adalimumab, etanercept or ustekinumab. Drugs Real World Outcomes. 2021;8:163–72.
Maul JT, Navarini AA, Sommer R, et al. Gender and age significantly determine patient needs and treatment goals in psoriasis—a lesson for practice. J Eur Acad Dermatol Venereol. 2019;33:700–8.
Pendzialek JB, Simic D, Stock S. Differences in price elasticities of demand for health insurance: a systematic review. Eur J Health Econ. 2016;17:5–21.
Böhm D, Stock Gissendanner S, Bangemann K, et al. Perceived relationships between severity of psoriasis symptoms, gender, stigmatization and quality of life. J Eur Acad Dermatol Venereol. 2013;27:220–6.
Radtke MA, Schäfer I, Blome C, et al. Patient benefit index (PBI) in the treatment of psoriasis—results of the National Care Study “PsoHealth.” Eur J Dermatol. 2013;23:212–7.
Cather JC. Psoriasis in children and women: addressing some special needs. Semin Cutan Med Surg. 2014;33:S42-44.
Menter A, Korman NJ, Elmets CA, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. Guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions. J Am Acad Dermatol. 2011;65:137–74.
Acknowledgements
Funding
Sponsorship for this study and Rapid Service Fee were funded by Eli Lilly and Company.
Medical Writing Support
Priyanka Bannikoppa, PhD, an employee of Eli Lilly Services India Pvt. Ltd., provided the writing support.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
April Armstrong, Emily Edson-Heredia, Baojin Zhu, Jeffery J. Crowley, Russel Burge, Stacy Smith contributed to interpretation of data and Stacy Smith, Emily Edson-Heredia, Jeffery J. Crowley were involved in analysis of data. Emily Edson-Heredia contributed to conception and acquisition of data. Emily Edson-Heredia and Russel Burge also contributed to design of the work. All the authors were involved in the critical revision of the manuscript and approved the final manuscript.
Prior Presentation
An earlier version of the data from this study was presented as poster at the American Academy of Dermatology (AAD); Denver, USA; 20–24 March 2020.
Disclosures
April Armstrong has been an investigator, and/or advisor, and/or speaker for: AbbVie, Celgene, Eli Lilly and Company, Janssen, Novartis, Regeneron, Sanofi, and Valeant. Emily Edson-Heredia, Baojin Zhu, and Russel Burge are employees and shareholders of Eli Lilly and Company. Stacie Bell is an employee of the National Psoriasis Foundation. Jeffery J. Crowley has received honoraria as a speaker and/or consultant for: AbbVie, Amgen, Celgene, Eli Lilly and Company, Janssen, Novartis, Pfizer, and Regeneron; and is an owner and employee of Bakersfield Dermatology, which has received research grant support from: AbbVie, Amgen, Celgene, Eli Lilly and Company, Janssen, Novartis, and Pfizer. Stacy Smith has performed clinical research studies for: AbbVie, Allergan, Boehringer Ingelheim, Brickell Biotech, Croma Pharma, Dermira, Eli Lilly and Company, Endo Pharmaceuticals, Evolus, Galderma, Glenmark Pharmaceuticals, Leo Pharma, Nielsen Biosciences, Novartis, Pfizer, Prollenium Medical Technologies, Revance Therapeutics, and Sun Pharmaceutical Industries; and has received fees and honoraria as a consultant from: Brickell Biotech, Galderma, Nielsen Biosciences, Prollenium Medical Technologies, Scarless Laboratories, and Teoxane.
Compliance with Ethics Guidelines
The study protocol was approved by the Genetic Alliance Institutional Review Board (protocol approval# NPF1801). This study was conducted in accordance with the Helsinki Declaration 1964, and its later amendments, Good Pharmacoepidemology Practices, and applicable laws and regulations of the USA. All patients provided informed consent for participation.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Armstrong, A., Edson-Heredia, E., Zhu, B. et al. Treatment Goals for Psoriasis as Measured by Patient Benefit Index: Results of a National Psoriasis Foundation Survey. Adv Ther 39, 2657–2667 (2022). https://doi.org/10.1007/s12325-022-02124-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02124-2