Abstract
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of mortality in Italy, accounting for 22% of total deaths. Lowering low-density lipoprotein cholesterol (LDL-C) levels reduces the risk of cardiovascular (CV) events; thus, lipid-lowering therapy (LLT) is the first-line treatment for patients with ASCVD and hypercholesterolaemia. However, many patients with ASCVD fail to reach LDL-C treatment thresholds, leaving them at greater risk of CV events. Inpatient care accounts for 51% of total expenditure on cardiovascular disease in the European Union, but healthcare resource utilization (HCRU) data for ASCVD in Italy is limited.
Methods
The study analysed healthcare claims data for 17,881 patients with acute coronary syndrome, ischemic stroke or peripheral artery disease from the Umbria 2 and Marche regions of Italy. LLT treatment patterns and CV event rates were collected and HCRU estimated in the year before and after the index event.
Results
High-intensity LLTs were prescribed to 44.3% of patients and 49.6% received moderate-/low-intensity LLTs during the 6 months after the index event. The first year CV event rate was 18.0/100 patient-years for patients receiving high-intensity LLTs and 17.2/100 patient-years for those on moderate-/low-intensity LLTs. Higher costs were associated with patients untreated with LLT 6 months post-index event (€8323) than patients prescribed high-intensity (€6278) or moderate-/low-intensity LLTs (€6270). Hospitalization accounted for most of the total costs.
Conclusions
This study found that CV events in secondary prevention Italian patients are associated with substantial HCRU and costs. More intensive LDL-C lowering can prevent CV events, easing the financial burden on the healthcare system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Many patients with ASCVD do not reach LDL-C treatment thresholds recommended by ESC/EAS guidelines, increasing their risk of future CV events and hospitalization, and placing a high economic burden on healthcare systems. |
This study analysed health resources utilization, LLT treatment patterns and CV event rates of patients with ASCVD in the Umbria 2 and Marche regions of Italy and may support payors and/or policymakers to make informed decisions on the availability and accessibility of treatment options for high-risk patients with ASCVD. |
Rates of hospitalization for CV events in patients with ASCVD are high and associated with significant costs. Intensification of LLT and the lowering of LDL-C levels may help prevent subsequent CV events and thus ease the economic burden on the Italian healthcare system. |
Introduction
Atherosclerosis, the leading cause of cardiovascular disease (CVD), is a serious health problem that can remain asymptomatic for many years and is associated with a poor prognosis and a reduction of life expectancy [1]. Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of mortality in Italy, with acute coronary syndrome (ACS) and ischemic stroke (IS) responsible for approximately 136,353 deaths annually, accounting for 22% of total deaths [2]. Patients with a history of myocardial infarction (MI), IS or peripheral artery disease (PAD) are at very high risk for a subsequent cardiovascular (CV) event, which is often more severe than the initial event, further increasing morbidity and mortality [3, 4]. Among survivors of ASCVD, 10% will experience another cardiovascular event within 1 year [5, 6] and 20% will experience another event within 4 years [7].
Low-density lipoprotein cholesterol (LDL-C) is a casual risk factor for ASCVD, and reductions in LDL-C are associated with a proportional reduction of the risk of cardiovascular events [8]. Thus, lipid-lowering therapy (LLT) plays a key role in secondary prevention in patients with ASCVD. Statin therapy is the first-line treatment for lowering LDL-C; however, many patients at very high risk of CV events do not meet the treatment goals set out in the current 2019 European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) guidelines for managing dyslipidemia (55 mg/dL (1.4 mmol/L) and at least a 50% reduction in LDL-C level from baseline) on statins alone [9]. The 2019 ESC/EAS guidelines recommend intensification of LLTs by adding ezetimibe or PCSK9 inhibitors in individuals who do not achieve their LDL-C goal on statin alone [10].
ACS, IS and severe cases of ASCVD such as unstable angina and transient ischemic attacks generally require hospitalization and are associated with substantial healthcare resource utilization (HCRU); inpatient care accounts for 51% of total expenditure on CVD in the European Union, amounting to €56 billion annually [7]. While inpatient care costs for Italy is estimated to be €7 billion annually [7], information on the HCRU associated with treatment of patients with ASCVD with LLTs in Italy is limited.
The aim of this study is to describe the ASCVD secondary prevention population in Italy, in terms of LLT treatment in the 6 months after the first cardiovascular hospitalization, CV event rate and cost of HCRU.
Methods
Data Sources
This study was based on the health information systems (HIS) data of the Marche region and Umbria Local Health Unit 2 (Umbria 2) of Italy (1.8 million inhabitants in the two regions). HIS routinely collects information on hospitalizations, drug prescriptions, outpatients care and laboratory tests for each patient registered in the Regional Health Care Assistance Registries (approximately 97% of residents). Each patient was identified in the HIS by an anonymous code that permitted deterministic linkage between the databases.
Under the rules of the Italian Drugs Agency (http://www.agenziafarmaco.gov.it/sites/default/files/det_20marzo2008.pdf), retrospective studies using administrative databases do not require ethics committee protocol approval.
Study Population
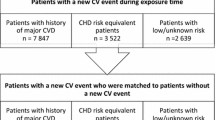
This retrospective cohort study included all patients aged 18–80 years with one or more hospitalizations for either ACS, IS/transient ischemic attack and/or PAD, discharged between 2009 and 2012 (for Marche region) or between 2011 and 2014 (for LHU Umbria 2), with at least two prescriptions of LLT (statins and/or ezetimibe) between 365 days before and/or in the 180 days after the first hospitalization for a CV event (index event). Patients were classified as either ACS, IS or PAD considering the first event to occur in the enrolment period.
The LLT treatment pattern for each patient was identified on the basis of the last drug prescription registered within the 6 months after the index event. LLT was classified on the basis of the 2013 American College of Cardiology and the American Heart Association guidelines for cholesterol treatment as follows (Table A, Supplemental Appendix) [11, 12]:
-
High-intensity LLT: atorvastatin (40–80 mg) or rosuvastatin (20–40 mg), with or without ezetimibe
-
Low- and moderate-intensity LLT: other statin regimens with or without ezetimibe monotherapy
-
Untreated with LLT 6 months post-index event: patients not receiving any LLT in the 6 months after the index event
For Umbria 2, the last LDL-C measurement available within 1 year after the index event was collected and used to determine a patient’s LDL-C level. LDL-C levels were not available from the Marche region. Three subgroups were defined: < 70 mg/dL (< 1.8 mmol/L), 70–100 mg/dL (1.8–2.6 mmol/L) and > 100 mg/dL (> 2.6 mmol/L) [10, 13].
Outcome and Healthcare Costs
Cardiovascular event rates at 1 year and 2 years were evaluated. CV event rates at 1-year and 2-year time periods were calculated on the basis of the occurrence of hospitalizations for subsequent CV events (ACS, IS, PAD, as identified using diagnosis-related groups [Table B, Supplemental Appendix]). Two-year CV event rates were calculated considering 730 days of follow-up and included patients who experienced a CV event in the first year of follow-up. Follow-up started on the day following the index event and ended at the first subsequent CV event or death. Patients were censored either at loss to follow-up, death or end of follow-up, whichever occurred first. HCRU were estimated for all enrolled patients and included hospitalizations, outpatient care and pharmaceutical prescriptions registered in the year before (baseline) and 1 year after the index event for all causes and for CV-related causes respectively. Costs were calculated using Italian National Health Service reimbursement tariffs; the results are expressed as the yearly average healthcare costs per patient [14].
Statistical Analyses
Descriptive analyses were undertaken. Categorical data were summarized using numbers and percentages, continuous data as mean and standard deviation (SD). The crude association between LLTs and LDL-C levels was tested using analysis of variance (ANOVA) test. All analyses were performed using SAS statistical package, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Patient Demographics and LLT Use
A total of 17,881 patients with a history of ACS (56.3%), IS (22.7%) or PAD (21.0%) were included; 71.5% were men and the mean age (SD) was 67 (± 9.8) years (Table 1).
Of the 1.8 million inhabitants of the Marche and Umbria 2 regions, the 17,881 patients identified here with history of ACS, MI or PAD represent a prevalence rate of 157.9 patients per 10,000 inhabitants. The prevalence rate for ACS was 76.7 patients per 10,000, 41.9 patients per 10,000 for IS and 39.4 per 10,000 for PAD. Overall, 44.3% of patients received high-intensity LLT (among them, 7893 patients (99.6%) were prescribed atorvastatin 40–80 mg or rosuvastatin 20–40 mg, 29 patients (0.4%) received combination treatment with ezetimibe), 49.6% received low- or moderate-intensity LLT (74 patients (0.8%) received ezetimibe monotherapy, 689 (7.8%) received fixed combination simvastatin/ezetimibe, while 8100 (91.4%) received other statin regimens), and 6.1% (a total of 1096 patients) were treated prior to the event and untreated with LLT during the first 6 months after the index event. The use of LLT was statistically significantly different between the three index event groups: high-intensity LLT treated patients were 60.9% for ACS, 29.7% for PAD and 16.5% for IS (p < 0.0001) (Table 1). Patients of the high-intensity LLT group were more likely to have other forms of ischemic heart disease compared with patients in the moderate-/low-intensity LLT and untreated with LLT 6 months post-index groups (63.5% compared with 43.6% and 37.0%, respectively) and more likely to have had previous coronary angioplasty (59.1% compared with 11.8% and 25.7%, respectively). Patients in the high-intensity LLT group were also more likely to be prescribed anti-thrombotic medications (89.1%) compared with moderate-/low-intensity LLT group (84.7%) and untreated with LLT 6 months post-index group (55.8%).
LDL-C Levels
A descriptive analysis of achieved LDL-C levels was performed in a subset of Umbria 2 patients with at least one LDL-C measurement available within 1 year from the index event (n = 811 [4.5% of the total study population]). Overall, 60.5% of patients failed to achieve an LDL-C level < 70 mg/dL (< 1.8 mmol/L) as recommended by the 2016 ESC/EAS guidelines that were in effect at the time of the study [13]: the proportion was significantly lower for high-intensity LLT treated patients (51.3%) compared with moderate-/low-intensity LLT and untreated with LLT 6 months post-index event (70.6% and 73.1%, respectively) (Table 2).
CV Event Rate
During the first year, CV event rate was estimated at 18.1 per 100 patient-years (PY) in patients untreated with LLT 6 months post-index event, 17.2 per 100 PY in patients receiving moderate-/low-intensity LLTs and 18.0 per 100 PY for those receiving high-intensity LLTs. The event rates were higher for patients with PAD (26.8, 28.8 and 27.8 per 100 PY, respectively), followed by ACS (16.4, 14.3 and 16.0 per 100 PY, respectively) and IS (12.9, 12.6 and 20.4 per 100 PY, respectively) (Fig. 1). The overall 2-year CV event rate was 12.5 per 100 PY for patients untreated with LLT 6 months post-index event, 11.8 per 100 PY for patients receiving moderate-/low-intensity LLT and 11.7 per 100 PY for those receiving high-intensity LLT (Fig. 1).
Health Resource Use
Overall, HCRU cost was estimated at €229.3 million: €114.8 million related to the index event and €114.5 million related to hospitalizations, drugs and specialist visits in the year after the index event. For patients treated with high-intensity LLTs the cost per patient per year was €13,678 (54.1% index event, 45.9% in the year following the index event), while patients treated with moderate-/low-intensity LLTs had a cost per year of €11,943 (47.5% index event, 52.5% in the year following the index event). Patients who did not receive treatment had a cost per year of €13,697; the cost incurred in the year following the index event represented a higher proportion of the total cost (60.7%) than in high-intensity LLT patients, attributed to greater hospitalization and outpatient care costs.
Baseline annual cost per patient was €6819 for patients untreated with LLT 6 months post-index event, €3349 for patients receiving moderate-/low-intensity LLTs and €2357 for patients receiving high-intensity LLTs. The economic impact due to the event could be estimated at €6273, €6278 and €8323 per patient in the first year for patients who received moderate-/low-intensity, high-intensity LLT and for those untreated with LLT 6 months post-index event, respectively. For patients with ACS and PAD treated with high-intensity LLT, baseline costs were lower (€2075 and €3285) than for those treated with moderate-/low-intensity LLT (€2885 and €4424). Conversely, for patients with IS the costs were higher for those receiving high-intensity LLT (€3385) than those receiving moderate-/low-intensity LLT (€3078) (Fig. 2). In patients with ACS treated with high-intensity LLTs, costs increased from baseline to 1-year post-index event by 362% and in those treated with moderate-/low-intensity LLT by 136%, but in patients with ACS untreated with LLT 6 months post-index event costs remained similar, with a slight decrease of 3.5%. This trend was less pronounced in patients with IS, with an 83.2% increase in costs observed for those treated with high-intensity LLT, a 40.1% increase in those treated with moderate-/low-intensity LLT and a decrease of 3.9% in patients with IS untreated with LLT 6 months post-index event. In patients with PAD, increases in costs were observed in all three groups; 108% in high-intensity, 66.1% in moderate-/low-intensity and 19.6% in untreated with LLT 6 months post-index event (Fig. 2). Similar trends were observed for CV-related costs, with costs in the year following the index event for patients with ACS treated with high-intensity LLTs increasing by 361%, in those treated with moderate-/low-intensity LLT by 228%, and in patients untreated with LLT 6 months post-index event by 70.5%. In patients with IS an 87.9% increase in costs observed for those treated with high-intensity LLT, a 47.1% increase in those treated with moderate-/low-intensity LLT and a decrease of 9.6% in untreated patients with IS. For PAD, costs for those treated with high-intensity LLTs, moderate-/low-intensity LLT or for patients untreated with LLT 6 months post-index event increased by 151%, 91.5% and 21.7%, respectively (Fig. 3).
Most of the total and CV related costs were related to hospitalizations, followed by pharmaceutical prescriptions and outpatient care. Both overall and CV-related costs increased in all patients in the first year after the index event. This was due to the cost of hospitalization for the index event and the high number of rehospitalizations within 1 year. Hospitalization accounted for a greater proportion of CV-related costs accrued for patients with PAD at baseline (54.3%) and in the first year after the index event (71.0%) than for patients with ACS (45.0% at baseline, 69.6% in the first year after the index event) and patients with IS (51.3% at baseline, 60.0% in the first year after the index event) (Fig. 4).
Discussion
In the present study carried out on a large population sample including 17,881 patients with ASCVD, we describe the treatment with LLT in the 6 months after the first CV hospitalization, estimate 1-year and 2-year CV event rate and annual costs of healthcare.
Overall, 44.3% of patients received high-intensity LLT, 49.6% received low- and moderate-intensity LLT, and 6.1% were untreated with LLT in the 6 months after the index event. These data are consistent with the literature: several studies have highlighted that a substantial proportion of patients at high risk for CV events, including patients with established CVD, receive suboptimal or no LLT [15,16,17,18,19]. The findings were also comparable to that of EUROASPIRE V, which found 50% of 7824 patients with coronary heart disease across 27 countries were receiving high-intensity LLT, with 34% receiving low- and moderate-intensity LLT; EUROASPIRE V also noted 16% of patients were untreated with LLT at time of interview, 6–24 months post-index event [20].
In our study, the rate of rehospitalization during the first year after the index CV event remains very high. This compares to an Italian retrospective observational study of three health units that found rehospitalization rate among patients at very high risk for CV events in the first year post-index was 38.2% [21].
Overall, patients with PAD had the highest CV event rate, followed by ACS and IS. By treatment, the highest CV event rate was reported in patients receiving high-intensity LLT; however, these patients also had more comorbidities, such as previous coronary angioplasty and other forms of ischemic heart disease and were more likely to be receiving anti-thrombotic medication at the time of the index event. These comorbidities may have contributed to their higher risk of CV events. Additionally, the higher costs associated with the index event for these patients (Fig. 2) indicate that these patients used more resources or more costly resources, which may be an indication that these patients were of worse clinical condition than patients on the moderate-/low-intensity LLT and untreated with LLT 6 months post-index groups.
Few existing studies have focused on the cost of CVD-related events over the first year for patients with hyperlipidemia or have examined the long-term costs associated with CVD-related events and stratified by specific event types. We found that patients with PAD had the highest annual cost, at €14,647, followed by ACS at €14,005, while the cost for patients with IS was substantially lower at €8178. These results are complementary to a study by Lucioni et al. [22] that assessed the clinical characteristics of patients in Italy in a community setting and reported on the clinical outcomes and the corresponding related costs of patients admitted for CV events. Lucioni et al. reported the annual cost for patients with ACS to be €14,871, with hospitalization accounting for 86.3% of the costs, although the report indicated that only short term (1-year) follow-up was considered to evaluate costs and no LDL-C data were provided because of the lack of linkage between databases and laboratory data. In addition, Marone et al. [23] and Fattore et al. [24] analysed costs considering a longer-term follow-up but both analyses focused only on a single specific patient cohort: patients with PAD and diabetes and patients with stroke, respectively. The cost for patients with PAD and stroke for the index event and 1 year following was €11,747, with costs relating to drugs accounting for €628, compared with €1202 reported here, which may reflect differences in the care of these two populations [24]. Real-world CV-event data in patients with PAD and diabetes and stroke are also limited in Italy with data available only for a 1-year follow-up [25].
In Italy, increased rates of morbidity and mortality have been associated with CVD, with the statistics indicating that the healthcare costs attributable to CVD accounted for 11% (€15.7 billion) of the total healthcare budget in 2015, with hospitalization identified as the main driver of the costs [7].
Our findings confirm that hospitalization is the major component of the total costs in treating patients with CVD regardless of the type of index CV event, accounting for 84.4% of total costs and 88.4% of CV-related costs in the first year after the index event. These data are consistent with other reports from Italy: a 2016 consensus study by Italian clinicians, representing all the key medical societies relevant to CVD management, showed that of the healthcare costs devoted to patients with ACS, 86.3% was spent on hospitalization [22]. This is reflected in the observation that the total number of hospital discharges in Italy for patients with ASCVD for 2017 was 439,887 [26]. Additionally, the leading cause of the hospitalizations was ACS, accounting for 131,973 events [26].
In keeping with the ESC/EAS guidelines, statins are the standard of care for treatment of hyperlipidemia in Italy. For patients at very high risk of CV events, if the treatment goal of < 55 mg/dL (1.4 mmol/L) and at least 50% reduction from baseline LDL-C level is not achieved on maximally tolerated statins, ezetimibe and PCSK9 inhibitors should be considered in addition to statin therapy [10]. In Italy, according to AIFA “Nota 13”, which defines statin reimbursement according to the level of CV risk, very high-risk patients are often treated with statins alone, and the addition of ezetimibe is considered only if the goal LDL-C levels (i.e. 70 mg/dL [1.8 mmol/L]) have not been achieved with the statin use [27]. The study found that most patients failed to achieve the target of LDL-C < 70 mg/dL (1.8 mmol/L) as set by “Nota 13”. Among patients on high-intensity LLT, 48.7% achieved the goal of LDL-C < 70 mg/dL (1.8 mmol/L) while a smaller proportion of patients on low- and moderate-intensity LLT (29.4%) achieved this target level. That less than 50% of very-high risk patients failed to achieve the “Nota 13” target of LDL-C < 70 mg/dL (1.8 mmol/L) represents a large unmet need in optimal LDL-C management. Importantly, with the current 2019 ESC/EAS guidelines [10] target of < 55 mg/dL (1.4 mmol/L) with a 50% reduction in LDL-C from baseline, the proportion of patients in the dataset who failed to achieve this more stringent target will be higher still.
Limitations
The analyses were based on administrative data sources which, by their very nature, were not designed to be used for epidemiological research, but only for accounting and billing. Therefore, this dataset only includes data considered important for accounting purposes and not necessarily includes data important for research. For instance, LDL-C data were only available for patients in the Umbria 2 region. However, the dataset from the Umbria region could be considered representative with respect to LDL-C measurements as the data presented here correlate well with results from other studies conducted in Italy (Table D, supplementary appendix). Additionally, to date, there are no specific epidemiological registries for measuring clinical outcomes and costs of patients with CVD in Italy; thus, administrative sources remain the best possible alternative for tracking patients’ HCRU within the Italian setting.
Secondly, the Marche and Umbria 2 regions account for 3.1% of the total population of Italy and so the results described here may not be representative of event rates for the entire country. However, the sample described in this study displays a comparable number of patients with ASCVD per 10,000 inhabitants as the rest of Italy (157.9 compared with 166.9 patients per 10,000), with similar numbers of patients with ACS (76.7 compared with 74.7 per 10,000), IS (41.9 compared with 43.0 per 10,000) and PAD (39.4 compared with 49.2 per 10,000) (Table D, supplementary appendix).
A third limitation of the study is the difficulty inherent in identifying patient-related clinical variables. This means that some misclassification may persist which will be linked to the severity of the disease and, more generally, to the clinical history of the patients in the analysis. However, the data gathering in these two regions is unlikely to be different when compared to the whole of Italy. Finally, another limitation regards estimates of patient mortality: the analysis referred only to in-hospital mortality, so it was impossible to identify deaths occurring outside the hospital environment, which could lead to an underestimation of patient mortality and event rates.
Conclusion
Rates of subsequent CV events in patients with ACS, IS and PAD are high. The cost of these events is substantial, both at the time of the event and for the first year after the event. Less than half of the patients at very high risk of CV events are on high-intensity statin therapy, resulting in more than 60% of these patients failing to achieve their LDL-C targets as recommended by Italian guidelines. An even higher proportion of patients would be considered uncontrolled according to the current ESC/EAS guidelines. Intensification of LLT and lowering of LDL-C levels below the treatment goals recommended by 2019 ESC/EAS guidelines will help prevent subsequent CV events and will ease the economic burden on the Italian healthcare system.
References
Roquer J, Ois A, Rodriguez-Campello A, et al. Atherosclerotic burden and early mortality in acute ischemic stroke. Arch Neurol. 2007;64(5):699–704.
European Commission. State of Health in the EU – Italy, Country Health Profile. https://www.euro.who.int/__data/assets/pdf_file/0008/355985/Health-Profile-Italy-Eng.pdf. Accessed Feb 2021.
Bhatt DL, Eagle KA, Ohman EM, et al. Comparative determinants of 4-year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA. 2010;304(12):1350–7.
Motivala AA, Tamhane U, Ramanath VS, et al. A prior myocardial infarction: how does it affect management and outcomes in recurrent acute coronary syndromes? Clin Cardiol. 2008;31(12):590–6.
Sulo G, Vollset SE, Nygard O, et al. Trends in acute myocardial infarction event rates and risk of recurrences after an incident event in Norway 1994 to 2009 (from a Cardiovascular Disease in Norway Project). Am J Cardiol. 2014;113(11):1777–81.
Mohan KM, Wolfe CD, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP. Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke. 2011;42(5):1489–94.
Wilkins E, Wilson L, Wickramasinghe K, et al. European cardiovascular disease statistics 2017. Brussels: European Heart Network; 2017.
Silverman MG, Ference BA, Im K, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316(12):1289–97.
Menzin J, Aggarwal J, Boatman B, et al. Ezetimibe use and LDL-C goal achievement: a retrospective database analysis of patients with clinical atherosclerotic cardiovascular disease or probable heterozygous familial hypercholesterolemia. J Manag Care Spec Pharm. 2017;23(12):1270–6.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J. 2020;41(1):111–88.
Danese MD, Gleeson M, Kutikova L, et al. Estimating the economic burden of cardiovascular events in patients receiving lipid-modifying therapy in the UK. BMJ Open. 2016;6(8):e011805.
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–934.
Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37(39):2999–3058.
Ministry of Health Decree. Remuneration for acute hospital care, post-acute hospital and long-term care and outpatient specialist care. 2012. https://www.gazzettaufficiale.it/eli/id/2013/01/28/13A00528/sg. Accessed Feb 2021.
Bittner V, Deng L, Rosenson RS, et al. Trends in the use of nonstatin lipid-lowering therapy among patients with coronary heart disease: a retrospective cohort study in the medicare population 2007 to 2011. J Am Coll Cardiol. 2015;66(17):1864–72.
Johansen ME, Green LA, Sen A, Kircher S, Richardson CR. Cardiovascular risk and statin use in the United States. Ann Fam Med. 2014;12(3):215–23.
Makam RC, Erskine N, McManus DD, et al. Decade-long trends (2001 to 2011) in the use of evidence-based medical therapies at the time of hospital discharge for patients surviving acute myocardial infarction. Am J Cardiol. 2016;118(12):1792–7.
Punekar RS, Fox KM, Richhariya A, et al. Burden of first and recurrent cardiovascular events among patients with hyperlipidemia. Clin Cardiol. 2015;38(8):483–91.
Verma A, Visintainer P, Elarabi M, Wartak S, Rothberg MB. Overtreatment and undertreatment of hyperlipidemia in the outpatient setting. South Med J. 2012;105(7):329–33.
Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol. 2019;26(8):824–35.
Esposti LD, Maggioni AP, Lap F, et al. Familial hypercholesterolemia and patients at very high cardiovascular risk: Real World Data analysis. GIHTAD 2016;9:2
Lucioni C, Mazzi S, Rossi E, et al. Therapeutic strategies and health costs of patients admitted for a cardiovascular event in Italy. Global Regional Health Technol Assess. 2016;3(2):GRHTA. 5000221.
Marone EM, Cozzolino P, Ciampichini R, et al. Peripheral arterial disease in diabetic patients: a long-term population-based study on occurrence, outcomes and cost. J Cardiovasc Surg (Torino). 2018;59(4):572–9.
Fattore G, Torbica A, Susi A, et al. The social and economic burden of stroke survivors in Italy: a prospective, incidence-based, multi-centre cost of illness study. BMC Neurol. 2012;14(12):137.
Perrone V, Sangiorgi D, Buda S, Degli EL. Residual cardiovascular risk in patients who received lipid-lowering treatment in a real-life setting: retrospective study. Clinicoecon Outcomes Res. 2016;8:649–55.
Agenzia Nazionale per i Servizi Sanitari Regionali. Programma Nazionale Esiti – PNE Edizione 2018. https://www.agenas.gov.it/images/agenas/In%20primo%20piano/PNE/2019/PNE2018_4_giugno.pdf. Accessed Feb 2021.
Italian Medicines Agency. Nota 13. https://www.aifa.gov.it/en/nota-13. Accessed Feb 2021.
Acknowledgements
Funding
This study was funded by Amgen (Europe) GmbH. The study sponsor is funding the journal’s Rapid Service fee.
Editorial/Medical Writing Assistance
The authors would like to thank Francesc Sorio Vilela (Amgen (Europe) GmbH) for contributions to the study design and analysis. Medical writing support (funded by Amgen (Europe) GmbH) was provided by Dan Smalley, PhD (Bioscript Medical Ltd, Macclesfield, UK).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
PS collected and analysed the data and wrote the manuscript. PS, APM, EA, ES, DAK and FSM critically revised the manuscript. All authors approved the final manuscript for submission.
Disclosures
Paolo Sciattella and Francesco S Mennini have no conflicts to declare. Aldo P Maggioni received personal fees for participating in study committees from Bayer, Fresenius, Novartis outside the present work. Emanuela Arcangeli is an employee of Amgen S.r.l. a socio unico. Eduard Sidelnikov and Doreen A Kahangire are full-time employees of Amgen (Europe) GmbH.
Compliance with Ethics Guidelines
Under the rules of the Italian Drugs Agency (http://www.agenziafarmaco.gov.it/sites/default/files/det_20marzo2008.pdf), retrospective studies using administrative databases do not require ethics committee protocol approval.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request and with permission of the Marche region and LHU Umbria 2.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sciattella, P., Maggioni, A.P., Arcangeli, E. et al. Healthcare Resource Utilization, Cardiovascular Event Rate and Use of Lipid-Lowering Therapies in Secondary Prevention of ASCVD in Hospitalized Patients in Italy. Adv Ther 39, 314–327 (2022). https://doi.org/10.1007/s12325-021-01960-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01960-y