Abstract
Introduction
Geographic access to novel oncology therapies, and the extent to which it may vary by potential sites of care, regions, and population characteristics, is poorly understood. We examined how expanding access to chimeric antigen receptor (CAR) T cell therapy administration sites impacts patient travel distances and time.
Methods
We used geographic information system techniques to calculate shortest travel distance and time between patients with relapsed/refractory diffuse large B cell lymphoma (DLBCL) and the nearest CAR T cell therapy administration site in three scenarios: academic hospitals; academic and community multispecialty hospitals; and academic and community multispecialty hospitals plus nonacademic specialty oncology network centers. Main outcome measures were differences in travel distance and time among the scenarios and the relationship between travel time and socioeconomic status, race, rural–urban areas, and non-Hodgkin lymphoma clusters. Non-Hodgkin lymphoma incidence, socioeconomic status, and administration centers were derived from governmental/publicly available data sources.
Results
Of 3922 patients eligible for CAR T cell therapy, more than 37% had to travel more than 1 h to the nearest academic hospital. Average travel time and distance were significantly reduced by 23% and 30% (P < 0.001), respectively, when access was expanded to include community hospitals plus a broader range of oncology specialty treatment centers. Compared to academic hospitals alone, increasing access to include community hospitals decreased time and distance by 7% and 8% (P < 0.01), respectively. In addition, there would be a lower proportion of sites operating as the only care provider within 25 miles if access was expanded outside of academic hospitals only. Longer travel time was associated with lower socioeconomic status.
Conclusion
Many patients with DLBCL have long travel times to an academic hospital that administers CAR T cell therapy. Expanding access to care through site-of-care planning will help address regional, rural–urban, and sociodemographic equity in the geographic allocation of CAR T cell therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Geographic access to novel oncology therapies, and the extent to which it may vary by sites of care, regions, and population characteristics, is poorly understood |
Our study assesses how expansion of chimeric antigen receptor (CAR) T cell therapy administration sites impacts patient accessibility in terms of travel distances and time |
We hypothesize that expansion of access to CAR T cell therapy administration sites can help to reduce the time and distance burden associated with traveling for CAR T cell therapy in the USA |
What was learned from this study? |
When access was expanded from academic hospitals to a broader network of specialty oncology treatment centers, average travel time and distance were significantly reduced by 23% and 30% (P < 0.001), respectively |
Many patients with diffuse large B cell lymphoma have long travel times to an academic hospital that administers CAR T cell therapy |
Our study indicates that site-of-care planning should address regional, rural–urban, and sociodemographic equity in the geographic allocation of CAR T cell therapy |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14815686.
Introduction
Travel distance and time are widely recognized factors impacting patients’ access to medical services and their willingness to receive treatment. Residing a long distance from health facilities decreases health service utilization [1,2,3]—a phenomenon known as the distance decay effect [4]. Extended travel distances to therapy or inconvenient care locations are barriers to patient care, particularly for those receiving later-line oncology therapy who may have poorer performance status. Travel can also greatly increase out-of-pocket therapy costs, making it unfeasible or burdensome for some patients to receive treatment [3, 5,6,7]. Consequently, longer travel distances may impose socioeconomic and clinical disparities on patients. Information regarding the accessibility of different treatment center types for various population subgroups is crucial for policy- and decision-making.
Chimeric antigen receptor (CAR) T cell therapies have shown promising results in the third-line setting among patients with the non-Hodgkin lymphoma (NHL) subtype diffuse large B cell lymphoma (DLBCL) [8, 9]. However, administration of CAR T cell therapy is currently limited to select cancer centers approved by manufacturers and independent institutions [10, 11]. Patients receiving approved CAR T cell therapies must be closely monitored for treatment-associated adverse events, including cytokine release syndrome (CRS) and neurological events (NEs), and must remain within 0.5–2 h of the treatment site for at least 4 weeks after infusion [12,13,14]. During this time, a caregiver is also needed to monitor symptoms. These requirements, along with the limited number of treatment sites, impose a travel burden that could limit many patients’ access to this therapy if its administration is restricted to academic hospital settings. To our knowledge, little is known regarding geographic access to CAR T cell therapy and the extent to which it may vary by potential sites of care, regions, and population characteristics. The objective of this study was to estimate the extent to which expanding access to different CAR T cell therapy administration sites impacts patient travel distances and time in the continental United States (US).
Methods
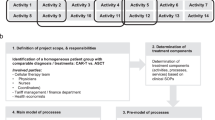
Data Sources
County-level NHL incidence counts of patients were matched to the nearest (“as the crow flies”) potential CAR T cell therapy administration center to analyze variations in travel requirements (in miles and minutes) by site scenario. CAR T cell therapy administration sites included centers with relevant claims activity indicating CAR T cell administration capability and phase 1 oncology clinical trial sponsorship, along with centers approved for administration of currently marketed CAR T cell products. All centers were geocoded in R software (version 3.5.3 [2019-03-11]; R Graphical User Interface system for Windows) [15].
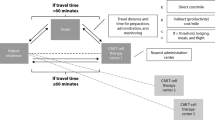
Our analysis considered three types of CAR T cell therapy facilities: academic hospitals, community multispecialty hospitals, and nonacademic specialty oncology network centers (NASONCs) (Fig. S1). Sites were categorized on the basis of publicly available information obtained from facility websites (Table 1) [16,17,18,19,20,21,22,23]. The facilities that administered CAR T cell therapy were classified by certain sites of care type as follows: academic hospitals, community multispecialty hospitals, or NASONCs (Table S1).
The three hypothetical scenarios analyzed were increasingly inclusive of site type and included treatment at (A) academic hospitals only; (B) both academic and community multispecialty hospitals; and (C) any specialized center that included approved inpatient or possible outpatient CAR T cell therapy (academic hospitals, community multispecialty hospitals, and NASONCs) (Table 1). Each patient was assumed to be treated at the nearest center. We used geographic information system techniques for this analysis.
This article does not contain any new studies with human participants or animals performed by any of the authors.
Patient and CAR T Cell Therapy Location and Characteristics
Patients were assigned to US counties with a corresponding US census tract region, level of urbanization, race/ethnicity distribution, and federal poverty level (FPL) based on NHL incidence data from State Cancer Profiles—a data program developed by the National Cancer Institute (NCI) and Centers for Disease Control and Prevention (CDC). Incidence data were extracted from the CDC’s National Program of Cancer Registries Cancer Surveillance System and the NCI’s Surveillance, Epidemiology, and End Results (SEER) Program. These data represented a 5-year average incidence count from 2011 to 2015 for every county except those in Kansas, Minnesota, and Nevada, as incidence data were not supplied to SEER from these states. Data from Alaska and Hawaii were excluded from analysis because these states had inconsistent road-based travel. The analysis was limited to counties with at least one incident NHL case, on average, from 2011 to 2015. Among counties with available data, limited information was provided in certain Wyoming and Colorado counties because of low NHL incidence or lack of sufficient data.
This analysis used the latest 5-year average (2011–2015) of county-level cancer incidence rate of NHL for all stages, all races (including Hispanic), both sexes, and all ages. Rates were reported as cases per 100,000 population per year; these rates were age adjusted to the 2000 US standard population. In many cases, the CDC suppressed county-level incidence data because of low annual rates. For this analysis, the suppressed county rates were imputed to 1 case per 100,000. The county-level incidence count of patients with DLBCL was estimated as a uniform percentage (32.5%) of patients with NHL based on published literature that analyzed data from the National Cancer Database [24]. Patients with DLBCL receiving third-line therapy (19.4%) and who were eligible for CAR T cell therapy [12, 13] were estimated on the basis of published findings on response by line of therapy [25,26,27]. To protect patient confidentiality, county-level geographic details on NHL incidence excluded patient demographics. Accordingly, the incidence data do not contain demographic characteristics of the cases. Thus, separate data on county-level socioeconomic status variables from the US Census Bureau 2011–2015 American Community Survey 5-Year Estimates were linked to the county-level incidence data. Socioeconomic data included county-level information on sex, race/ethnicity, and number of persons above and below the FPL.
Patients’ residences were assumed to be at the county population centroid. The centroids were geocoded into latitude and longitude coordinates [28]. For each US county, the number of NHL cases and total county population for the year 2015 were recorded and uploaded to SaTScan (version 9.6; Kulldorff M and Information Management Services, Inc.) and R software. Consistent with payment classification specified by the Centers for Medicare and Medicaid Services, we classified any patient residing within a core-based statistical area (included metropolitan and micropolitan areas) as urban and any patient residing outside of a core-based statistical area as rural [29, 30].
Geographic Access Measures
Travel distance and times were calculated on the basis of the shortest driving route from each county population center to the nearest destination point (academic hospital, community multispecialty hospital, or NASONC) based on a national major and minor road network with associated speed limits and average traffic time (Google’s Distance Matrix API) [15]. We computed travel distance and time using a nearest-neighbor algorithm developed in R. Demographic and rural–urban data were then linked to the county travel distance and times for the three CAR T cell therapy settings (academic hospital, community multispecialty hospital, or NASONC) to evaluate implications across socioeconomic variables.
Travel to a CAR T cell therapy center was defined as the driving distance (miles) and estimated time (minutes; assuming average traffic conditions in the areas) between the geographic center of the patient’s residence and the CAR T cell therapy center. Travel distance was categorized, on the basis of literature [31,32,33], as 0–12.49, 12.5–49.9, 50–149.9, 150–249.9, and ≥ 250 miles. Travel time was categorized, on the basis of literature and guidelines [14, 32, 34, 35], as 0–30, 31–60, 61–120, 121–300, and > 300 min. Travel time categories were mapped and summarized in R.
Statistical Analysis
Descriptive analyses were used to investigate the distribution of potential CAR T cell administration sites by each scenario’s type of center and by independent variables (race/ethnicity, FPL, and rural–urban). The number of sites by region, rural–urban residencies, and type are shown in Table S2. The base case assumed that patients could only attend academic hospitals (scenario A). This case was compared with the incremental addition of community multispecialty hospitals to academic hospitals (scenario B) and then with the addition of NASONCs (scenario C). Analysis of the differences in the weighted mean travel distance and time was performed using the t test after testing for equality of variance. Differences in the proportions of sole providers (“monopoly” providers) were tested using the independent z test. Means were weighted by the estimated number of patients with DLBCL in the county. To explore statistical associations between distance and time and sociodemographic characteristics, we conducted nonparametric tests for bivariate correlation using Spearman correlation coefficients. In all statistical tests, P < 0.05 was considered statistically significant. All statistical analyses were performed with R.
Cluster Analysis
A geographic cancer cluster is defined as “a greater-than-expected number of cancer cases that occurs within a group of people in a defined geographic area over a period of time” [36]. In this study, SaTScan was used for NHL cluster identification and significance testing. NHL incidence (vs DLBCL incidence) was used for accuracy in the cluster analysis as a result of county-level data availability. The results for patients with DLBCL were assumed to be representative if these patients had similar geographical distribution to patients with NHL. NHL incidence in each county was assumed to be distributed according to a Poisson model, which tests the null hypothesis that the age‐adjusted risk of NHL incidence is the same for all counties in the data set. We then compared the top five clusters to the number of available sites to evaluate treatment accessibility for high-density areas with patients with NHL. Lack of overlap would suggest a geographic access disparity in counties that may need it most.
Results
Patients
The analysis included NHL incidence data (2011–2015) from all evaluable states. From these data, 62,339 unique cases of NHL were identified. Patients with DLBCL receiving third-line therapy were estimated to comprise 3922 (6.3%) of the identified patients with NHL [26, 27, 37].
Travel Distance and Time
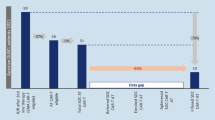
A shift toward shorter travel distance and time occurred as the scenarios progressed through expanding inclusion of site types. Maps of travel distance by site type and travel time and distance by type of potential CAR T cell therapy site scenario are presented in Fig. 1. Weighted mean travel distance and time traveled, respectively, were significantly shorter to academic and community multispecialty hospitals for scenario B (54.8 miles and 61.0 min) and were further reduced under scenario C (any specialized treatment center; 41.9 miles and 50.7 min) compared with scenario A (academic hospitals only; 59.7 miles and 65.8 min) (Table 2). For scenario C versus scenario A, this reflected a reduced average travel time and distance of 23% and 30%, respectively. Significance was maintained for travel time between scenarios A and C when stratified by all regions and rural–urban classification; travel distance remained significantly shorter for scenario C versus scenario A when stratified by rural–urban classification and in all regions except the northeast. Numerical improvements were observed between scenarios A and B when stratified by all regions and rural–urban classification; however, statistical significance for both time and distance was seen for only the south region and urban areas. The south region had the longest estimated mean travel distance (71.9 miles) and time (76.3 min) under scenario A but was reduced to 61.9 miles and 66.8 min (P < 0.001), respectively, under scenario B (academic and community multispecialty hospitals) and to 46.7 miles and 53.1 min (P < 0.001), respectively, under scenario C (any specialized treatment center). Travel distance for urban areas was 51.0 miles under scenario A versus 34.5 miles under scenario C, and travel time was 57.2 min and 41.3 min, respectively (P < 0.001 for both); results were not statistically significant for scenario A versus scenario B.
In scenario A, approximately 60% of potential patients resided less than 50 miles (Fig. 2a) from an academic hospital, and 36%, 63%, and 84% lived within 30 min, 1 h, and 2 h, respectively (Fig. 2b). In scenario B, approximately 64% of patients resided less than 50 miles from the nearest treatment center (P = not significant), and 40%, 67%, and 87% lived within 30 min, 1 h, and 2 h, respectively. In scenario C, approximately 71% of patients resided less than 50 miles from the nearest treatment center (P < 0.001), and 46%, 74%, and 92% lived within 30 min, 1 h, and 2 h, respectively. About 15% of patients would have to travel more than 2 h to the nearest academic hospital in scenario A, whereas 13% and 8% of patients would have to travel more than 2 h in scenarios B and C, respectively.
Number of the diffuse large B cell lymphoma incident population (N = 3922) stratified by site type and a travel distance and b travel time to nearest chimeric antigen receptor (CAR) T cell therapy administration center. aScenario A: academic hospitals only. bScenario B: both academic and community multispecialty hospitals. cScenario C: any specialized center that included approved inpatient or possible outpatient CAR T cell therapy (academic hospitals, community multispecialty hospitals, and nonacademic specialty oncology network centers). mi miles, min minutes
Travel Time, Socioeconomic Status, and Race/Ethnicity
Differences in distance and travel time across the scenarios were apparent for FPL and rural–urban measures (Table 3; Fig. 3). An estimated 42% of patients living below 100% FPL resided at least 50 miles from the nearest academic hospital (scenario A), compared with 39% for academic and community multispecialty hospitals (scenario B) and 31% for any specialized treatment center (scenario C) (both P < 0.001; Table 3). Similarly, 64% of patients living below 100% FPL would travel more than 30 min to an academic site, compared with 61% and 55% for academic and community multispecialty hospitals and any specialized treatment center (both P < 0.001), respectively. A significantly (P < 0.01) lower proportion of sites would be the sole care providers for patients (the only provider within 25 miles) if all sites were included compared with academic hospitals only (27% vs 41%, respectively); results were not statistically significant for scenario B (Table 2). Travel distance and time were shorter among both rural and urban areas in scenario C than in scenario A (Fig. 3).
The bivariate analysis of the association between travel time, socioeconomic status, and race/ethnicity showed that longer travel times were significantly (P < 0.001) associated with higher poverty rates and particular races/ethnicities (Table S3). Spearman correlation coefficients indicated statistically significant and positive linear associations between time to the nearest CAR T cell therapy site and the percentage of patients living below the FPL, as well as the proportions of Native American and non-Hispanic Whites; for race/ethnicity, the proportion of Native Americans showed the strongest positive correlation (Table S3).
Cluster Analysis
The spatial scan identified five areas where observed NHL incidence was significantly greater than the number expected from the distribution in the remaining US areas after adjusting for age (Fig. 1). A heightened need for therapy is expected in these clusters. The cluster analysis revealed a stronger positive correlation between the number of CAR T cell administration sites and NHL patient counts for any specialized treatment center (scenario C) compared with academic hospitals only (scenario A) (Fig. S2).
Discussion
This geospatial analysis showed that increasing the number of administration center options for CAR T cell therapy led to a greater number of patients with shorter travel distance and time to a treatment site. About 74% of patients with DLBCL lived within a travel time of less than 1 h to any specialized treatment center in scenario C compared with only 63% of patients in scenario A, where treatment was limited to the nearest academic hospital. This difference is notable, as CAR T cell therapy requires patients to remain within 0.5–2 h of the site of care for at least 4 weeks after infusion for CRS and NE monitoring [12, 13]. Patients unable to live at home during this monitoring period would need to find lodging near the site of care, making the treatment more costly for patients and caregivers. Travel burden—in terms of distance, time, and costs—is an important factor in access to care. This analysis examines patient access to CAR T cell therapy and reflects on access to future novel oncology therapies.
The results presented here suggest that patients may benefit from administration of CAR T cell therapy in the outpatient setting, as it would allow for more sites to be able to administer CAR T cell therapy. Recent studies have shown that outpatient treatment with CAR T cell therapy is possible with an acceptable safety profile [38]. Because fever is the first presenting symptom of CRS, it has been argued that CAR T cell therapy can be safely administered in the outpatient setting if patients are carefully monitored, with hospital admittance at the time of fever development [39]. Many clinics have the infrastructure and multidisciplinary teams in place to support outpatient stem cell and bone marrow transplant programs [40]. Additionally, differences in safety profiles between CAR T cell therapies and in individual patient risk factors may allow for identification of those patients who can safely be administered CAR T cell therapy at nonacademic centers. Nevertheless, any clinic tasked with administering CAR T cell therapy should be prepared to manage the complexity of administering this therapy and its potential associated adverse effects.
Access to a greater number of qualified administering locations is particularly important for certain geographic areas. In NHL cluster areas, the number of potential administration sites increased under scenario C, resulting in greater proximity to CAR T cell therapy administration sites. In bivariate analyses, patients of Native American race/ethnicity, those living in rural areas, and those with low socioeconomic status had relatively long travel times to CAR T cell therapy administration sites. These findings align with previous studies showing that these groups traveled longer distances to receive care and that longer travel distances were associated with additional patient time burden, cost, and discomfort levels [3, 41,42,43,44]. Moreover, lower income has been associated with a reduced likelihood of traveling long distances for therapy [45], potentially decreasing patients’ access to appropriate cancer care.
The association between regions and socioeconomic variables with estimated travel distances and times is also concerning, as some health plans may restrict patients’ hospital choice. Patients with these plans may need to travel farther from home despite having critical medical conditions and limited resources. Policy- and decision-makers should consider evaluating the geospatial accessibility of CAR T cell therapy administration and monitoring, along with its impact on patients’ care and quality of life.
This study has several strengths and limitations. By developing a detailed geographic information systems database of NHL incidence combined with a specific site of care, we estimated more precise measures of access to novel oncology therapies than those previously described [31,32,33]. A limitation of this study is that disease incidence was based on county-level NHL patient incidence counts as of 2015. Also, the database from which CAR T cell therapy site locations were extracted is frequently updated. Patients may also be required to travel to a specific site according to provider networks and local oncologist referrals. While this study did not incorporate these possibilities, we analyzed the most optimistic circumstances in that patients were assumed to travel to the nearest location administering CAR T cell therapy.
Actual patient addresses or DLBCL incidence by ZIP code would have refined this analysis; however, these data were not publicly available because of patient confidentiality. Therefore, we were unable to analyze distances traveled by patients living along county borders who may have been closer to potential CAR T cell therapy administration sites than estimated by using the county centroid. However, comparisons across site-of-care scenarios are unlikely to be considerably impacted by increased precision in patient residence data. Additionally, some counties were excluded from the analysis because of insufficient incidence data.
The impact of distance and time on patients’ ability to receive therapy may be mitigated by other factors not included in our study, such as the patient–physician relationship, patient preference, physician networks, and patient health status [46, 47]. Further, our study did not address capacity by geographic region, an area of potential concern if NHL and CAR T cell therapy center clusters do not overlap.
It is also critical to note that there are additional costs required to expand CAR T cell therapy to nonacademic hospitals and treatment settings to meet requirements consistent with the Foundation for the Accreditation of Cellular Therapy (FACT) [48, 49]. The CAR T cell therapy process has many steps, including leukapheresis or lymphocyte collection, transportation of the collected cells to a laboratory, cell engineering, patient conditioning or lymphodepleting chemotherapy, infusion, and patient monitoring and follow-up that must not be compromised in order to properly care for patients during and after CAR T cell therapy. Furthermore, investment costs will also require providers in the CAR T cell therapy unit to focus on education. Inpatient units are more likely to have FACT accreditation at the time they establish a CAR T cell therapy program [49], and outpatient facilities must also coordinate with inpatient providers for possible admission to manage adverse events [48]. In this study, the few patients requiring these procedures could potentially affect expansion of CAR T cell therapy to nonacademic hospitals and treatment settings.
The absence of sociodemographic and clinical detail, along with imprecise key patient characteristics, is an inherent limitation of public incidence databases, making association with outcomes unfeasible. As a descriptive study, this research did not attempt to draw causal inferences between geographic access and patient outcomes or receipt of treatment; however, it provides the foundation for this next logical step. Finally, with recent approval of CAR T cell therapies, such as idecabtagene vicleucel, for multiple myeloma, we believe that these study findings have implications outside of DLBCL, and further investigation of access to therapy is warranted. While this study did not include all patient indications for current and future CAR T cell therapies, it provides the basis for such research to be conducted in the future.
Conclusion
Our research indicates that patient access to therapy may be limited on the basis of geographic location. Patients with DLBCL who live more than 25 miles from an academic hospital may not have access to the same treatment options as those who live closer. Expanding CAR T cell therapy to nonacademic hospitals and outpatient treatment centers could make this therapy accessible to a broader patient population.
References
Kelly C, Hulme C, Farragher T, Clarke G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open. 2016;6(11):e013059. https://doi.org/10.1136/bmjopen-2016-013059.
Su D, Pratt W, Salinas J, Wong R, Pagan JA. Rural-urban differences in health services utilization in the US-Mexico border region. J Rural Health. 2013;29(2):215–23. https://doi.org/10.1111/j.1748-0361.2012.00445.x.
Friedman SA, Frayne SM, Berg E, et al. Travel time and attrition from VHA care among women veterans: how far is too far? Med Care. 2015;53(4 suppl 1):S15–22. https://doi.org/10.1097/MLR.0000000000000296.
Pun-Cheng LSC. Distance decay. In: Richardson D, Castree N, Goodchild MF, Kobayashi A, Liu W, Marston RA, editors. International encyclopedia of geography: people, the earth, environment and technology. Hoboken: Wiley; 2016. p. 1–5.
Chari A, Romanus D, DasMahapatra P, et al. Patient-reported factors in treatment satisfaction in patients with relapsed/refractory multiple myeloma (RRMM). Oncologist. 2019;24(11):1479–87. https://doi.org/10.1634/theoncologist.2018-0724.
Javid SH, Unger JM, Gralow JR, et al. A prospective analysis of the influence of older age on physician and patient decision-making when considering enrollment in breast cancer clinical trials (SWOG S0316). Oncologist. 2012;17(9):1180–90. https://doi.org/10.1634/theoncologist.2011-0384.
Patel M, Periyakoil V, Douglas W, et al. Redesigning cancer care delivery: views from patients and caregivers. J Oncol Pract. 2017;13(4):e291–302. https://doi.org/10.1200/jop.2016.017327.
Schuster SJ, Bishop MR, Tam CS, et al. Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2019;380(1):45–56. https://doi.org/10.1056/NEJMoa1804980.
Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377(26):2531–44. https://doi.org/10.1056/NEJMoa1707447.
Novartis Pharmaceuticals Corporation. KYMRIAH risk evaluation and mitigation strategy. 2019. https://www.kymriah-rems.com/. Accessed 10 Sep 2019.
Kite Pharma. YESCARTA risk evaluation and mitigation strategy (REMS). 2020 https://www.yescartarems.com/. Accessed 10 Sep 2019.
Novartis Pharmaceuticals Corporation. KYMRIAH (tisagenlecleucel) prescribing information. 2018. https://www.novartis.us/sites/www.novartis.us/files/kymriah.pdf. Accessed 9 Mar 2019.
Kite Pharma. YESCARTA (axicabtagene ciloleucel) prescribing information. 2019. https://www.gilead.com/-/media/files/pdfs/medicines/oncology/yescarta/yescarta-pi.pdf. Accessed 9 Mar 2019.
Mayo Clinic. CAR-T cell therapy program - frequently asked questions. 2019. https://www.mayoclinic.org/departments-centers/car-t-cell-therapy-program/sections/gnc-20405547. Accessed 16 Dec 2019.
Kahle D, Wickham H. ggmap: spatial visualization with ggplot2. R J. 2013;5(1):144–61.
Centers for Medicare & Medicaid Services. Glossary and acronyms. 2016. https://www.cms.gov/OpenPayments/About/Glossary-and-Acronyms.html#teachinghospital. Accessed 12 Aug 2019.
Centers for Medicare & Medicaid Services. 2019 reporting cycle: teaching hospital list. 2018. https://www.cms.gov/OpenPayments/Downloads/2019-Reporting-Cycle-Teaching-Hospital-List-pdf.pdf. Accessed 31 July 2019.
Kite Pharma. Where can YESCARTA be received? 2019. https://www.yescarta.com/treatment-centers. Accessed 31 Jan 2020.
Novartis Pharmaceuticals Corporation. Find a KYMRIAH treatment center. 2020. https://www.us.kymriah.com/treatment-center-locator/. Accessed 12 July 2021.
American Hospital Association. Fast facts on US hospitals. 2019. https://www.aha.org/statistics/fast-facts-us-hospitals. Accessed 12 Aug 2019.
National Cancer Institute. Find a cancer center. 2020. https://www.cancer.gov/research/nci-role/cancer-centers/find. Accessed 31 Jan 2020.
Centers for Medicare & Medicaid Services. Oncology care model practice list. 2020. https://innovation.cms.gov/initiatives/Oncology-Care/. Accessed 31 Jan 2020.
Association of Community Cancer Centers. Find a cancer program. 2020. https://www.accc-cancer.org/. Accessed 31 Jan 2020.
Al-Hamadani M, Habermann TM, Cerhan JR, Macon WR, Maurer MJ, Go RS. Non-Hodgkin lymphoma subtype distribution, geodemographic patterns, and survival in the US: a longitudinal analysis of the National Cancer Data Base from 1998 to 2011. Am J Hematol. 2015;90(9):790–5.
Gisselbrecht C, Glass B, Mounier N, et al. Salvage regimens with autologous transplantation for relapsed large B-cell lymphoma in the rituximab era. J Clin Oncol. 2010;28(27):4184–90. https://doi.org/10.1200/JCO.2010.28.1618.
Rovira J, Valera A, Colomo L, et al. Prognosis of patients with diffuse large B cell lymphoma not reaching complete response or relapsing after frontline chemotherapy or immunochemotherapy. Ann Hematol. 2015;94(5):803–12. https://doi.org/10.1007/s00277-014-2271-1.
Van Den Neste E, Schmitz N, Mounier N, et al. Outcomes of diffuse large B-cell lymphoma patients relapsing after autologous stem cell transplantation: an analysis of patients included in the CORAL study. Bone Marrow Transplant. 2017;52(2):216–21. https://doi.org/10.1038/bmt.2016.213.
US Census Bureau. Geographies. 2019. https://www.census.gov/geographies/reference-files/time-series/geo/centers-population.html. Accessed 11 Sep 2019.
Centers for Medicare & Medicaid Services. Rural-urban disparities in health care in medicare. 2018. https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/Rural-Urban-Disparities-in-Health-Care-in-Medicare-Report.pdf. Accessed July 31 2019.
National Bureau of Economic Research. CMS's SSA to FIPS CBSA and MSA county crosswalk (2017). https://www.nber.org/research/data/ssa-federal-information-processing-series-fips-core-based-statistical-area-cbsa-and-metropolitan-and. Accessed May 28 2019.
Massarweh NN, Chiang YJ, Xing Y, et al. Association between travel distance and metastatic disease at diagnosis among patients with colon cancer. J Clin Oncol. 2014;32(9):942–8. https://doi.org/10.1200/JCO.2013.52.3845.
Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D. Geographic access to cancer care in the U.S. Cancer. 2008;112(4):909–18. https://doi.org/10.1002/cncr.23229.
Wang EH, Mougalian SS, Soulos PR, et al. Adoption of hypofractionated whole-breast irradiation for early-stage breast cancer: a National Cancer Data Base analysis. Int J Radiat Oncol Biol Phys. 2014;90(5):993–1000. https://doi.org/10.1016/j.ijrobp.2014.06.038.
Onega T, Cook A, Kirlin B, et al. The influence of travel time on breast cancer characteristics, receipt of primary therapy, and surveillance mammography. Breast Cancer Res Treat. 2011;129(1):269–75. https://doi.org/10.1007/s10549-011-1549-4.
University of Iowa Hospitals and Clinics. CAR T-cell therapy. 2019. https://uihc.org/health-topics/car-t-cell-therapy. Accessed 28 May 2019.
Centers for Disease Control and Prevention. Cancer clusters. 2019. https://www.cdc.gov/nceh/clusters/default.htm. Accessed 28 May 2019.
Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence - SEER 9 Regs Research Data, Nov 2018 Sub (1975–2016) <Katrina/Rita Population Adjustment>. 2019. www.seer.cancer.gov. Accessed 28 May 2019.
Bachier CR, Palomba ML, Abramson JS, et al. Outpatient treatment with lisocabtagene maraleucel (liso-cel) in three ongoing clinical studies in relapsed/refractory (R/R) B cell non-Hodgkin lymphoma (NHL), including second-line transplant ineligible patients: TRANSCEND NHL 001, Outreach, and PILOT. Blood. 2019;134(suppl 1):2868. https://doi.org/10.1182/blood-2019-127566.
Teachey DT, Bishop MR, Maloney DG, Grupp SA. Toxicity management after chimeric antigen receptor T cell therapy: one size does not fit “ALL.” Nat Rev Clin Oncol. 2018;15(4):218. https://doi.org/10.1038/nrclinonc.2018.19.
Smith S, Essell J. Evolving the delivery of CAR T-cell therapies to the outpatient setting. J Clin Pathw. 2018;4(8):42–7. https://doi.org/10.25270/jcp.2018.10.00039.
Baldwin LM, Cai Y, Larson EH, et al. Access to cancer services for rural colorectal cancer patients. J Rural Health. 2008;24(4):390–9. https://doi.org/10.1111/j.1748-0361.2008.00186.x.
Onega T, Alford-Teaster J, Wang F. Population-based geographic access to parent and satellite National Cancer Institute Cancer Center Facilities. Cancer. 2017;123(17):3305–11. https://doi.org/10.1002/cncr.30727.
Vetterlein MW, Loppenberg B, Karabon P, et al. Impact of travel distance to the treatment facility on overall mortality in US patients with prostate cancer. Cancer. 2017;123(17):3241–52. https://doi.org/10.1002/cncr.30744.
Xu Y, Fu C, Onega T, Shi X, Wang F. Disparities in geographic accessibility of National Cancer Institute Cancer Centers in the United States. J Med Syst. 2017;41(12):203. https://doi.org/10.1007/s10916-017-0850-0.
Graboyes EM, Ellis MA, Li H, Kaczmar JM, et al. Racial and ethnic disparities in travel for head and neck cancer treatment and the impact of travel distance on survival. Cancer. 2018;124(15):3181–91. https://doi.org/10.1002/cncr.31571.
Chan L, Hart LG, Goodman DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health. 2006;22(2):140–6. https://doi.org/10.1111/j.1748-0361.2006.00022.x.
Tai WT, Porell FW, Adams EK. Hospital choice of rural Medicare beneficiaries: patient, hospital attributes, and the patient-physician relationship. Health Serv Res. 2004;39(6 pt 1):1903–22. https://doi.org/10.1111/j.1475-6773.2004.00324.x.
Perica K, Curran KJ, Brentjens RJ, Giralt SA. Building a CAR garage: preparing for the delivery of commercial CAR T cell products at Memorial Sloan Kettering Cancer Center. Biol Blood Marrow Transplant. 2018;24(6):1135–41. https://doi.org/10.1016/j.bbmt.2018.02.018.
Taylor L, Rodriguez ES, Reese A, Anderson K. Building a program: implications for infrastructure, nursing education, and training for CAR T-cell therapy. Clin J Oncol Nurs. 2019;23(2):20–6. https://doi.org/10.1188/19.CJON.S1.20-26.
Acknowledgements
Funding
This study was funded by Bristol Myers Squibb. The study sponsor is also funding the journal’s Rapid Service and Open Access fees.
Medical Writing and Editorial Assistance
Medical writing, graphics, and editorial support were provided by Sheridan Henness, PhD, and Edwin Thrower, PhD, of The Lockwood Group (Stamford, CT), funded by Bristol Myers Squibb.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors had full access to the data in the study and take responsibility for the integrity of the data, the relevance of the methodology, and the accuracy of the data analysis. Sophie Snyder, Karen C. Chung, Monika P. Jun, and Matthew Gitlin were involved in study conception and design. Sophie Snyder, Karen C. Chung, and Monika P. Jun were responsible for collection and assembly of data. Sophie Snyder, Karen C. Chung, Monika P. Jun, and Matthew Gitlin carried out data analysis and interpretation. Sophie Snyder, Karen C. Chung, Monika P. Jun, and Matthew Gitlin were involved in writing the manuscript. All authors approved of the manuscript and were accountable for all aspects of the work.
Disclosures
Sophie Snyder is an employee of BluePath Solutions, which received funding from Bristol Myers Squibb to perform the analyses. Karen C. Chung is a former employee of the study sponsor, Juno Therapeutics, a Celgene Company, prior to the acquisition of Celgene by Bristol Myers Squibb. Monika Jun is an employee of Bristol Myers Squibb, Princeton, NJ. Matthew Gitlin is an employee of BluePath Solutions, which received funding from Bristol Myers Squibb to perform the analyses.
Compliance with Ethics Guidelines
This article does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
All data generated or analyzed during this study are included in this published article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Karen C. Chung was an employee of Juno Therapeutics, a Celgene Company, prior to the acquisition of Celgene by Bristol Myers Squibb.
Supplementary Information
Below is the link to the electronic supplementary material.


Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Snyder, S., Chung, K.C., Jun, M.P. et al. Access to Chimeric Antigen Receptor T Cell Therapy for Diffuse Large B Cell Lymphoma. Adv Ther 38, 4659–4674 (2021). https://doi.org/10.1007/s12325-021-01838-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01838-z