Abstract
Introduction
Patients with asthma typically increase short-acting β2-agonists (SABA) use with worsening symptoms. Excessive SABA use may lead to a higher risk of adverse outcomes. We evaluated, in a large population cohort, an association between SABA inhaler use and asthma exacerbations and healthcare utilization.
Methods
As part of the SABINA (SABA use IN Asthma) global program, we conducted a retrospective longitudinal observational study (SABINA I) using UK primary care electronic healthcare records (Clinical Practice Research Datalink; 2007–2017) from asthma patients aged ≥ 12 years. SABA inhaler use was classified as ‘high use’, ≥ 3 canisters/year versus ‘low use’, 0–2 canisters/year. Taking into consideration all their asthma prescriptions, patients were categorized into a treatment step according to 2016 British Thoracic Society (BTS) asthma management guidelines. Multivariable regression assessed the association of SABA inhaler use by BTS treatment steps (grouped as BTS steps 1/2 and 3–5), separately, and with outcomes of exacerbations or asthma-related healthcare utilization (primary care and hospital outpatient consultations); only patients with linked hospital data were included in this analysis.
Results
Of the 574,913 patients included, 218,365 (38%) had high SABA inhaler use. Overall, 336,412 patients had linked hospital data. High SABA inhaler use was significantly associated with an increased risk of exacerbations [adjusted hazard ratio, 95% confidence interval (CI): BTS steps 1/2 = 1.20, 1.16–1.24; BTS steps 3–5 = 1.24, 1.20–1.28], asthma-related primary care consultations [adjusted incidence rate ratio (IRR), 95% CI: BTS steps 1/2 = 1.24, 1.23–1.26; BTS steps 3–5 = 1.13, 1.11–1.15], and asthma-related hospital outpatient consultations (adjusted IRR, 95% CI: BTS steps 1/2 = 1.19, 1.12–1.27; BTS steps 3–5 = 1.19, 1.13–1.26).
Conclusion
High SABA inhaler use was frequent across BTS steps and was associated with a significant increase in exacerbations and asthma-related healthcare utilization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
In the United Kingdom (UK), asthma exacerbations lead to increased hospitalizations and even death. |
Despite the availability of inhaled corticosteroids, which reduce airway inflammation in asthma, patients tend to overuse short-acting β2-agonists (SABA), which do not address inflammation but only offer immediate symptom relief. |
As part of the SABINA (SABA use IN Asthma) program, this study (SABINA I) was conducted to better understand the extent of SABA inhaler use and any associated impact on asthma-related exacerbations and healthcare utilization in the UK. |
What was learned from the study? |
High SABA use (≥ 3 SABA canisters/year) was observed in over one-third of UK asthma patients (n = 574,913). |
High SABA use was associated with a significant increase in exacerbations and healthcare utilization (primary care and hospital outpatient visits), regardless of treatment step or asthma severity and after adjusting for multiple known exacerbation risk factors. |
The Global Initiative for Asthma no longer recommends treating adolescents and adults with as-needed SABA alone for symptom relief. As these findings reveal high SABA use and associated burden even in patients with mild asthma, there is a need to align SABA prescription practices with current treatment recommendations. |
Introduction
Asthma is a fluctuating disease, with day-to-day variability in inflammation and correspondingly, lung function and symptoms. In the United Kingdom (UK), approximately 7% of the population have active, physician-diagnosed asthma [1]. Asthma management guidelines recommend a stepwise approach to treatment in order to control symptoms and reduce the risk of exacerbations [2, 3]. For decades, the use of short-acting β2-agonists (SABA) has been recommended both as the first treatment step and for symptomatic relief in patients across the spectrum of asthma. A post hoc analysis of the 3-year inhaled Steroid Treatment As Regular Therapy (START) study has shown that treatment with inhaled corticosteroids (ICS) reduced the risk of an asthma-related hospital admission or emergency department visit or death in mild asthma patients compared with placebo [4]. Additionally, two recent randomized controlled trials demonstrated that symptom-driven use of ICS-containing reliever medication reduced the risk of exacerbations in patients with mild asthma as compared with as-needed SABA [5], and was noninferior to daily ICS medication [6]. These studies, alongside earlier evidence and safety concerns since the 1990s regarding the use of SABA [7, 8], led to a landmark change in the 2019 Global Initiative for Asthma (GINA) report, which no longer recommended treatment with SABA alone and instead recommends low-dose ICS-containing medication as the preferred reliever at GINA steps 1 and 2, and, in steps 3–5, for patients prescribed ICS-formoterol maintenance and reliever therapy [2, 9]. Since the GINA update, multiple studies conducted in clinical practice settings have demonstrated the validity of using ICS-formoterol reliever therapy to lower the risk of exacerbations compared with use of SABA as needed [10, 11].
While poor ICS adherence is a concern, regardless of the use of controller medication, high SABA use has been found to be associated with poorer clinical outcomes, including exacerbations and mortality, in addition to increased healthcare utilization [12,13,14,15,16,17,18]. There is a growing view that worsening inflammation contributes toward symptomatic episodes, and that the first-line treatment of worsening symptoms should be with an anti-inflammatory medication (such as ICS-containing medication) rather than purely symptom management with SABA alone [19, 20].
To better understand the impact of SABA inhaler use, the SABINA (SABA use IN Asthma) global program was initiated to describe asthma treatment patterns, the extent of SABA inhaler use, and its subsequent impact on asthma-related clinical outcomes [21]. This study (SABINA I) examined prescription patterns and the impact of SABA inhaler use on asthma-related health outcomes in the UK.
Methods
Data Sources
The Clinical Practice Research Datalink (CPRD-GOLD) currently encompasses primary care data for over 40 million patients across the UK [22], and is representative of the population with respect to age, sex, and body mass index (BMI) [23]. Hospital admissions and outpatient consultation data were obtained from the Hospital Episode Statistics (HES) database. HES only covers hospitals in England; therefore, only around 60% of CPRD practices have patient-level linkage to HES, the Office for National Statistics mortality data, and the Index of Multiple Deprivation (IMD) socioeconomic data.
Study Design and Population
We conducted a retrospective, longitudinal, open-cohort study; asthma patients were identified using validated diagnostic codes [24]. Patients had to have an asthma diagnostic code within 3 years of index date and could either be a new diagnosis (first code occurred in the baseline year, which was 12 months prior to index date) or prevalent disease (≥ 2 validated asthma codes or asthma medication prescriptions > 1 year apart). Index date was set as the latest date of any of the following: asthma diagnosis, 12th birthday, start of study period (April 1, 2007), 1 year after the general practitioner (GP) practice began recording research quality data (CPRD quality control), or 1 year after their continuous CPRD practice registration date (Fig. S1). Patients were censored at the earliest date of death, the end of study period (December 31, 2017), the last CPRD data collection date, or the date transferred out of a CPRD practice. Patients managed on the highest treatment step [continuous or frequent oral corticosteroid (OCS) use] were excluded as these patients are often managed in both primary and secondary care, and their CPRD records may not be complete. Moreover, these patients are unique and regularly use OCS as part of their management; they also constitute approximately < 1% of the cohort. All patients who met the eligibility criteria were included in the prescription analysis. Only patients with CPRD–HES-linked records contributed to the analysis of asthma outcomes (as the outcome measurements required hospital data).
Outcomes and Covariates
Exacerbations were defined as previously described [1, 25, 26], as asthma worsening that necessitated a short course of OCS (GP-managed exacerbation), an Accident and Emergency (A&E) department visit for asthma, a hospital admission or death secondary to asthma. A course of OCS was defined as a prescription [not during an annual asthma review or on days treated for other steroid responsive diseases (see Appendix for list of other steroid responsive diseases)] of a total amount ≤ 300 mg. Primary care consultations for asthma were identified in CPRD as the date of a consultation that occurred on the same day as an asthma diagnostic code. Hospital consultations were identified in HES as the date of a respiratory outpatient clinic. Of note, mortality events in this asthma cohort were too few to be analyzed separately.
The following variables were recorded in the baseline year (12 months before the study entry date): ‘SABA inhaler use’ (number of canisters prescribed), ‘ICS use’ (maximum ICS dose prescribed), proportion of days covered (PDC) by ICS prescriptions, number of exacerbations, and treatment step. SABA inhaler use was categorized as ‘low use’ (0–2 SABA canisters/year) or ‘high use’ (≥ 3 SABA canisters/year). Guideline recommendations for mild asthma in the UK are such that ≥ 3 puffs per week is considered inadequate control [27]. In the UK, SABA canisters contain 100 or 200 puffs and some patients keep a ‘spare’ SABA inhaler; therefore, a cut-off of ≥ 3 canisters was set. SABA inhaler use was also used as a categorical variable (canisters per baseline year: 0–1, 2, 3–6, 7–12, and ≥ 13). PDC was used as a measure of adherence [28] and was calculated as the proportion of the baseline year that had days covered by ICS prescriptions. Treatment step was assigned based on correlation between prescriptions recorded and treatment proposed in the 2016 Scottish Intercollegiate Guidelines Network/British Thoracic Society (SIGN/BTS) guidelines [27]; patients were thus classified into steps 1–5 according to their highest ICS prescription dose in the baseline year [step 1 = no ICS, step 2 = low-dose ICS (400–799 µg, beclomethasone dipropionate equivalent), step 3 = low-dose ICS + long-acting β2-agonist, step 4 = medium-dose ICS (800–1599 µg) ± additional therapies, step 5 = high-dose ICS (> 1600 µg) ± additional therapies] [25]. A history of atopy, gastroesophageal reflux, smoking, pneumonia, anxiety, and depression was recorded using appropriate diagnostic codes (available upon request). Chronic obstructive pulmonary disease (COPD) was identified by validated diagnostic codes, a smoking history, and age > 35 years, while non-smokers with COPD were identified using validated diagnostic codes and age > 35 years [29, 30].
Statistical Analysis
Prescription analysis described the number and proportion of patients in each SABA category in the baseline year by treatment step. Outcomes analysis addressed the association between SABA inhaler use and exacerbations, primary care consultations, and hospital consultations. The mean number of exacerbations during the first year of follow-up and the incidence rate of exacerbations during total study follow-up were estimated according to asthma severity designated by treatment step (grouped as BTS steps 1/2 for mild asthma and steps 3–5 for moderate-to-severe asthma) and SABA inhaler use. To estimate the association between SABA inhaler use and exacerbations, the Cox proportional hazard regression model was used with Andersen-Gill extension to account for repeat outcomes. To estimate the association between SABA inhaler use and primary care consultations, a mixed-effects negative binomial regression model was used; random effects accounted for clustering by patient. To estimate the association between SABA inhaler use and hospital consultations, zero-inflated negative binomial regression, with age as the zero-inflated variable, was used. All regression models used complete case analysis, were stratified by BTS step, and adjusted for age, gender, socioeconomic status (defined using the 2015 Index of Multiple Deprivation [31]), BMI, smoking history, exacerbation history, ICS use, PDC, and comorbidities. Sensitivity analyses were conducted including SABA inhaler use as a categorical variable, excluding patients with a COPD co-diagnosis and excluding patients who were not prescribed a SABA inhaler in the baseline year, and for BTS step 2 patients using ICS. All analyses were performed using STATA 14.2.
Ethical Approval
The protocol for this research was approved by the Independent Scientific Advisory Committee (ISAC) for the Medicines and Healthcare products Regulatory Agency (MHRA) Database Research (protocol number 18_080R) and the approved protocol was made available to the journal and reviewers during peer review. Generic ethical approval for observational research using CPRD with approval from ISAC was granted by a Health Research Authority (HRA) Research Ethics Committee (East Midlands–Derby, REC Reference No. 05/MRE04/87). Linked pseudonymized data were provided for this study by CPRD. Data were linked by National Health Service (NHS) Digital, the statutory trusted third party for linking data, using identifiable data held only by NHS Digital. Select practices consent to this process at a practice level, with individual patients having the right to opt-out.
Results
SABA Inhaler Use Patterns by Asthma Treatment Steps
Of the 709,268 asthma patients identified in the CPRD from April 1, 2007 to December 31, 2017, a total of 574,913 patients were eligible for the prescription analysis (Fig. S1). Of the 134,355 patients excluded, 26,627 belonged to BTS step 6 or were not following BTS guidelines. In step 1, 12% of the patients were high SABA users (Fig. 1). However, the proportion of high SABA users increased with increasing treatment step (step 2 = 44%, step 3 = 54%, step 4 = 57%); over two-thirds of the patients in step 5 were high SABA users (68%). Of note, across BTS steps, a proportion of asthma patients did not receive any SABA inhaler prescriptions in the baseline year (step 1 = 56%, step 2 = 9.6%, step 3 = 14%, step 4 = 13%, step 5 = 9.8%) (Fig. S2). Of those in step 1 not prescribed a SABA inhaler in the baseline year (n = 151,760), 91% in the year before or after the baseline year had either been prescribed asthma medication (n = 105,741) or had attended a GP asthma consultation (n = 31,710). Thus, only 7.3% (n = 14,309) of patients in BTS step 1 did not have any asthma treatment in the year before or after the baseline year.
Description of SABA inhaler use according to BTS treatment step (prescription analysis). BTS British Thoracic Society, ICS inhaled corticosteroids, SABA short-acting β2-agonists. Low use: 0–2 SABA canisters/year; high use: ≥ 3 SABA canisters/year. Step 1 = no ICS; step 2 = low-dose ICS; step 3 = low-dose ICS + long-acting β2-agonist; step 4 = medium-dose ICS ± additional therapies; step 5 = high-dose ICS ± additional therapies
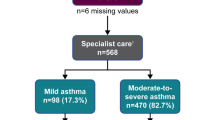
Patient Characteristics of the Outcomes Cohort
A total of 336,412 patients were eligible for the outcomes cohort (Fig. S1); 222,135 (66%) were receiving BTS steps 1/2 treatment, and 114,277 (34%) received steps 3–5 treatment (Table 1). Approximately 60% were female across BTS steps; the majority of patients were aged 18–55 years, 59% in the BTS steps 1/2 cohort and 51% in the BTS steps 3–5 cohort. Among all asthma patients, only 61,428 (18%) had ≥ 75% of days covered with ICS prescriptions, while 118,237 (53%) had no ICS prescriptions. High SABA use occurred among 26% and 57% of BTS steps 1/2 and 3–5 asthma patients, respectively. The proportions of asthma patients at BTS steps 1/2 and 3–5 who experienced ≥ 1 exacerbation during the baseline year were 7% and 24%, respectively.
SABA Inhaler Use and Exacerbations
The mean number of exacerbations during the first year of follow-up was 1.7–2.2 times higher among high SABA users than among low SABA users across treatment steps (Fig. 2). In all patients, the rate of exacerbations was almost double in high SABA users compared with low SABA users [BTS steps 1/2: low SABA use = 1.66 exacerbations per 10 person-years, 95% confidence interval (CI) 1.62–1.69 and high SABA use = 2.96 exacerbations per 10 person-years, 95% CI 2.87–3.05; BTS steps 3–5: low SABA use = 4.15 exacerbations per 10 person-years, 95% CI 4.04–4.26 and high SABA use = 7.83 exacerbations per 10 person-years, 95% CI 7.70–7.96; Table 2]. The increase in exacerbation rates in high SABA users compared with low SABA users remained regardless of where the exacerbation was treated (by a GP, in an A&E department, or in a hospital; Table 3).
Mean number of exacerbations in the first year of follow-up, by BTS treatment step and SABA inhaler use frequency (outcomes cohort). BTS British Thoracic Society, ICS inhaled corticosteroids, SABA short-acting β2-agonists. Step 1 no ICS; step 2 low-dose ICS; step 3 low-dose ICS + long-acting β2-agonist; step 4 medium-dose ICS ± additional therapies; step 5 high-dose ICS ± additional therapies. Low use: 0–2 SABA canisters/year; high use: ≥ 3 SABA canisters/year
Patients at BTS steps 1/2 with high SABA use had a 20% increased rate of exacerbations compared with low SABA users, even after adjusting for ICS use, age, gender, BMI, socioeconomic status, smoking, recent exacerbations and history of pneumonia, atopy, reflux, COPD, anxiety, and depression [adjusted hazard ratio (HR) = 1.20, 95% CI 1.16–1.24]. Patients at BTS steps 3–5 with high SABA use had a 24% increased rate of exacerbations (adjusted HR = 1.24, 95% CI 1.20–1.28) (Table 4).
For BTS steps 1/2 patients, a significant dose–response effect of increased exacerbation risk was found with increasing SABA inhaler use once patients used ≥ 3 SABA canisters/year [SABA canisters/year, HR (95% CI) 2 = 1.00 (0.96–1.05); 3–6 = 1.14 (1.09–1.19); 7–12 = 1.26 (1.18–1.33); ≥ 13 = 1.52 (1.37–1.68); Table 5]. In BTS steps 3–5 patients, the dose–response effect occurred at ≥ 2 SABA canisters/year [SABA canisters/year, HR (95% CI) 2 = 1.09 (1.04–1.14); 3–6 = 1.19 (1.14–1.23); 7–12 = 1.37 (1.31–1.43); ≥ 13 = 1.55 (1.47–1.64); Table 5].
Estimates were not significantly affected by the exclusion of patients with COPD or zero-SABA inhaler users in the sensitivity analyses (Tables S1–S3). Similar results were seen among patients at BTS steps 1/2 who were prescribed ICS (Table S4). Notably, exacerbation risk was strongly associated with the highest adherence tertile in this subset of patients.
SABA Inhaler Use and Primary Care and Hospital Consultations
The adjusted incidence rate ratio (IRR) for primary care consultations comparing high SABA users with low SABA users was 1.24 (95% CI 1.23–1.26) among BTS step 1/2 patients and 1.13 (95% CI 1.11–1.15) among patients at BTS steps 3–5 (Table 6). For hospital consultations, the adjusted IRR was 1.19 (95% CI 1.12–1.27) among BTS steps 1/2 patients and 1.19 (95% CI 1.13–1.26) among BTS steps 3–5 patients, respectively (Table 7).
Discussion
In this real-world, observational study, high SABA inhaler use was prevalent in over one-third of UK patients with asthma. High SABA users were significantly more likely to have exacerbations than low SABA users, even after considering multiple known exacerbation risk factors, in patients across BTS steps. High SABA users were also significantly more likely to attend primary care consultations and consultations with a specialist, regardless of asthma severity.
Consistent with previous UK data [25], the majority of patients (65%) received BTS steps 1/2 treatment and may be considered to have mild asthma. Notably, over half of the patients were managed on BTS step 1 treatment. While the BTS guidelines are used across the UK, both BTS and GINA recommend a stepwise approach to the pharmacological treatment of asthma and until recently [9], GINA recommended a similar management approach for patients with mild asthma [32]. However, the 2019 GINA report saw a fundamental change, recommending that step 1 treatment is no longer SABA alone but includes low-dose ICS-formoterol as a preferred reliever [2]. Our study found that even mild asthma patients experienced exacerbations, in keeping with previous findings [5, 6, 26, 33,34,35], and that this risk appeared to be further elevated with high SABA use. This analysis points to an association but not a causal relationship between over-reliance on SABA inhalers and poor clinical outcomes in patients with mild asthma. This evidence of an association even while adjusting for confounding factors, such as exacerbation history (potentially indicating poor control), ICS dose, and PDC (in BTS step 2 patients), indicates that high use of SABA inhalers, in part, may contribute to poor clinical outcomes in this subset of patients. These real-world findings therefore appear to support the concept of treating mild asthma patients with anti-inflammatory medications and not just a short-acting bronchodilator alone.
A significant dose–response effect of increased exacerbation risk with increasing SABA inhaler use was seen across severities. SABA inhaler use, from as few as 2 canisters/year in patients receiving BTS steps 3–5 treatment (and thus potentially having moderate-to-severe asthma), was a significant risk factor for exacerbations even after considering disease severity and multiple other known risk factors. Earlier observational studies addressing concerns related to SABA use have reported similar results, but the studies have only focused on hospitalized exacerbations [15,16,17, 36]. In contrast, our study addressed exacerbations managed within primary and secondary care.
The largest study preceding this one was carried out in a Canadian population, which used administrative data to evaluate the risk of SABA use on hospitalizations [12]. They found an increase in hospitalizations, but the question remained whether the increases observed were related to the financial barriers faced by some Canadian patients due to incomplete publicly administered medication coverage. Similarly, a previous study conducted in the United States, which also used administrative data, found considerable increments in total healthcare costs with increasing SABA use, posing the same question about the impact of financial barriers [16]. This UK study, evaluating the impact in a population with complete medication coverage, has shown that the association between high SABA use and adverse asthma outcomes and healthcare utilization is not related to financial barriers.
Notably, these results highlight high SABA use and associated burden even in patients with mild asthma. Whether the healthcare utilization burden associated with high SABA use is due to patients having poor asthma control, or whether this represents actual burden associated with high SABA use itself, will require further investigation. It is possible that increased SABA inhaler use is preceded by the deterioration of asthma control and is reflected by an increase in patient’s symptoms. Asthma control was not specifically adjusted for in this analysis; however, exacerbation history was one of the confounding factors, which may indirectly reflect asthma control. Of note, assessment of qualitative research focusing on patient-centered drivers of poor medication adherence suggests that SABA overuse may not always be related to the severity of the disease. It may also be due to factors including ICS underuse driven by suboptimal patient knowledge about the difference between maintenance and reliever medication, the patient’s need for immediate symptom relief, concerns about the side-effects of steroids, and poor communication between patients and physicians [37]. Additionally, previous analysis of the same patient cohort revealed that, over an 8-year period, SABA prescriptions at the population-level have remained stable [38]. However, there was greater variability year to year in prescriptions of SABA compared with ICS, suggesting that SABA use, rather than ICS use, may be altered in response to changes in asthma control [38]. Overall, these findings indicate a need for outreach strategies involving medical education targeted at patients, healthcare providers, and policymakers, and digital health initiatives (e.g., digital inhalers) [39, 40], in order to align SABA prescription behavior with current treatment recommendations.
The use of the CPRD has several limitations. Prescriptions recorded in the database did not necessarily represent dispensed or used inhalers, potentially leading to an overestimation of actual SABA inhaler use. The baseline BTS step was used to represent severity throughout follow-up, and it is possible that this changed over time. Additionally, many patients on step 1 treatment did not receive a SABA prescription in the baseline year and therefore potentially did not have active asthma. However, sensitivity analyses excluding these patients did not yield a change in effect estimates (Table S3), and 91% received asthma management in the year before or after the baseline year. It is possible that the remaining 9% were in remission, misdiagnosed, or did not wish to receive treatment for their asthma during the 3-year period. The outcomes cohort (requiring patients only with HES linkage) constituted approximately 60% of the total asthma patients eligible for the prescription analysis; this could lead to a selection bias, although HES has universal coverage of English hospitals, thus providing an unselected sample [41]. In most countries including the UK, SABA inhalers contain 100 or 200 puffs. However, in order to standardize the threshold for high SABA use across countries in the SABINA program, a SABA inhaler was considered to contain an assumed average of 150 puffs. Nebulized SABA use was not analyzed separately; however, it is not commonly prescribed in the UK, except for more severe asthma patients [42], and is recommended for the treatment of acute severe asthma attacks in children by paramedics or in the A&E [27].
Limited data on the burden of high SABA use and considerable variability in the definition of SABA ‘overuse’ [17, 43,44,45] have made comparisons with previous studies and regions challenging. In the SABINA program [21], the definition of high SABA use has been standardized across studies, enabling comparison and harmonization of results across geographies. Emerging data from more than 1 million patients in the SABINA program reveal that high SABA use is also prevalent in other European countries, such as Sweden (30%), Germany (16%), Spain (29%), and Italy (9%), and is found across asthma severities [46]. Moreover, the HERA study, conducted in a Swedish asthma cohort as part of the SABINA program, showed similar results: among high SABA users, constituting one-third of all asthma patients, the risk of exacerbations and asthma-related mortality significantly increased with use of ≥ 3 SABA canisters/year [47]. The current study describes SABA inhaler use in more than half a million asthma patients, allowing for characterization of exacerbation rates and healthcare utilization across all asthma severities. Furthermore, patients in CPRD are nationally representative in terms of age, sex, and BMI [23], ensuring that the results of this study are generalizable to the national population. Additionally, in the UK healthcare system, all patients are assigned to a GP and most prescriptions are undertaken in primary care, as GPs are in a good position to provide continuing care. Thus, these findings on SABA inhaler prescription patterns are representative of the entire UK asthma patient population.
Conclusions
Our findings in SABINA I, part of the SABINA program, show that a large proportion of asthma patients in the UK have high SABA inhaler use. Across all asthma severities, an association was found between high SABA use, namely use of ≥ 3 canisters/year, and an increase in exacerbation rates and healthcare utilization.
References
Bloom CI, Saglani S, Feary J, Jarvis D, Quint JK. Changing prevalence of current asthma and inhaled corticosteroid treatment in the UK: population-based cohort 2006–2016. Eur Respir J. 2019;53:1802130.
Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention; 2019. https://ginasthma.org/. Accessed 13 Jan 2020.
British Thoracic Society. Scottish Intercollegiate Guidelines Network: British Guideline on the Management of Asthma; 2019. https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/. Accessed 13 Jan 2020.
Reddel HK, Busse WW, Pedersen S, et al. Should recommendations about starting inhaled corticosteroid treatment for mild asthma be based on symptom frequency: a post-hoc efficacy analysis of the START study. Lancet. 2017;389:157–66.
O’Byrne PM, FitzGerald JM, Bateman ED, et al. Inhaled combined budesonide-formoterol as needed in mild asthma. N Engl J Med. 2018;378:1865–76.
Bateman ED, Reddel HK, O’Byrne PM, et al. As-needed budesonide-formoterol versus maintenance budesonide in mild asthma. N Engl J Med. 2018;378:1877–87.
Hancox RJ, Cowan JO, Flannery EM, Herbison GP, McLachlan CR, Taylor DR. Bronchodilator tolerance and rebound bronchoconstriction during regular inhaled beta-agonist treatment. Respir Med. 2000;94:767–71.
Suissa S, Ernst P, Boivin JF, et al. A cohort analysis of excess mortality in asthma and the use of inhaled beta-agonists. Am J Respir Crit Care Med. 1994;149:604–10.
Reddel HK, FitzGerald JM, Bateman ED, et al. GINA 2019: a fundamental change in asthma management. Eur Respir J. 2019;53:1901046.
Beasley R, Holliday M, Reddel HK, et al. Controlled trial of budesonide-formoterol as needed for mild asthma. N Engl J Med. 2019;380:2020–30.
Hardy J, Baggott C, Fingleton J, et al. Budesonide-formoterol reliever therapy versus maintenance budesonide plus terbutaline reliever therapy in adults with mild to moderate asthma (PRACTICAL): a 52-week, open-label, multicentre, superiority, randomised controlled trial. Lancet. 2019;394:919–28.
FitzGerald JM, Tavakoli H, Lynd LD, Al Efraij K, Sadatsafavi M. The impact of inappropriate use of short acting beta agonists in asthma. Respir Med. 2017;131:135–40.
Makhinova T, Barner JC, Richards KM, Rascati KL. Asthma controller medication adherence, risk of exacerbation, and use of rescue agents among Texas Medicaid patients with persistent asthma. J Manag Care Spec Pharm. 2015;21:1124–32.
Patel M, Pilcher J, Munro C, et al. Short-acting β-agonist use as a marker of current asthma control. J Allergy Clin Immunol Pract. 2013;1:370–7.
Senthilselvan A, Lawson JA, Rennie DC, Dosman JA. Regular use of corticosteroids and low use of short-acting beta2-agonists can reduce asthma hospitalization. Chest. 2005;127:1242–51.
Silver HS, Blanchette CM, Kamble S, et al. Relationship between short-acting β2-adrenergic agonist use and healthcare costs. Am J Manag Care. 2011;17:19–27.
Hull SA, McKibben S, Homer K, Taylor SJ, Pike K, Griffiths C. Asthma prescribing, ethnicity and risk of hospital admission: an analysis of 35,864 linked primary and secondary care records in East London. NPJ Prim Care Respir Med. 2016;26:16049.
Stanford RH, Shah MB, D’Souza AO, Dhamane AD, Schatz M. Short-acting β-agonist use and its ability to predict future asthma-related outcomes. Ann Allergy Asthma Immunol. 2012;109:403–7.
O’Byrne PM, Jenkins C, Bateman ED. The paradoxes of asthma management: time for a new approach? Eur Respir J. 2017;50:1701103.
Pavord ID, Beasley R, Agusti A, et al. After asthma: redefining airways diseases. Lancet. 2018;391:350–400.
Cabrera CS, Nan C, Lindarck N, Beekman MJ, Arnetorp S, van der Valk RJ. SABINA: global programme to evaluate prescriptions and clinical outcomes related to short-acting β2-agonist use in asthma. Eur Respir J. 2020;55:1901858.
Clinical Practice Research DataLink (CPRD). https://www.cprd.com/home. Accessed 13 Jan 2020.
Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol. 2015;44:827–36.
Nissen F, Morales DR, Mullerova H, Smeeth L, Douglas IJ, Quint JK. Validation of asthma recording in the Clinical Practice Research Datalink (CPRD). BMJ Open. 2017;7:e017474.
Bloom CI, Nissen F, Douglas IJ, Smeeth L, Cullinan P, Quint JK. Exacerbation risk and characterisation of the UK’s asthma population from infants to old age. Thorax. 2018;73:313–20.
Bloom CI, Palmer T, Feary J, Quint JK, Cullinan P. Exacerbation patterns in adults with asthma in England. A population-based study. Am J Resp Crit Care Med. 2019;199:446–53.
British Thoracic Society. Scottish Intercollegiate Guidelines Network: British guideline on the management of asthma; 2016. https://www.brit-thoracic.org.uk/document-library/guidelines/asthma/btssign-asthma-guideline-2016/. Accessed 13 Jan 2020.
Raebel MA, Schmittdiel J, Karter AJ, Konieczny JL, Steiner JF. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med Care. 2013;51(8 Suppl 3):S11–21.
Quint JK, Müllerova H, DiSantostefano RL, et al. Validation of chronic obstructive pulmonary disease recording in the Clinical Practice Research Datalink (CPRD-GOLD). BMJ Open. 2014;4:e005540.
Nissen F, Morales DR, Mullerova H, et al. Concomitant diagnosis of asthma and COPD: a quantitative study in UK primary care. Br J Gen Pract. 2018;68:e775–e782.
Department for Communities and Local Government. The English indices of deprivation 2015: statistical release; 2015. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015. Accessed 24 July 2020.
Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention; 2017. https://ginasthma.org/archived-reports/. Accessed 27 Feb 2020.
O’Byrne PM, Barnes PJ, Rodriguez-Roisin R, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med. 2001;164:1392–7.
Price D, Fletcher M, van der Molen T. Asthma control and management in 8000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med. 2014;24:14009.
Suruki RY, Daugherty JB, Boudiaf N, Albers FC. The frequency of asthma exacerbations and healthcare utilization in patients with asthma from the UK and USA. BMC Pulm Med. 2017;17:74.
Gonem S, Cumella A, Richardson M. Asthma admission rates and patterns of salbutamol and inhaled corticosteroid prescribing in England from 2013 to 2017. Thorax. 2019;74:705–6.
Amin S, Soliman M, McIvor A, Cave A, Cabrera C. Understanding patient perspectives on medication adherence in asthma: a targeted review of qualitative studies. Patient Prefer Adherence. 2020;14:541–51.
Bloom C, Quint J, Cabrera C. SABA and ICS use among mild asthma patients in UK primary care. Eur Respir J. 2019;54(suppl 63):PA2565.
Merchant R, Szefler SJ, Bender BG, et al. Impact of a digital health intervention on asthma resource utilization. World Allergy Organ. 2018;11:28.
Barrett MA, Humblet O, Marcus JE, et al. Effect of a mobile health, sensor-driven asthma management platform on asthma control. Ann Allergy Asthma Immunol. 2017;119:415–21.
Padmanabhan S, Carty L, Cameron E, Ghosh RE, Williams R, Strongman H. Approach to record linkage of primary care data from Clinical Practice Research Datalink to other health-related patient data: overview and implications. Eur J Epidemiol. 2019;34:91–9.
National Health Service (NHS). Salbutamol inhaler. https://www.nhs.uk/medicines/salbutamol-inhaler/. Accessed 05 June 2020.
Belhassen M, Nibber A, Van Ganse E, et al. Inappropriate asthma therapy-a tale of two countries: a parallel population-based cohort study. NPJ Prim Care Respir Med. 2016;26:16076.
Elkout H, Helms PJ, Simpson CR, McLay JS. Changes in primary care prescribing patterns for paediatric asthma: a prescribing database analysis. Arch Dis Child. 2012;97:521–5.
Slejko JF, Ghushchyan VH, Sucher B, et al. Asthma control in the United States, 2008–2010: indicators of poor asthma control. J Allergy Clin Immunol. 2014;133:1579–87.
Janson C, Menzies-Gow A, Nan C, et al. SABINA: an overview of short-acting β2-agonist use in asthma in European countries. Adv Ther. 2020;37:1124–35.
Nwaru B, Ekström M, Hasvold P, Wiklund F, Telg G, Janson C. Overuse of short-acting β2-agonists in asthma is associated with increased risk of exacerbation and mortality: a nationwide cohort study of the global SABINA programme. Eur Respir J. 2020;55:1901872.
Acknowledgements
Funding
This study and medical writing support were funded by AstraZeneca. The sponsor designed the study and was involved in the analysis and interpretation of the data. AstraZeneca also funded the journal’s Rapid Service Fees for publication of this manuscript and the open access fees.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Medical Writing, Editorial, and Other Assistance
Medical writing and editorial support was provided by Michelle Rebello, PhD, CMPP, of Cactus Life Sciences (part of Cactus Communications) (Mumbai, India), which was funded by AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines http://www.ismpp.org/gpp3.
Disclosures
Claudia Cabrera, Sofie Arnetorp, Karen Coulton, Cassandra Nan, and Ralf J. P. van der Valk are employees of AstraZeneca and hold shares in AstraZeneca. Cassandra Nan and Ralf J. P. van der Valk also hold shares in GlaxoSmithKline. Jennifer K. Quint’s research group received funding from AstraZeneca for this work, and funding from Asthma UK, The Health Foundation, MRC, Wellcome Trust, BLF, GlaxoSmithKline, Insmed, AstraZeneca, Bayer, Chiesi, IQVIA, and Boehringer Ingelheim, outside of the submitted work. Jennifer K. Quint received funds from AstraZeneca, GlaxoSmithKline, Chiesi, Bayer, Teva, and Boehringer Ingelheim for Advisory board participation or travel.
Compliance with Ethical Guidelines
The protocol for this research was approved by the Independent Scientific Advisory Committee (ISAC) for the Medicines and Healthcare products Regulatory Agency (MHRA) Database Research (protocol number 18_080R) and the approved protocol was made available to the journal and reviewers during peer review. Generic ethical approval for observational research using CPRD with approval from ISAC was granted by a Health Research Authority (HRA) Research Ethics Committee (East Midlands–Derby, REC reference number 05/MRE04/87). Linked pseudonymized data were provided for this study by CPRD. Data were linked by National Health Service (NHS) Digital, the statutory trusted third party for linking data, using identifiable data held only by NHS Digital. Select practices consent to this process at a practice level, with individual patients having the right to opt-out.
The studies carried out under the SABINA program conformed with ethical principles that are consistent with the Declaration of Helsinki of 1964 and its later amendments, ICH GCP, GPP3, and the applicable legislation on noninterventional studies and/or observational studies.
Data Availability
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12631229.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bloom, C.I., Cabrera, C., Arnetorp, S. et al. Asthma-Related Health Outcomes Associated with Short-Acting β2-Agonist Inhaler Use: An Observational UK Study as Part of the SABINA Global Program. Adv Ther 37, 4190–4208 (2020). https://doi.org/10.1007/s12325-020-01444-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01444-5