Abstract
Introduction
To date, no study has reported the prevalence of cannabis use in chronic pain patients. The aim of this study is to investigate the trends in cannabis use among chronic pain in-patients from 2011 to 2015 in the USA.
Methods
Patients were identified from the National Inpatient Sample (NIS) database using the International Classification of Diseases, Ninth and Tenth Revision, diagnosis codes for chronic pain and cannabis use. Annual estimates and trends were determined for cannabis use, patient characteristics, cannabis use among subgroups of chronic pain conditions, cost, length of stay, and associated discharge diagnosis.
Results
Between 2011 to 2015, a total of 247,949 chronic pain patients were cannabis users, increasing from 33,189 to 72,115 (P < 0.001). There were upward trends of cannabis use in females (38.7–40.7%; P = 0.03), Medicare insured patients (32.7–40.4%; P < 0.01), patients with lowest annual household income (36.1–40.9%; P = 0.02), patients aged 45–64 years (45.9–49.2%; P < 0.001), and patients with tobacco use disorder (63.8–72.4%; P < 0.0001). Concurrently, cannabis use decreased among patients with opioid use disorder (23.8–19.9%; P < 0.001). Cannabis use increased from 2011 to 2015 in patients with chronic regional pain syndrome, trauma, spondylosis, and failed back surgery syndrome. Adjusted total hospitalization cost increased from $31,271 ($1333) in 2011 to $38,684 ($946) in 2015 (P < 0.001).
Conclusions
Cannabis use increased substantially from 2011 to 2015, while the rates of cannabis use in opioid users down-trended simultaneously. Disparities in cannabis use among subgroups should be explored further.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Why carry out this study? |
Cannabis is a commonly used psychoactive substance, and its use has been suggested to have a high prevalence among patients with chronic pain |
With the recent legalization of marijuana across several states in the US, there is a dire need to establish a baseline use among hospitalized patients |
The aim of this study is to investigate the trends in cannabis use among chronic pain in-patients from 2011 to 2015 in the US |
What was learned from the study? |
We found that cannabis use is increasing among chronic pain patients and a subpopulation of chronic pain patients (tobacco users, men, low household income, Medicaid insurance coverage, and certain chronic pain syndromes). However, we observed that the rates of cannabis use in opioid users were down-trending simultaneously |
In the era of recent legalization of cannabis use in certain regions of the US, our study reveals a rising trend among certain groups of hospitalized patients with chronic pain |
Introduction
Chronic pain is a major public health issue with an estimated 12-month prevalence of 37% in developed countries and as high as 41% in developing countries [1]. Cannabis is a commonly used psychoactive substance, and its use has been suggested to have a high prevalence among patients with chronic pain [2]. Prior to the recent ongoing legalizations driven by public demand, illegal access to the substance was exceptionally high [3]. Now cannabis is the most frequently consumed illicit drug, driven by increased availability and new medicinal perspective [4].
Though cannabis use was a taboo just a decade ago, increased widespread availability of medical and recreational cannabis coupled with social acceptability and its potential medicinal value has led to a normalization of its use in everyday life. Despite the lower potential addiction potential of those who consume cannabis, one in ten will progress to develop cannabis use disorder [5, 6]. Cannabis use may be a precipitating factor in further developing additional substance abuse and has been implicated in a causal model for abuse/dependence on a diversity of other drugs [7].
This is evidenced by a report of the health effects of cannabis, which supports the use of cannabis for chronic pain and associated conditions such as fibromyalgia, multiple sclerosis, and sleep apnea [8]. As cannabis gains a role in the treatment of chronic pain conditions, the development of cannabis use disorder and ultimately subsequent illicit substance abuse disorder in patients becomes a concern [9]. In this study we assess the prevalence of cannabis use among inpatients with chronic pain using a national inpatient database.
Methods
Database Characteristics
NIS data from 2011 to 2015 were reviewed and included in our analysis. The NIS (National Inpatient Sample) is one of the Healthcare Cost and Utilization Projects databases sponsored by the Agency for Healthcare Research and Quality [10]. This database is considered the largest all-payer inpatient care database in the US and has been used in multiple instances to analyze national trends in outcomes, quality, charges, access, and health care utilization based on data extracted from 7 to 8 million hospital stays.
These hospital stays represent approximately 20% of the US community hospitals, defined as all academic medical centers, general specialty hospitals, and non-federal and short-term medical centers. The NIS is publicly available and contains no personal identifying information. Hence, this study was exempt from institutional review board approval. In our analysis, we included chemical dependency treatment facilities, long-term acute care hospitals, short-term rehabilitation facilities, and psychiatric hospitals. Hospitals within a given stratum have similar statistical probability of sample selection regardless of appearance in a prior sample. Further information on the design and statistical information of the NIS is available at http://www.hcup-us.ahrq.gov.
Inclusion and Exclusion Criteria
Our study evaluated patient information data acquired from NIS from 2011 to 2015 to determine the trends of comorbid cannabis use in patients with chronic pain. Cannabis users were identified based on International Classification of Diseases (ICD) codes for cannabis dependence (ICD-9 codes: 304.30-3, ICD-10 codes: F12.10, F12.11, F12.19, F12.20, F12.21, F12.29, F12.288, F12.988, and F12.188) and non-dependence (ICD-9 codes: 305.20-3, ICD-10 codes: F12.90, F12.99). This definition is consistent with prior reported studies in the cardiovascular literature [11, 12]. Due to the lack of specific ICD-9-CM codes for medical cannabis use, we assumed that patients with a clinical diagnosis of cannabis abuse, dependence, or non-dependence represent patients with recreational cannabis use. Studies have shown that medical cannabis users also use cannabis recreationally [13, 14] with 86% of people who report ever using cannabis for medicinal purposes also using it recreationally [15]. Hence, ICD-9-CM codes for cannabis abuse, dependence, or disorder were used to represent recreational cannabis use. Patients without a diagnosis of chronic pain were excluded from our analysis.
Outcomes
Our primary outcomes were trends in cannabis use, patient characteristics, and cannabis use among subgroups of chronic pain conditions. Hospital charges, length of hospital stay, number of inpatient procedures, discharge destinations, and associated discharge diagnosis were considered our secondary outcomes. The appropriate weights from the NIS database were applied to obtain trends and annual national estimates.
Statistical Analysis
In our statistical analysis, we calculated the frequencies of these outcomes for each year and determined whether there were any trends in outcomes from 2011 to 2015. We used guidance from the Agency for Healthcare Research and Quality for survey analysis. Survey-specific commands were used to obtain descriptive statistics and perform trend analyses (e.g., svymean, svytab, svyregress). The provided trend weights were used to obtain national estimates. For tests of trend, we used survey-specific linear regression. We adjusted for trends in patient characteristics over time by using a logistic regression model for survey data (svy:regress) and included the year (centered around the mean) as a continuous variable. We conducted our analysis using STATA 14 [16].
Compliance with Ethics Guidelines
This study uses anonymous patient data from another source and so is exempt from needing ethics approval.
Results
Trends of Cannabis Use in Chronic Pain Patients
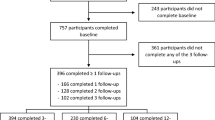
Between 2011 to 2015, approximately 10.3 million patients with chronic pain were identified. Of this cohort 247,949 were cannabis users. The estimated number of patients using cannabis increased from 33,189 in 2011 to 72,114 in 2015 (P < 0.001) (Table 1). The yearly prevalence of cannabis use among patients with chronic pain increased from 2.4% in 2011 to 3.9% in 2015 (P < 0.001) (Fig. 1).
Trends of Cannabis Use and Patient Characteristics
The trends in patient characteristics are displayed in Table 1. The mean (SE) age of cannabis users increased from 42.80 (0.25) to 45.40 (0.14) years (P < 0.0001) with the highest proportion of patients observed among patients aged 45–64 years. The lowest proportion was observed in elderly patients > 84 years old. Between 2011 to 2015, there was an upward trend in cannabis use among patients within the 45–64- and 65–84-year age groups. Cannabis use was lower among females, and the proportion increased from 38.7 in 2011 to 40.2 in 2015 (P = 0.03). The proportions of cannabis users were highest among whites at 70.1% (0.39) with the lowest proportion observed in Asian/Pacific Islanders at 0.51% (0.05). From 2011 to 2015, the proportion of cannabis use increased from 17.8% (1.20) to 21.0% (0.66) among blacks but decreased from 71.4% (1.50) to 69.7% (0.74) among whites.
Patients at the lowest income quartile had the highest proportion of cannabis use, 39.4% (0.47), and those at the highest quartile had the lowest proportion of cannabis use, 11.9% (0.28). From 2011 to 2015, the proportion of cannabis users increased from 36.1% (1.90) to 40.9% (0.74) among the lowest income quartile but decreased from 13.1% (1.10) to 12.0% (0.52) among the highest income quartile. Patients with cannabis use were mostly covered by Medicaid and least often covered by private insurance (36.8% vs. 11.9%; P = 0.02). From 2011 to 2015, the proportion of cannabis users increased from 32.7% (1.10) to 40.4% (0.63) among Medicaid patients but remained stable among Medicare and private insurance patients. Most patients who used cannabis were admitted at hospitals with large bed sizes compared to smaller sizes (59.9% vs. 14.08%; P < 0.0001). From 2011 to 2015, the proportion of cannabis users increased from 8.4% (1.20) to 15.9% (0.90) among small bed size facilities but decreased from 68.2% (2.56) to 56.7% (1.50) among larger bed size facilities.
Trends of Cannabis Use Among Subgroups of Chronic Pain Diagnosis
Trauma patients had the highest proportion of cannabis users but patients with failed back surgery syndrome (FBSS) had the lowest proportion (6.89% vs. 0.70%) (Table 2). From 2011 to 2015, the proportion of cannabis users trended up among patients with chronic regional pain syndrome (CRPS) [1.25 (0.17) to 1.96 (0.24); P = 0.02], trauma [5.23 (0.56) to 8.98 (0.71); P < 0.001], spondylosis [0.57 (0.04) to 1.2 (0.05); P < 0.001], FBSS [0.47 (0.12) to 0.97 (0.15); P < 0.001], and other chronic pain diagnoses [2.4 (0.11) to 3.49 (0.07); P < 0.01]. However, the trend of cannabis use was stable among post-surgical patients (P = 0.72).
Trends of Cannabis Use and Healthcare Utilization
After adjusting for inflation, the total hospital cost of patients with cannabis use increased from $31,271 ($1333) in 2011 to $38,684 ($946) in 2015 (P < 0.001) (Table 3). The mean length of hospital stay trended up marginally from 2012 to 2015 (P = 0.03). The majority of patients were discharged home or to self-care (77.9%).
Trends of Cannabis Use and Discharge Diagnosis
The proportion of cannabis use among chronic pain patients who had a diagnosis of tobacco use disorder (TUD), depression, and opioid use disorder (OUD) were 68.8%, 20.0%, and 21.9%, respectively. From 2011 to 2015, there was an increase in cannabis use among patients with TUD (63.8% vs. 72.4%; P < 0.001). However, we noticed a decline in cannabis use among patients with OUD patients (23.8% vs. 19.9%; P < 0.01).
Discussion
Our study found that, within our sample, the proportion of patients with chronic pain using cannabis was 2.4%. Moreover, over the course of our study, from 2011 to 2015, we identified a significant and progressive increase in the number of patients using cannabis. In patients with chronic pain, cannabis use more than doubled during this period, from 33,189 to 72,114 people. We observed an increasing trend in patients with chronic regional pain syndrome (1.25–1.96%), trauma (5.23–8.98%), spondylosis 0.57–1.2%), FBSS (0.47–0.97%), and other chronic pain diagnoses (2.4–3.49%) (Table 2). This overall increase is not surprising given that several studies have shown cannabis to be effective in mitigating inflammation and demonstrated benefit to chronic pain symptoms with the use of cannabis, including improved pain, functional outcomes, and quality of life in patients with chronic pain syndromes [17,18,19,20,21,22,23]. With chronic pain projected to increase over the next 2 decades to a rate of one in three people from the current rate of one in five people, our findings foretell that cannabis use can be projected to increase even more rapidly [24,25,26]. As evidence of benefits of cannabis use grows, even countries slow to embrace medical cannabis legislation have seen increases in patient awareness of and interest in the therapy [27].
While our study identified a rising prevalence in the use of cannabis among patients with chronic pain, patients with chronic pain frequently have comorbid conditions that may additionally benefit from cannabis use. Various studies have reported that the increased enactment of medicinal cannabis will lead to improved access to cannabis as an alternative pharmaceutical therapy for the treatment of several chronic pain conditions [28, 29]. Across all states that had legalized cannabis for medical use, Baron et al. found pain syndromes, such as migraines, headaches, and arthritis, reported as the most common indication for cannabis use. In addition they found opioids to account for the majority of prescription medications substituted with cannabis, followed by anti-depressants, anti-anxiety medications, and nonsteroidal anti-inflammatory drugs (NSAIDs) [28].
Despite the rising trend of cannabinoid use, which implies improved access to patients who have a need for cannabinoid management of chronic pain, concerns remain regarding cannabis serving as a common illicit gateway drug [29]. This is evidenced by studies that demonstrate a rise in cannabis use among teens, supported by a corresponding decline in the perception of associated risk [30, 31]. In the whole population, approximately 12% of people aged ≥ 12 years had used cannabis at least once in the past year [30]. This observed increase in use suggests a perceived risk of use as well as increase of use among the general population is significant and may contribute to our finding of an increased trend of cannabis use in chronic pain patients. As a whole, these observations may shed light on the overall transformation of knowledge, attitudes, and beliefs in the US population toward the social acceptability of cannabis use; however, further research is needed to investigate outcomes of widespread increases in cannabis use.
Our study showed that the average age of chronic pain patients who use cannabis increased from 42.8 to 45.4 years during the years 2011 to 2015. Moreover, the highest proportion of cannabis use was observed in patients aged 45–84 years and the lowest in those > 85. These results are in line with the findings of Baron et al. who found a mean age of 40 years among all cannabis users but conflict with the results of Vin-Ravin et al., who found 65% of cannabis users to be < 40 years old [28, 32].
The majority of chronic pain patients using cannabis belonged to a lower socioeconomic class (SEC) compared to non-cannabis users. This was similarly shown by Hill et al. and Vin-Raviv et al. [29, 32]. The lowest proportion of cannabis use, 11.9%, was found in the highest income quartile while the highest proportion of cannabis use, 39.4%, was in the lowest income quartile. In our analysis of the payer base, we found that patients with cannabis use were mostly covered by Medicaid. Furthermore, we observed an increased proportion of cannabis users on Medicaid, from 32.7 to 40.4%. Cannabis users were least covered by private insurance, 11.9%, compared to non-cannabis users, 36.8%.
In contrast, Baron et al. reported cannabis use to be associated with a higher SEC [28]. Moreover, Baron et al. found that patients who use cannabis for chronic pain syndromes were more likely to be employed (62.8%) and have education beyond high school (73.6%). Only 5.5% of the patients using medicinal cannabis for chronic pain were retired, which is in line with a decrease in observed use with increasing age. Their study was conducted via electronic questionnaire, which may be a source of selection bias leading to a preponderance of the upper class accounting for the discrepancy between our results. Despite this limitation and potential for bias, a trend of increased cannabis use among patients of higher SEC may be correlated with increased awareness, knowledge, and access to the benefits of cannabis use. Our analysis however does not support this trend; over the course of our study period, the lowest income quartile saw an increase in the proportion of cannabis users, 36.1–40.9%, whereas the highest income quartile saw a decrease in the proportion of cannabis users, 13.1–12.0%. A history of chronic pain may contribute to this observed discrepancy although further studies are needed for elucidation.
Healthcare cost and utilization have been shown to be highest in patients with increasing numbers of comorbidities [33, 34]. In our study we note that the total hospital cost of patients with cannabis use increased from $31,271 (SD $1333) in 2011 to $38,684 (SD $946) in 2015 (Table 3), with the mean length of hospital stay also increasing from 2012 to 2015. Interestingly, in an analysis of cannabis use and inpatient outcomes among hospitalized patients, Vin-Ravin et al. reported cannabis users as having fewer comorbid conditions on admission (78% vs. 71%) compared to non-users [32]. This led Vin-Ravin et al. to report a significantly reduced odds of in-hospital mortality and morbidity in cannabis users compared with non-cannabis users (odds ratios of 0.41 and 0.44, respectively). This indicates that cannabis use may have some degree of all cause morbidity and mortality benefit among hospitalized patients. The increase in healthcare spending among chronic pain patients using cannabis is difficult to explain based on these previous studies together. We would expect increases in cannabis use to lead to decreases in overall spending; however, our findings show the opposite trend. The disparity in our findings may partly be due to the fact that the majority of cannabis users in the study by Vin-Ravin et al. were < 40 years old, who are less likely to have comorbidities and ultimately have lower health care costs compared with the predominant cannabis users in our study who were between 45 and 64 years old. Moreover, the increased spending among chronic pain patients using cannabis, which we note in our study, may largely be due to an overall trend of increased hospital spending. Our findings are supported by the concept of “super-additive costs” per Cortaredona et al. and may be explained by an increasing trend of older patients having more comorbidities and as a result higher health care utilization and resultant costs [34].
Our study has several limitations. First, the NIS database does not contain variables that can evaluate disease severity. The degree of cannabis use and its relationship to worsening chronic pain was not available for analysis. In addition, the definite relationship between chronic pain and cannabis may not be well established with this administrative data set. We included only chronic pain patients with a history of cannabis use. However, it is very difficult to elucidate the indication for cannabis prescription or consumption among our chronic pain cohort. Cannabis use may be secondary to other medical comorbidity outside of chronic pain. Second, the NIS database does not include detailed comorbid cannabis use disorder-related cost information, but rather total hospital charges. This unfortunately makes specific cost analysis, such as intensive care unit (ICU) admission cost, cost of administered anesthesia, procedure room charges, and postoperative charges, impossible. Third, healthcare utilization outcomes available for analysis in this study may not be directly related to comorbid cannabis use. They could be influenced by multiple factors such as payer status and social factors. Fourth, the NIS database is highly dependent on the selection and accuracy of the appropriate diagnostic ICD codes reported [35]. The rise in concomitant cannabis use may reflect a coding artifact or the implementation of new ICD-9 codes. This makes it is very difficult to determine the actual incidence of cannabis use in hospitalized patients with chronic pain. Furthermore, the criteria used for diagnosis of conditions such as CRPS were not reported in our database. The lack of standardization may affect the quality of our result.
Conclusion
The consequences of a fast-approaching landscape of widespread cannabis legalization may greatly impact the management of chronic pain patients; cannabis may offer a viable therapeutic approach to decreasing opioid dependence. As a whole, our results show that cannabis use is on the rise in patients with chronic pain and can be expected to continue to trend upwards in the face of increasing societal awareness and availability of legal cannabis.
References
Tsang A, Von Korff M, Lee S, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain. 2008;9(10):883–91.
Degenhardt L, Lintzeris N, Campbell G, et al. Experience of adjunctive cannabis use for chronic non-cancer pain: findings from the Pain and Opioids IN Treatment (POINT) study. Drug Alcohol Depend. 2015;147:144–50.
Chou SP, Zhang H, Jung J, Roger P. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;72(12):1235–42.
United Nations Office of Drug Control and Crime Prevention. World Drug Report; 2016.
Wagner FA, Anthony JC. From first drug use to drug dependence; developmental periods of risk for dependence upon marijuana, cocaine, and alcohol. Neuropsychopharmacology. 2002;26(4):479–88.
Martel MO, Shir Y, Ware MA. Substance-related disorders: a review of prevalence and correlates among patients with chronic pain. Prog Neuro-Psychopharmacol Biol Psychiatry. 2017;87:245–54.
Fergusson DM, Boden JM, Horwood LJ. Cannabis use and other illicit drug use: testing the cannabis gateway hypothesis. Addiction. 2006;101(4):556–69.
National Academies of Sciences, Engineering and Medicine. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC; 2017.
Lévesque A, Le Foll B. when and how to treat possible cannabis use disorder. Med Clin N Am. 2018;102(4):667–81.
AHRQ. HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). Rockville.
Rumalla K, Reddy AY, Mittal MK. Recreational marijuana use and acute ischemic stroke: a population-based analysis of hospitalized patients in the United States. J Neurol Sci. 2016;364:191–6.
Rumalla K, Reddy AY, Mittal MK. Association of recreational marijuana use with aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2016;25(2):452–60.
Reinarman C, Nunberg H, Lanthier F, Heddleston T. Who are medical marijuana patients? Population characteristics from nine California assessment clinics. J Psychoactive Drugs. 2011;43(2):128–35.
Ware MA, Adams H, Guy GW. The medicinal use of cannabis in the UK: results of a nationwide survey. Int J Clin Pract. 2005;59(3):291–5.
Pacula RL, Jacobson M, Maksabedian EJ. In the weeds: a baseline view of cannabis use among legalizing states and their neighbours. Addiction. 2016;111(6):973–80.
StataCorp. Stata. 2016.
Boehnke KF, Litinas E, Clauw DJ. Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. J Pain. 2016;17(6):739–44.
Haroutounian S, Ratz Y, Ginosar Y, et al. The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: a prospective open-label study. Clin J Pain. 2016;32(12):1036–43.
Manzanares J, Julian M, Carrascosa A. Role of the cannabinoid system in pain control and therapeutic implications for the management of acute and chronic pain episodes. Curr Neuropharmacol. 2006;4(3):239–57.
Miller RJ, Miller RE. Is cannabis an effective treatment for joint pain? Clin Exp Rheumatol. 2017;35 Suppl 1(5):59–67.
Baron EP. Medicinal properties of cannabinoids, terpenes, and flavonoids in cannabis, and benefits in migraine, headache, and pain: an update on current evidence and cannabis science. Headache J Head Face Pain. 2018;58(7):1139–86.
Wallace JL, Flannigan KL, McKnight W, Wang L, Ferraz JGP, Tuitt D. Pro-resolution, protective and anti-nociceptive effects of a cannabis extract in the rat gastrointestinal tract. J Physiol Pharmacol. 2013;64(2):167–75.
Oláh A, Tóth BI, Borbíró I, et al. Cannabidiol exerts sebostatic and antiinflammatory effects on human sebocytes. J Clin Investig. 2014;124(9):3713–24.
Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: a prevalence study. Pain. 2001;89(2–3):127–34.
Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287.
Moulin DE, Clark AJ, Speechley M, Morley-Forster PK. Chronic pain in Canada—prevalence, treatment, impact and the role of opioid analgesia. Pain Res Manag. 2002;7(4):179–84.
Hill KP, Palastro MD. Medical cannabis for the treatment of chronic pain and other disorders: misconceptions and facts. Polish Arch Intern Med. 2017;127(11):785–9.
Baron EP, Lucas P, Eades J, Hogue O. Patterns of medicinal cannabis use, strain analysis, and substitution effect among patients with migraine, headache, arthritis, and chronic pain in a medicinal cannabis cohort. J Headache Pain. 2018;19(1):37.
Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313(24):2474–83.
Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national results on adolescent drug use: overview of key findings, 2012; 2013.
Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health. Rockville; 2013.
Vin-Raviv N, Akinyemiju T, Meng Q, Sakhuja S, Hayward R. Marijuana use and inpatient outcomes among hospitalized patients: analysis of the nationwide inpatient sample database. Cancer Med. 2017;6(1):320–9.
Zulman DM, Pal Chee C, Wagner TH, et al. Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System. BMJ Open. 2015;5(4):e007771.
Cortaredona S, Ventelou B. The extra cost of comorbidity: multiple illnesses and the economic burden of non-communicable diseases. BMC Med. 2017;15(1):216.
Berthelsen CL. Evaluation of coding data quality of the HCUP National Inpatient Sample. Top Health Inf Manag. 2000;21(2):10–23.
Acknowledgements
Funding
No funding or sponsorship, including departmental and institutional funding, was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Study concept and design: Vwaire Orhurhu, Thomas Simopoulos, Jatinder Gill, Musa Aner. Acquisition of data: Vwaire Orhurhu, Mariam Salisu Orhurhu and Mayowa Olusunmade. Statistical analysis: Vwaire Orhurhu, Mariam Salisu Orhurhu and Mayowa Olusunmade had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Interpretation of data: All authors. Drafting of the manuscript: All authors. Critical revision of the manuscript for important intellectual content: All authors. Study supervision: Vwaire Orhurhu, Jatinder Gill, Thomas Simopoulos, Musa Aner.
Disclosures
Vwaire Orhurhu, Ivan Urits, Mayowa Olusunmade, Akinola Olayinka, Mariam Salisu Orhurhu, Chiedozie Uwandu, Musa Aner, Sebele Ogunsola, Loretta Akpala, Sameer Hirj, Omar Viswanath, Jay Karri, Thomas Simopoulos, and Jatinder Gill have nothing to disclose.
Compliance with Ethics Guidelines
This study uses anonymous patient data from another source and so is exempt from needing ethics approval.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12481829.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Orhurhu, V., Urits, I., Olusunmade, M. et al. Cannabis Use in Hospitalized Patients with Chronic Pain. Adv Ther 37, 3571–3583 (2020). https://doi.org/10.1007/s12325-020-01416-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01416-9