Abstract
Introduction
The purpose of this review is to present the current and emerging treatment alternatives for Leber’s hereditary optic neuropathy (LHON), emphasizing the most recent use of idebenone and stem cells or gene therapy.
Methods
A comprehensive literature review was performed at the PubMed database regarding the various treatment modalities for LHON.
Results
Treatment modalities for LHON include nutritional supplements, activators of mitochondrial biogenesis, brimonidine, and symptomatic and supportive treatment, but nowadays attention is being paid to idebenone and gene therapy or stem cells.
Conclusion
The treatment of LHON remains challenging, given the nature of the disease and its prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Leber’s hereditary optic neuropathy (LHON) is a rare, maternally inherited mitochondrial disease and is considered one of the most common inherited optic neuropathies, caused by a primary mutation in mitochondrial DNA (mtDNA), resulting in optic nerve atrophy and loss of central vision [1, 2]. The 11778G>A/ND4 mutation is by far the most common, accounting for 70% of all LHON cases worldwide. Other known mutations are 3460G>A/ND1 and 14484T>C/ND6, with the latter being preponderant in patients of French Canadian origin [3,4,5,6]. Apart from these, more than 18 mtDNA alterations have been associated with LHON, leading to a dysfunction of complex I of the mitochondrial electron transport chain and consequently to degeneration and apoptotic cell death of retinal ganglion cells (RGCs) due to decreased ATP synthesis and elevated levels of oxidative stress [7,8,9,10].
The incidence of LHON ranges between 1:31,000 and 1:54,000, affecting predominantly males (in 80–90% of cases) with typical onset of symptoms at the 2nd and 3rd decades of life, although there have been reports of LHON onset from 2 to 87 years [11, 12]. It usually presents as painless, subacute, central visual loss in one eye, while the fellow eye becomes involved weeks to months later with a median delay of 6–8 weeks. Since 97% of the affected patients have bilateral involvement within 1 year, if patients present with unilateral optic neuropathy for longer than 1 year they are highly unlikely to suffer from LHON. Dyschromatopsia is also common and usually depends on the degree of visual acuity loss. In addition, pupillary light reflexes usually remain intact because of sparing of a special class of melanopsin-containing RGCs, which seem more resistant to mitochondrial dysfunction [13].
At the clinical examination, the fundus can look entirely normal, while the optic disc is more commonly hyperemic with peripapillary telangiectasias and vascular tortuosity of the central retinal vessels. Optical coherence tomography (OCT) can show swelling of the retinal nerve fiber layer (RNFL), which gradually subsides, and optic atrophy develops with progressive generalized RNFL thinning over the subsequent 6–12 months [14]. The main differential diagnoses of LHON are other inherited optic atrophies, such as dominant optic atrophy and Wolfram syndrome, acquired optic atrophies, optic neuritis, compressive optic neuropathies, metabolic or toxic optic neuropathies, maculopathies and non-organic visual loss [14, 15]. It has to be noted that apart from visual loss, LHON has been associated with cardiac, neurologic and skeletal abnormalities [16].
The visual prognosis in LHON is generally poor, and the majority of patients will end up legally blind with visual acuity of 20/200 or worse and a significant detrimental impact on their quality of life [17, 18]. However, prognosis may range, since spontaneous improvement may occur within the 1st year, but has also been reported several years or even decades after initial visual loss. LHON carriers rarely lose vision after the age of 50 years [13]. Additionally, LHON carriers harboring the 14484T>C mutation have the best visual prognosis with a partial visual recovery rate of 37–58% compared with 4–25% for the 11778G>A mutation [13, 19]. Other positive prognostic factors for visual recovery may include an earlier age of onset, subacute presentation with slow visual deterioration and a relatively large optic disc [20].
Several treatment modalities have been proposed for LHON, including nutritional supplements, activators of mitochondrial biogenesis, phytoestrogens, hyperbaric oxygen therapy, and symptomatic and supportive treatment [21, 22]. Recently, idebenone has gained scientific interest for the treatment of LHON, along with gene therapies [23, 24]. In light of the above, the purpose of this review is to present the current and emerging treatment alternatives for LHON, emphasizing the most recent use of idebenone and gene therapy or stem cells.
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Treatment Modalities for LHON
Traditional Treatment and Supportive Approaches
Traditional treatment and supportive approaches include nutritional supplements, activators of mitochondrial biogenesis, brimonidine, phytoestrogens, cyclosporine A, low vision aids, and change in nutritional and environmental factors, with several options seen as more fringe—a testament to the prior lack of an effective treatment option.
Nutritional Supplements
Several combinations of vitamins (B2, B3, B12, C, E and folic acid), coenzyme Q10 and other supplements, such as alpha-lipoic acid, carnitine, creatine, l-arginine and dichloroacetate, have been tried for the treatment of mitochondrial disorders, including LHON. The rationale for using nutritional supplements is to increase mitochondrial respiration and simultaneously scavenge free radicals to reduce reactive oxygen species (ROS) and toxic acyl coenzyme A molecules, which are produced in mitochondrial diseases. Moreover, some supplements act as alternate energy fuels and possibly bypass the block within the respiratory chain complexes. However, the benefit of the above-mentioned treatment alternatives in patients with LHON remains limited and variable [25, 26].
Activators of Mitochondrial Biogenesis
Mitochondrial biogenesis is the process by which cells increase their individual mitochondrial mass and copy number to increase the production of ATP as a response to greater energy expenditure. Since increased mitochondrial biogenesis has been significantly associated with unaffected LHON mutation carriers and may have a protective effect, activators of mitochondrial biogenesis have been tried for the treatment of LHON [27]. Specifically, mitochondrial biogenesis is partly regulated by the transcriptional activator PGC-1a, which is controlled by peroxisome proliferator-activated receptors and AMP-activated protein kinase [28]. Pharmacologic activators of these proteins include fibrates, rosiglitazone, metformin and 5-aminoimidazole-4-carboxamide ribonucleoside (AICAR) [29]. However, it remains to be proven whether pharmaceutical activation of PGC-1a will be effective for the treatment of LHON-affected patients or mutation carriers.
Brimonidine
Brimonidine is a topical a2-agonist, with known neuroprotective action, which is used for the treatment of glaucoma and has been shown to protect RGCs from oxidative damage in animal models [30]. Although the drug was not effective in preventing visual loss in the fellow eye of patients with monocular visual loss, its neuroprotective properties enhance the potential of being a good treatment alternative for unaffected LHON carriers diagnosed with glaucoma or ocular hypertension, as raised intraocular pressure has been associated with an increased risk of visual loss in LHON [31, 32].
Phytoestrogens
Studies have shown that targeting estrogen receptor β by using phytoestrogens may become a therapeutic strategy for LOHN, trying to avoid or delay the onset of the disease in mutation careers. It seems that these molecules improve cell viability by reducing apoptosis, inducing mitochondrial biogenesis and strongly reducing the levels of ROS in LHON cells [33].
Cyclosporin A
Pre-treatment with cyclosporin A blunted the deleterious consequences of hydrogen peroxide by blocking the MTP pore, indicating a possible therapeutic pathway for LHON. The antiapoptotic effect of cyclosporine A has also been demonstrated in LHON cybrids harboring the m.14484T4C and m.14279G4A mutations [34].
Symptomatic and Supportive Treatments
Low vision aids may benefit patients with severe vision loss. In particular, patients with LHON are often young adults with preserved peripheral vision, who make excellent candidates for low vision rehabilitation. Patients should also be counseled to optimize environmental risk factors for vision loss by avoiding tobacco use, heavy alcohol consumption, cyanide-containing products, medications with mitochondrial toxicity and exposure to environmental toxins, especially during the acute phase of visual loss [25].
Fringe Treatment Modalities
Near-infrared light therapy has been shown to improve mitochondrial function and cellular survival in various experimental models. Although these findings are not universally accepted and the mechanisms are not fully understood, near-infrared light is thought to increase ATP synthesis by stimulating the activity of cytochrome c oxidase (complex IV) [35]. In LHON, although a study conducted to investigate the visual benefit of this therapy in affected LHON carriers failed, it could be considered as a possible rescue treatment strategy [36].
There is some “internet” evidence that hyperbaric oxygen has helped patients with LOHN. In this therapy, increased levels of oxygen are provided to RGCs during the acute phase of LOHN, aiming at improving mitochondrial biogenesis. However, it seems to be a controversial treatment modality, and the theoretical toxic effects of supra-physiologic levels of oxygen in LHON should be considered in the context of a dysfunctional mitochondrial respiratory chain, which is already producing increased ROS levels [20].
Novel Therapies for LHON
Novel therapies for LHON include idebenone and quinine analogs as well as the most recent gene therapy and stem cells.
Idebenone and Quinone Analogs
Ubiquinone, known as coenzyme Q10 (CoQ), is a lipophilic electron carrier and endogenous antioxidant found in all cellular membranes. Specifically, in the mitochondrial inner membrane ubiquinone transfers electrons to complex III of the electron transport chain. Idebenone [2,3-dimethoxy-5-methyl-6-(10hydroxydecyl)-1,4-benzoquinone] is a human-made short-chain CoQ analog, which is considered for use as a CoQ replacement. The mechanism of action of idebenone involves its antioxidant properties and ability to act as a mitochondrial electron carrier, overcoming mitochondrial complex I respiratory chain deficiency in patients with LHON by transferring electrons directly to mitochondrial complex III (bypassing complex I), thereby restoring cellular energy (ATP) production and reactivating inactive-but-viable RGCs, which ultimately prevents further vision loss and promotes vision recovery. Although championed as an antioxidant, idebenone can also act as a prooxidant by forming an unstable semiquinone at complex I [37].
In vitro studies of RGC deficiency in complex I demonstrated a protective role of idebenone against cell death [38], while in the past patients with LHON reported improvement in vision following treatment with the short-chain synthetic benzoquinone [39, 40]. Until 2011, since no randomized clinical trials were performed regarding idebenone for the treatment of LHON, patients were initially treated “off label,” and only isolated case reports or small retrospective studies were published [39,40,41,42,43].
Carelli et al. retrospectively reviewed a cohort of idebenone-treated patients with LHON (44 patients) and compared them with 59 untreated patients with LHON. All patients were older than 10 years within 1 year of the onset of visual loss, because this is the frame to reach the nadir of the visual loss, and had undergone at least 5 years of follow-up. The 11,778 patients had an earlier onset of recovery and longer duration of therapy. Furthermore, all patients treated with idebenone prior to second eye involvement had an apparent delay in visual loss in the second eye, although all second eyes were involved or got worse regarding their final visual function [44].
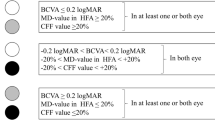
The first randomized study using idebenone for the treatment of LHON, called RHODOS (Rescue of Hereditary Optic Disease Outpatient Study), was a 24-week, multi-center, double-blind, randomized, placebo-controlled trial. The study included 85 patients with LHON due to m.3460G>A, m.11778G>A and m.14484T>C or mitochondrial DNA mutations who described loss of vision within 5 years and received idebenone 900 mg/day [45]. The study did not show any benefit for the primary outcome of best recovery of visual acuity after 24 weeks. However, it provided evidence that patients with discordant visual acuities are the most likely to benefit from idebenone treatment, which was safe and well tolerated; discordant means that the visual acuity was different between the two eyes of a patient, which is usually observed in early stages of the condition. For these patients, there was a 45% difference in the responders for the best recovery of visual acuity (P = 0.024) and a 32.5% difference in the end point assessing the change in visual acuity for all eyes (P = 0.011). The study also found that patients with the 11,778 or 3460 mutation presented the largest treatment effect, while those with the 14,484 mutation had a high spontaneous recovery rate in the placebo group [45]. The patients of this trial were followed up for 30 months after termination of treatment (RHODOS-OFU study), and it was found that the beneficial effect from the 6-month treatment with idebenone persisted despite discontinuation of therapy [46]. Moreover, a sub-analysis of the RHODOS trial, including 39 LHON patients with disease duration < 5 years, revealed a significant improvement in the tritan color contrast (blue-yellow color domain) in the idebenone group at 12 and 24 weeks [47].
Recently, in the International Consensus on the clinical and therapeutic management of LHON, idebenone was proposed to be started as soon as possible at 900 mg/day and to be continued at least 1 year in patients with disease < 1 year. Furthermore, there is not enough evidence to recommend treatment in chronic patients between 1- and 5-year duration (after the second eye onset) and no evidence to recommend treatment in chronic patients older than 5 years after the second eye onset [48].
Additionally, EPI-743 is structurally similar to CoQ10 and idebenone with a modified benzene ring to improve efficiency by 1000- to 10,000-fold compared with either drug in accepting electrons to reduce oxidative stress while improving mitochondrial function. EPI-743 works by interacting with the enzyme NADPH quinone reductase (NQO1) to form stable hydroquinones with excellent antioxidant properties [49]. The initial results from EPI-743 appear promising, since four out of five LHON patients with different mtDNA mutations showed an improvement in visual recovery based on various tests, such as visual acuity, field, color vision and other metrics, without developing any adverse effects [50].
Gene Therapy
Gene therapy, in which the defective gene is replaced by the normal wild-type gene so that the normal gene is expressed, has shown some promise for mitochondrial diseases. For LHON in particular, it is an even more appealing treatment option because the RGC layer in the retina can be easily accessed, while LHON offers a unique “laboratory” for the investigation of new interventions in mitochondrial disease [51]. Since LHON vision loss often occurs in a bilateral sequential fashion, a window of opportunity exists for possible therapeutic intervention after vision loss in the first eye but before second eye involvement [52]. However, the double-membrane nature of mitochondria presents a formidable series of technical challenges that need to be overcome [51]. As a result, a highly efficient vector, such as the adeno-associated virus (AAV), is needed to penetrate the relatively impermeable inner mitochondrial membrane, bypassing the mitochondrial genome altogether, so as to successfully integrate the normal gene into the mitochondrial genome [51].
The potential of the gene therapy approach was first demonstrated in m.11778G>A LHON cybrids [53]. Due to the difficulty of inserting a gene directly into mitochondria, the principle of allotopic gene expression was used. In this technique, the gene construct is inserted into the nuclear genome, and the resulting protein has a mitochondrial targeting sequence, which then allows its import into the mitochondrial compartment. Specifically, rescue of a mutant mouse model of LHON by AAV vector containing wild-type allotopic ND4 was successful, with preserved vision, restoration of ATP synthesis, and prevention of loss of RGCs and optic nerve axons [54]. Moreover, in a rat model of LHON, Cwerman-Thibault et al. demonstrated the safety and efficacy of allotopic expression of wild-type human ND4 introduced by a recombinant AAV2/2 vector containing ND4, providing further evidence that gene therapy through allotopic expression in humans may be useful for LHON [55]. Gene therapy has also been implemented in humans. Wan et al. conducted a clinical trial, which showed improvement in visual acuity in six of nine LHON patients at the 9-month follow-up without complications during or after the procedure [56]. Accordingly, Guy et al. showed favorable results in patients with LHON using low and medium doses of allotopic gene therapy, suggesting that high doses should also have been tested [57], while other authors supported these findings [58, 59].
Stem Cells
The Stem Cell Ophthalmology Treatment Study (SCOTS) utilizes autologous bone-marrow-derived stem cells to treat optic nerve and retinal diseases. Patients with LHON had visual acuity gains of up to 35 letters and Snellen acuity improvements from hand motion to 20/200 and from counting fingers to 20/100, while visual field improvement was also noticed without serious complications [60]. However, further research is needed to examine the role of stem cells in the treatment of LHON.
Conclusions
LHON is a rare disease, characterized by the degeneration of RGCs, involving bilateral visual loss with poor prognosis. The disease is expressed because of mitochondrial mutations, but several risk factors have also been involved. Regarding treatment, there are many suggested therapies with variable outcomes, while the most recent idebenone and gene therapy or stem cells have provided encouraging results, leading to a new era, where LHON will no longer be faced as an incurable disease.
References
Bi R, Logan I, Yao YG. Leber hereditary optic neuropathy: a mitochondrial disease unique in many ways. Handb Exp Pharmacol. 2017;240:309–36.
Jancic J, Samardzic J, Stojanovic S, Stojanovic A, Milanovic AM, Nikolic B, Ivancevic N, Kostic V. Leber’s hereditary optic neuropathy: novel views and persisting challenges. CNS Neurol Disord Drug Targets. 2017;16:927–35.
Dai Y, Wang C, Nie Z, Han J, Chen T, Zhao X, Ai C, Ji Y, Gao T, Jiang P. Mutation analysis of Leber’s hereditary optic neuropathy using a multi-gene panel. Biomed Rep. 2018;8:51–8.
Lu Q, Guo Y, Yi J, Deng X, Yang Z, Yuan X, Deng H. Identification of an ND4 mutation in leber hereditary optic neuropathy. Optom Vis Sci. 2017;94:1090–4.
Wallace DC, Lott MT. Leber hereditary optic neuropathy: exemplar of an mtDNA disease. Handb Exp Pharmacol. 2017;240:339–76.
Dimitriadis K, Leonhardt M, Yu-Wai-Man P, Kirkman MA, Korsten A, De Coo IF, Chinnery PF, Klopstock T. Leber’s hereditary optic neuropathy with late disease onset: clinical and molecular characteristics of 20 patients. Orphanet J Rare Dis. 2014;9:158.
Jørstad ØK, Ødegaard EM, Heimdal KR, Kerty E, Heimdal KR, Kerty E. Leber hereditary optic neuropathy caused by a mitochondrial DNA 10663T>C point mutation and its response to idebenone treatment. J Neuroophthalmol. 2018;38:129–31.
Majander A, Robson AG, João C, Holder GE, Chinnery PF, Moore AT, Votruba M, Stockman A, Yu-Wai-Man P. The pattern of retinal ganglion cell dysfunction in Leber hereditary optic neuropathy. Mitochondrion. 2017;36:138–49.
González-Martín-Moro J, Castro-Rebollo M, Contreras I, Pérez-Sarriegui A. Subclinical thinning of macular ganglion cell layer in Leber optic neuropathy carriers. Clin Exp Optom. 2018;101:406–11. https://doi.org/10.1111/cxo.12634.
Hayashi G, Cortopassi G. Oxidative stress in inherited mitochondrial diseases. Free Radic Biol Med. 2015;88:10–7.
Yu-Wai-Man P, Griffiths PG, Brown DT, Howell N, Turnbull DM, Chinnery PF. The epidemiology of Leber hereditary optic neuropathy in the North East of England. Am J Hum Genet. 2003;72:333–9.
Rosenberg T, Nørby S, Schwartz M, Saillard J, Magalhães PJ, Leroy D, Kann EC, Duno M. Prevalence and genetics of Leber hereditary optic neuropathy in the Danish population. Invest Ophthalmol Vis Sci. 2016;57:1370–5.
Meyerson C, Van Stavern G, McClelland C. Leber hereditary optic neuropathy: current perspectives. Clin Ophthalmol. 2015;9:1165–76.
Grzybowski A, Zülsdorff M, Wilhelm H, Tonagel F. Toxic optic neuropathies: an updated review. Acta Ophthalmol. 2015;93:402–10.
Chun BY, Rizzo JF 3rd. Dominant optic atrophy and Leber’s hereditary optic neuropathy: update on clinical features and current therapeutic approaches. Semin Pediatr Neurol. 2017;24:129–34.
Orssaud C. Cardiac disorders in patients with Leber hereditary optic neuropathy. J Neuroophthalmol. 2018. https://doi.org/10.1097/wno.0000000000000623 (in press).
Yu-Wai-Man P. Therapeutic approaches to inherited optic neuropathies. Semin Neurol. 2015;35:578–86.
Kirkman MA, Korsten A, Leonhardt M, Dimitriadis K, De Coo IF, Klopstock T, Griffiths PG, Hudson G, Chinnery PF, Yu-Wai-Man P. Quality of life in patients with Leber hereditary optic neuropathy. Invest Ophthalmol Vis Sci. 2009;50:3112–5.
Johns DR, Heher KL, Miller NR, Smith KH. Leber’s hereditary optic neuropathy. Clinical manifestations of the 14484 mutation. Arch Ophthalmol. 1993;111:495–8.
Yu-Wai-Man P, Votruba M, Moore AT, Chinnery PF. Treatment strategies for inherited optic neuropathies: past, present and future. Eye. 2014;28:521–37.
Peragallo JH, Newman NJ. Is there treatment for Leber hereditary optic neuropathy? Curr Opin Ophthalmol. 2015;26:450–7.
Manickam AH, Michael MJ, Ramasamy S. Mitochondrial genetics and therapeutic overview of Leber’s hereditary optic neuropathy. Indian J Ophthalmol. 2017;65:1087–92.
Karanjia R, Chahal J, Ammar M, Sadun AA. Treatment of Leber’s hereditary optic neuropathy. Curr Pharm Des. 2017;23:624–8.
Le Meur G, Lebranchu P, Billaud F, Adjali O, Schmitt S, Bézieau S, Péréon Y, Valabregue R, Ivan C, Darmon C, Moullier P, Rolling F, Weber M. Safety and long-term efficacy of AAV4 gene therapy in patients with RPE65 Leber congenital amaurosis. Mol Ther. 2018;26:256–68.
Newman NJ. Treatment of Leber hereditary optic neuropathy. Brain. 2011;134:2447–50.
Iyer S. Novel therapeutic approaches for Leber’s hereditary optic neuropathy. Discov Med. 2013;15:141–9.
Giordano C, Iommarini L, Giordano L, Maresca A, Pisano A, Valentino ML, Caporali L, Liguori R, Deceglie S, Roberti M, Fanelli F, Fracasso F, Ross-Cisneros FN, D’Adamo P, Hudson G, Pyle A, Yu-Wai-Man P, Chinnery PF, Zeviani M, Salomao SR, Berezovsky A, Belfort R Jr, Ventura DF, Moraes M, Moraes Filho M, Barboni P, Sadun F, De Negri A, Sadun AA, Tancredi A, Mancini M, d’Amati G, Loguercio Polosa P, Cantatore P, Carelli V. Efficient mitochondrial biogenesis drives incomplete penetrance in Leber’s hereditary optic neuropathy. Brain. 2014;137:335–53.
Wenz T, Williams SL, Bacman SR, Moraes CT. Emerging therapeutic approaches to mitochondrial diseases. Dev Disabil Res Rev. 2010;16:219–29.
La Morgia C, Carbonelli M, Barboni P, Sadun AA, Carelli V. Medical management of hereditary optic neuropathies. Front Neurol. 2014;5:141.
Saylor M, McLoon LK, Harrison AR, Lee MS. Experimental and clinical evidence for brimonidine as an optic nerve and retinal neuroprotective agent. Arch Ophthalmol. 2009;127:402–6.
Newman NJ, Biousse V, David R, Bhatti MT, Hamilton SR, Farris BK, Lesser RL, Newman SA, Turbin RE, Chen K, Keaney RP. Prophylaxis for second eye involvement in Leber hereditary optic neuropathy: an open-labeled, nonrandomized multicenter trial of topical brimonidine purite. Am J Ophthalmol. 2005;140:407–15.
Thouin A, Griffiths PG, Hudson G, Chinnery PF, Yu-Wai-Man P. Raised intraocular pressure as a potential risk factor for visual loss in Leber hereditary optic neuropathy. PLoS ONE. 2013;8:e63446.
Pisano A, Preziuso C, Iommarini L, Perli E, Grazioli P, Campese AF, Maresca A, Montopoli M, Masuelli L, Sadun AA, d’Amati G, Carelli V, Ghelli A, Giordano C. Targeting estrogen receptor β as preventive therapeutic strategy for Leber’s hereditary optic neuropathy. Hum Mol Genet. 2015;24:6921–31.
Porcelli AM, Angelin A, Ghelli A, Mariani E, Martinuzzi A, Carelli V, Petronilli V, Bernardi P, Rugolo M. Respiratory complex I dysfunction due to mitochondrial DNA mutations shifts the voltage threshold for opening of the permeability transition pore toward resting levels. J Biol Chem. 2009;284:2045–52.
Desmet KD, Paz DA, Corry JJ, Eells JT, Wong-Riley MT, Henry MM, Buchmann EV, Connelly MP, Dovi JV, Liang HL, Henshel DS, Yeager RL, Millsap DS, Lim J, Gould LJ, Das R, Jett M, Hodgson BD, Margolis D, Whelan HT. Clinical and experimental applications of NIR-LED photobiomodulation. Photomed Laser Surg. 2006;24:121–8.
Gueven N, Faldu D. Therapeutic strategies for Leber’s hereditary optic neuropathy: a current update. Intractable Rare Dis Res. 2013;2:130–5.
Jaber S, Polster BM. Idebenone and neuroprotection: antioxidant, pro-oxidant, or electron carrier? J Bioenerg Biomembr. 2015;47:111–8.
Heitz FD, Erb M, Anklin C, et al. Idebenone protects against retinal damage and loss of vision in a mouse mode of Leber’s hereditary optic neuropathy. PLoS ONE. 2012;7:e45182.
Mashima Y, Hiida Y, Oguchi Y. Remission of Leber’s hereditary optic neuropathy with idebenone. Lancet. 1992;340:368–9.
Carelli V, Barboni P, Zacchini A, Mancini R, Monari L, Cevoli S, Liguori R, Sensi M, Lugaresi E, Montagna P. Leber’s hereditary optic neuropathy (LHON) with 14484/ND6 mutation in a North African patient. J Neurol Sci. 1998;160:183–8.
Cortelli P, Montagna P, Pierangeli G, Lodi R, Barboni P, Liguori R, Carelli V, Iotti S, Zaniol P, Lugaresi E, Barbiroli B. Clinical and brain bioenergetics improvement with idebenone in a patient with Leber’s hereditary optic neuropathy: a clinical and 31P-MRS study. J Neurol Sci. 1997;148:25–31.
Mashima Y, Kigasawa K, Wakakura M, Oguchi Y. Do idebenone and vitamin therapy shorten the time to achieve visual recovery in Leber hereditary optic neuropathy? J Neuroophthalmol. 2000;20:166–70.
Barnils N, Mesa E, Muñoz S, Ferrer-Artola A, Arruga J. Response to idebenone and multivitamin therapy in Leber’s hereditary optic neuropathy. Arch Soc Esp Oftalmol. 2007;82:377–80.
Carelli V, La Morgia C, Valentino ML, Rizzo G, Carbonelli M, De Negri AM, Sadun F, Carta A, Guerriero S, Simonelli F, Sadun AA, Aggarwal D, Liguori R, Avoni P, Baruzzi A, Zeviani M, Montagna P, Barboni P. Idebenone treatment in Leber’s hereditary optic neuropathy. Brain. 2011;134:e18.
Klopstock T, Yu-Wai-Man P, Dimitriadis K, Rouleau J, Heck S, Bailie M, Atawan A, Chattopadhyay S, Schubert M, Garip A, Kernt M, Petraki D, Rummey C, Leinonen M, Metz G, Griffiths PG, Meier T, Chinnery PF. A randomized placebo-controlled trial of idebenone in Leber’s hereditary optic neuropathy. Brain. 2011;134:2677–86.
Klopstock T, Metz G, Yu-Wai-Man P, Büchner B, Gallenmüller C, Bailie M, Nwali N, Griffiths PG, von Livonius B, Reznicek L, Rouleau J, Coppard N, Meier T, Chinnery PF. Persistence of the treatment effect of idebenone in Leber’s hereditary optic neuropathy. Brain. 2013;136:e230.
Rudolph G, Dimitriadis K, Büchner B, Heck S, Al-Tamami J, Seidensticker F, Rummey C, Leinonen M, Meier T, Klopstock T. Effects of idebenone on color vision in patients with Leber hereditary optic neuropathy. J Neuroophthalmol. 2013;33:30–6.
Carelli V, Carbonelli M, de Coo IF, Kawasaki A, Klopstock T, Lagrèze WA, La Morgia C, Newman NJ, Orssaud C, Pott JWR, Sadun AA, van Everdingen J, Vignal-Clermont C, Votruba M, Yu-Wai-Man P, Barboni P. International consensus statement on the clinical and therapeutic management of Leber hereditary optic neuropathy. J Neuroophthalmol. 2017;37:371–81.
Iyer S. Novel therapeutic approaches for Leber’s hereditary optic neuropathy. Discov Med. 2013;15:141–9.
Sadun AA, Chicani CF, Ross-Cisneros FN, Barboni P, Thoolen M, Shrader WD, Kubis K, Carelli V, Miller G. Effect of EPI-743 on the clinical course of the mitochondrial disease Leber hereditary optic neuropathy. Arch Neurol. 2012;69:331–8.
Yu-Wai-Man P. Therapeutic approaches to inherited optic neuropathies. Semin Neurol. 2015;35:578–86.
Newman NJ. Hereditary optic neuropathies: from the mitochondria to the optic nerve. Am J Ophthalmol. 2005;140:517–23.
Guy J, Qi X, Pallotti F, Schon EA, Manfredi G, Carelli V, Martinuzzi A, Hauswirth WW, Lewin AS. Rescue of a mitochondrial deficiency causing Leber hereditary optic neuropathy. Ann Neurol. 2002;52:534–42.
Koilkonda RD, Yu H, Chou TH, Feuer WJ, Ruggeri M, Porciatti V, Tse D, Hauswirth WW, Chiodo V, Boye SL, Lewin AS, Neuringer M, Renner L, Guy J. Safety and effects of the vector for the Leber hereditary optic neuropathy gene therapy clinical trial. JAMA Ophthalmol. 2014;132:409–20.
Cwerman-Thibault H, Augustin S, Lechauve C, Ayache J, Ellouze S, Sahel JA, Corral-Debrinski M. Nuclear expression of mitochondrial ND4 leads to the protein assembling in complex I and prevents optic atrophy and visual loss. Mol Ther Methods Clin Dev. 2015;2:15003.
Wan X, Pei H, Zhao MJ, Yang S, Hu WK, He H, Ma SQ, Zhang G, Dong XY, Chen C, Wang DW, Li B. Efficacy and safety of rAAV2-ND4 treatment for Leber’s hereditary optic neuropathy. Sci Rep. 2016;6:21587.
Guy J, Feuer WJ, Davis JL, Porciatti V, Gonzalez PJ, Koilkonda RD, Yuan H, Hauswirth WW, Lam BL. Gene therapy for Leber hereditary optic neuropathy: low-and medium-dose visual results. Ophthalmology. 2017;124:1621–34.
Vignal C, Uretsky S, Fitoussi S, Galy A, Blouin L, Girmens JF, Bidot S, Thomasson N, Bouquet C, Valero S, Meunier S, Combal JP, Gilly B, Katz B, Sahel JA. Safety of rAAV2/2-ND4 gene therapy for Leber hereditary optic neuropathy. Ophthalmology. 2018;125:945–47.
DeBusk A, Moster ML. Gene therapy in optic nerve disease. Curr Opin Ophthalmol. 2018;29:234–8.
Weiss JN, Levy S, Benes SC. Stem Cell Ophthalmology Treatment Study (SCOTS): bone marrow-derived stem cells in the treatment of Leber’s hereditary optic neuropathy. Neural Regen Res. 2016;11:1685–94.
Acknowledgements
Funding
No funding or sponsorship was received for publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole and have given final approval to the version to be published.
Disclosures
A. Theodorou-Kanakari, S. Karampitianis, V. Karageorgou, E. Kampourelli, E. Kapasakis, G. Theodossiadis, P. Theodossiadis and I. Chatziralli have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no data sets were generated or analyzed during the current study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.6965006.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Theodorou-Kanakari, A., Karampitianis, S., Karageorgou, V. et al. Current and Emerging Treatment Modalities for Leber’s Hereditary Optic Neuropathy: A Review of the Literature. Adv Ther 35, 1510–1518 (2018). https://doi.org/10.1007/s12325-018-0776-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-018-0776-z