Abstract
Introduction
Mesh-related complications especially after vaginal implantation have raised awareness lately because of severe adverse reactions and legal aspects. About 20% of patients suffer from complications after mesh insertion in the anterior vaginal wall. Autologous plasma coating of meshes prior to implantation has shown potential to improve the biocompatibility of meshes in vivo and in vitro. This innovative approach has been developed according to the IDEAL recommendations for surgical innovations. The method has still to be assessed at stage 3 accordingly.
Methods
A protocol is developed for a prospective single-blinded randomized controlled phase II trial for biocompatibility optimization of anterior vaginal meshes for prolapse repair by autologous plasma coating versus non-coated meshes.
Results
The protocol aims at fulfilling the requirements for stage 3 (assessment) according to IDEAL. Eligible for inclusion are women with primary cystocele, requiring a surgical procedure, suitable for randomization, and willing to be randomized. Participants will be followed up by postal questionnaires (6 months post surgery and 12 months post randomization) and will also be reviewed in clinic 12 and 24 months post surgery. Primary endpoint is the assessment of mesh-related complications following the Clavien–Dindo classifications. QoL, sexual function assessment, efficacy, and validation of an already developed long-term register are considered secondary endpoints. To afford a calculated 10% reduction of postoperative complications through plasma-coated meshes vs. non-coated meshes at 1-year follow-up, a total 214 women in each arm will be necessary to achieve 80% power at a significance level of 5%.
Conclusion
The protocol for this randomized clinical trial represents the conditions to assess the surgical innovation of plasma coating of meshes in order to improve the meshes’ biocompatibility at stage 3 according to the IDEAL recommendations.


Similar content being viewed by others
References
McCulloch P, Altman DG, Campbell WB, et al. No surgical innovation without evaluation: the IDEAL recommendations. Lancet. 2009;374(9695):1105–12. doi:10.1016/S0140-6736(09)61116-8.
Ergina PL, Cook JA, Blazeby JM, et al. Challenges in evaluating surgical innovation. Lancet. 2009;374(9695):1097–104. doi:10.1016/S0140-6736(09)61086-2.
Barkun JS, Aronson JK, Feldman LS, et al. Evaluation and stages of surgical innovations. Lancet. 2009;374(9695):1089–96.
Sedrakyan A, Campbell B, Merino JG, Kuntz R, Hirst A, McCulloch P. IDEAL-D: a rational framework for evaluating and regulating the use of medical devices. BMJ. 2016;353:i2372.
Vitale SG, Lagana AS, Gulino FA, Tropea A, Tarda S. Prosthetic surgery versus native tissue repair of cystocele: literature review. Updates Surg. 2016;68(4):325–9. doi:10.1007/s13304-015-0343-y.
UPDATE on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse: FDA safety communication hwfgMSAuh. https://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM262760.pdf. Accessed 1 Jan 2017.
FDA Gastroenterology-Urology Medical Devices Advisory Committee Panel. Reclassification of orogynecologic surgical mesh instrumentation. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/MedicalDevices/MedicalDevicesAdvisoryCommittee/Gastroenterology-UrologyDevicesPanel/UCM487224.pdf. Accessed 1 Jan 2017.
Junge K, Rosch R, Klinge U, et al. Titanium coating of a polypropylene mesh for hernia repair: effect on biocompatibilty. Hernia. 2005;9(2):115–9.
Lukasiewicz A, Skopinska-Wisniewska J, Marszalek A, Molski S, Drewa T. Collagen/Polypropylene composite mesh biocompatibility in abdominal wall reconstruction. Plast Reconstr Surg. 2013;131(5):731e–40e. doi:10.1097/PRS.0b013e3182865d2c.
Sedrakyan A. Metal-on-metal failures–in science, regulation, and policy. Lancet. 2012;379(9822):1174–6. doi:10.1016/S0140-6736(12)60372-9.
Chatterjee S, Herrmann HC, Wilensky RL, et al. Safety and procedural success of left atrial appendage exclusion with the lariat device: a systematic review of published reports and analytic Review of the FDA MAUDE Database. JAMA Intern Med. 2015;175(7):1104–9.
Kramer DB, Xu S, Kesselheim AS. How does medical device regulation perform in the United States and the European Union? A systematic review. PLoS Med. 2012;9(7):e1001276.
Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW, National Joint Registry of E, et al. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012;379(9822):1199–204.
Lilford RJ, Braunholtz DA, Greenhalgh R, Edwards SJ. Trials and fast changing technologies: the case for tracker studies. BMJ. 2000;320(7226):43–6.
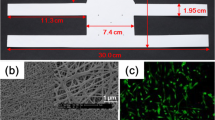
Gerullis H, Georgas E, Eimer C, et al. Evaluation of biocompatibility of alloplastic materials: development of a tissue culture in vitro test system. Surg Technol Int. 2011;21:21–7.
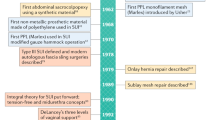
Gerullis H, Klosterhalfen B, Boros M, et al. IDEAL in meshes for prolapse, urinary incontinence, and hernia repair. Surg Innov. 2013;20(5):502–8.
Gerullis H, Georgas E, Eimer C, et al. Coating with autologous plasma improves biocompatibility of mesh grafts in vitro: development stage of a surgical innovation. Biomed Res Int. 2013;2013:536814.
Gerullis H, Georgas E, Boros M, et al. Inflammatory reaction as determinant of foreign body reaction is an early and susceptible event after mesh implantation. Biomed Res Int. 2014;2014:510807.
McCulloch P. The IDEAL recommendations and urological innovation. World J Urol. 2011;29(3):331–6.
Gerullis H, Barski D, Ecke TH, et al. Autologous plasma coating improves the biocompatibility of mesh implants. On the IDEAL way from bench to bedside. Int J Surg. 2016; 36(Suppl 2):S142. doi:10.1016/j.ijsu.2016.11.050.
Barski D, Gerullis H, Georgas E, et al. Coating of mesh grafts for prolapse and urinary incontinence repair with autologous plasma: exploration stage of a surgical innovation. Biomed Res Int. 2014;2014:296498. doi:10.1155/2014/296498.
Barski D, Gerullis H, Ecke TH, et al. In: Register of urogynecological implants: the development of an online platform for registration and outcome measurement according to the IDEAL long-term stage of surgical innovation. Int J Surg 2016;36(Suppl 2):S141–2. doi:10.1016/j.ijsu.2016.11.048.
Chan AW, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–7.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Rogers RG, Rockwood TH, Constantine ML, et al. A new measure of sexual function in women with pelvic floor disorders (PFD): the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire, IUGA-Revised (PISQ-IR). Int Urogynecol J. 2013;24(7):1091–103.
Trutnovsky G, Nagele E, Ulrich D, et al. German translation and validation of the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire-IUGA revised (PISQ-IR). Int Urogynecol J. 2016;27(8):1235–44.
Barski D, Otto T, Gerullis H. Systematic review and classification of complications after anterior, posterior, apical, and total vaginal mesh implantation for prolapse repair. Surg Technol Int. 2014;XXIV:217–24.
Haylen BT, Freeman RM, Swift SE, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Neurourol Urodyn. 2011;30(1):2–12.
Lenz F, Stammer H, Brocker K, Rak M, Scherg H, Sohn C. Validation of a German version of the P-QOL Questionnaire. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(6):641–9.
Bump RC, Mattiasson A, Bo K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012079.
Agha R, Fowler AJ, Limb C, et al. The first 500 registrations to the Research Registry®: advancing registration of under-registered study types. Front Surg. 2016;3:50.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Chapman SJ, Shelton B, Mahmood H, Fitzgerald JE, Harrison EM, Bhangu A. Discontinuation and non-publication of surgical randomised controlled trials: observational study. BMJ. 2014;349:g6870.
Vitale SG, Caruso S, Rapisarda AM, et al. Biocompatible porcine dermis graft to treat severe cystocele: impact on quality of life and sexuality. Arch Gynecol Obstet. 2016;293(1):125–31.
Ware JE Jr, Kosinski M, Gandek B, et al. The factor structure of the SF-36 health survey in 10 countries: results from the IQOLA Project. international quality of life assessment. J Clin Epidemiol. 1998;51(11):1159–65.
de Tayrac R, Alves A, Therin M. Collagen-coated vs noncoated low-weight polypropylene meshes in a sheep model for vaginal surgery. A pilot study. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(5):513–20.
Lo TS, Tan YL, Khanuengkitkong S, Dass AK, Cortes EF, Wu PY. Assessment of collagen-coated anterior mesh through morphology and clinical outcomes in pelvic reconstructive surgery for pelvic organ prolapse. J Minim Invasive Gynecol. 2014;21(5):753–61.
Feola A, Endo M, Urbankova I, et al. Host reaction to vaginally inserted collagen containing polypropylene implants in sheep. Am J Obstet Gynecol. 2015;212(4):474 (e1–8).
Darzi S, Urbankova I, Su K, et al. Tissue response to collagen containing polypropylene meshes in an ovine vaginal repair model. Acta Biomater. 2016;39:114–23.
Cervigni M, Natale F, La Penna C, Saltari M, Padoa A, Agostini M. Collagen-coated polypropylene mesh in vaginal prolapse surgery: an observational study. Eur J Obstet Gynecol Reprod Biol. 2011;156(2):223–7.
Lo TS, Cortes EF, Wu PY, Tan YL, Al-Kharabsheh A, Pue LB. Assessment of collagen versus non collagen coated anterior vaginal mesh in pelvic reconstructive surgery: prospective study. Eur J Obstet Gynecol Reprod Biol. 2016;198:138–44.
Siniscalchi RT, Melo M, Palma PC, Dal Fabbro IM, Vidal Bde C, Riccetto CL. Highly purified collagen coating enhances tissue adherence and integration properties of monofilament polypropylene meshes. Int Urogynecol J. 2013;24(10):1747–54.
Cornwell KG, Zhang F, Lineaweaver W. Bovine fetal collagen reinforcement in a small animal model of hernia with component repair. J Surg Res. 2016;201(2):416–24.
Avila OR, Parizzi NG, Souza AP, Botini DS, Alves JY, Almeida SH. Histological response to platelet-rich plasma added to polypropylene mesh implemented in rabbits. Int Braz J Urol. 2016;42(5):993–8.
Liang R, Knight K, Barone W, et al. Extracellular matrix regenerative graft attenuates the negative impact of polypropylene prolapse mesh on vagina in rhesus macaque. Am J Obstet Gynecol. 2017;216(2):153e1.
Ergina PL, Barkun JS, McCulloch P, Cook JA, Altman DG, IDEAL Group. IDEAL framework for surgical innovation 2: observational studies in the exploration and assessment stages. BMJ. 2013;346:f3011.
Acknowledgements
No funding or sponsorship was received for this study or publication of this article.
All authors read and approved the final manuscript. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. Holger Gerullis and Dimitri Barski contributed equally to this manuscript.
Disclosures
Holger Gerullis, Dimitri Barski, Evangelos Georgas, Mihaly Borós, Albert Ramon, Thorsten H. Ecke, Silvia Selinski, Dörte Luedders, Mario W. Kramer, Alexander Winter, Friedhelm Wawroschek, and Thomas Otto have nothing to disclose.
Compliance with Ethics Guidelines
This trial will be performed according to the Declaration of Helsinki. The protocol will be approved by the regional ethical commissions of the participating centers and possible additional centers. The study will only start once those institutions have given their positive vote. This article does not contain any new studies with human or animal subjects performed by any of the authors.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/ED87F060514E549F.
Rights and permissions
About this article
Cite this article
Gerullis, H., Barski, D., Georgas, E. et al. Protocol for a Randomized Phase II Trial for Mesh Optimization by Autologous Plasma Coating in Prolapse Repair: IDEAL Stage 3. Adv Ther 34, 995–1006 (2017). https://doi.org/10.1007/s12325-017-0493-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-017-0493-z