Abstract
Introduction
Pregabalin is an anticonvulsant approved in Europe for the treatment of neuropathic pain, as an adjunct therapy for epileptic seizures, and recently for generalized anxiety disorder. The aim of this study was to conduct a systematic review to evaluate the cost-effectiveness of pregabalin associated with the treatment of its labeled indications from a societal perspective in Spain.
Methods
Data from the MEDLINE database were searched using algorithms to identify relevant economic evaluations published in English or Spanish on pregabalin for the management of neuropathic pain, generalized anxiety disorder (GAD), and epilepsy in Spanish patients over the last 10 years.
Results
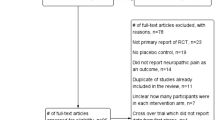
In total, 52 potentially relevant abstracts were identified from the MEDLINE database. Twenty manuscripts met the inclusion criteria. The majority of the selected papers (14/20) evaluated pregabalin for neuropathic pain from a societal perspective in Spain (5 economic models of pregabalin vs. gabapentin, 4 economic analyses of pregabalin in comparison with usual care, 4 economic evaluations comparing pregabalin monotherapy with add-on strategies, and one that evaluated different times of initiating pregabalin therapy). Five studies analyzed the use of pregabalin in Spain for the management of GAD (one cost-effectiveness model that compared pregabalin with venlafaxine, 2 secondary analyses in benzodiazepine-refractory patients, and 2 studies evaluating pregabalin vs. usual care in patients refractory to standard regimens). The last manuscript described a cost-effectiveness model that compared pregabalin versus levetiracetam use for the treatment of refractory partial epilepsy.
Conclusion
The majority of published evidence supports the possibility that pregabalin could be a cost-effective and/or cost-saving alternative for the treatment of refractory epilepsy, GAD, and neuropathic pain, in both treatment-naïve patients and in those who have demonstrated inadequate response or intolerance to previous therapy.


Similar content being viewed by others
References
McDermott AM, Toelle TR, Rowbotham DJ, et al. The burden of neuropathic pain: results from a cross-sectional survey. Eur J Pain. 2006;10(2):127–35.
Kavoussi R. Pregabalin: from molecule to medicine. Eur Neuropsychopharmacol. 2006;16(Suppl 2):S128–33.
Tassone DM, Boyce E, Guyer J, et al. Pregabalin: a novel gamma-aminobutyric acid analogue in the treatment of neuropathic pain, partial-onset seizures, and anxiety disorders. Clin Ther. 2007;29(1):26–48.
Torrance N, Smith BH, Bennett MI, et al. The epidemiology of chronic pain of predominantly neuropathic origin. Results from a general population survey. J Pain. 2006;7(4):281–9.
Portenoy RK. Painful polyneuropathy. Neurol Clin. 1989;7(2):265–88.
Bouhassira D, Lanteri-Minet M, Attal N, et al. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain. 2008;136(3):380–7.
Wittchen HU, Kessler RC, Beesdo K, et al. Generalized anxiety and depression in primary care: prevalence, recognition, and management. J Clin Psychiatry. 2002;63(Suppl 8):24–34.
Lieb R, Becker E, Altamura C. The epidemiology of generalized anxiety disorder in Europe. Eur Neuropsychopharmacol. 2005;15(4):445–52.
Kessler RC, Petukhova M, Sampson NA, et al. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21(3):169–84.
Chang BS, Lowenstein DH. Epilepsy. N Engl J Med. 2003;349(13):1257–66.
Fisher RS, van Emde Boas W, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46(4):470–2.
Hauser WA. Recent developments in the epidemiology of epilepsy. Acta Neurol Scand Suppl. 1995;162:17–21.
Rodriguez MJ, Garcia AJ, Investigators of Collaborative Study REC. A registry of the aetiology and costs of neuropathic pain in pain clinics: results of the registry of aetiologies and costs (REC) in neuropathic pain disorders study. Clin Drug Investig. 2007;27(11):771–82.
Rovira J, Albarracin G, Salvador L, et al. The cost of generalized anxiety disorder in primary care settings: results of the ANCORA study. Community Ment Health J. 2012;48(3):372–83.
Sancho J, Pena P, Rufo M, et al. Health and non-health care resources use in the management of adult outpatients with drug-resistant epilepsy in Spain: a cost-of-illness study (LINCE study). Epilepsy Res. 2008;81(2–3):176–87.
Beesdo-Baum K, Jenjahn E, Hofler M, et al. Avoidance, safety behavior, and reassurance seeking in generalized anxiety disorder. Depress Anxiety. 2012;29(11):948–57.
Lauria G, Faber CG, Merkies IS, et al. Diagnosis of neuropathic pain: challenges and possibilities. Expert Opin Med Diagn. 2012;6(2):89–93.
Prayson RA. Diagnostic challenges in the evaluation of chronic epilepsy-related surgical neuropathology. Am J Surg Pathol. 2010;34(5):e1–13.
Gallagher RM. Neuropathic pain: the global challenge. Pain Med. 2004;5(Suppl 1):S1–2.
Attal N, Cruccu G, Haanpaa M, et al. EFNS guidelines on pharmacological treatment of neuropathic pain. Eur J Neurol. 2006;13(11):1153–69.
Valverde Espinoza JA. Recommendations for pharmacological treatment of neuropathic pain. Neuroeje. 2012;25(2):51–61.
Rickels K, Pollack MH, Feltner DE, et al. Pregabalin for treatment of generalized anxiety disorder: a 4-week, multicenter, double-blind, placebo-controlled trial of pregabalin and alprazolam. Arch Gen Psychiatry. 2005;62(9):1022–30.
Bandelow B, Zohar J, Hollander E, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive–compulsive and posttraumatic stress disorders. World J Biol Psychiatry. 2002;3(4):171–99.
Cockerell OC, Johnson AL, Sander JW, et al. Prognosis of epilepsy: a review and further analysis of the first nine years of the British National General Practice Study of Epilepsy, a prospective population-based study. Epilepsia. 1997;38(1):31–46.
Elger CE, Brodie MJ, Anhut H, et al. Pregabalin add-on treatment in patients with partial seizures: a novel evaluation of flexible-dose and fixed-dose treatment in a double-blind, placebo-controlled study. Epilepsia. 2005;46(12):1926–36.
Shorvon SD, Lowenthal A, Janz D, et al. Multicenter double-blind, randomized, placebo-controlled trial of levetiracetam as add-on therapy in patients with refractory partial seizures. European Levetiracetam Study Group. Epilepsia. 2000;41(9):1179–86.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Sacristan JA, Oliva J, Del Llano J, et al. What is an efficient health technology in Spain? Gac Sanit. 2002;16(4):334–43.
Husereau D, Drummond M, Petrou S, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Pharmacoeconomics. 2013;31(5):361–7.
Finnerup NB, Sindrup SH, Jensen TS. The evidence for pharmacological treatment of neuropathic pain. Pain. 2010;150(3):573–81.
Rodriguez MJ, Diaz S, Vera-Llonch M, et al. Cost-effectiveness analysis of pregabalin versus gabapentin in the management of neuropathic pain due to diabetic polyneuropathy or post-herpetic neuralgia. Curr Med Res Opin. 2007;23(10):2585–96.
Perez C, Navarro A, Saldana MT, et al. Pregabalin and gabapentin in matched patients with peripheral neuropathic pain in routine medical practice in a primary care setting: findings from a cost–consequences analysis in a nested case–control study. Clin Ther. 2010;32(7):1357–70.
Navarro A, Saldana MT, Perez C, et al. Patient-reported outcomes in subjects with neuropathic pain receiving pregabalin: evidence from medical practice in primary care settings. Pain Med. 2010;11(5):719–31.
Saldana MT, Navarro A, Perez C, et al. Patient-reported outcomes in subjects with painful lumbar or cervical radiculopathy treated with pregabalin: evidence from medical practice in primary care settings. Rheumatol Int. 2010;30(8):1005–15.
Sicras-Mainar A, Rejas-Gutierrez J, Navarro-Artieda R, et al. Cost analysis of adding pregabalin or gabapentin to the management of community-treated patients with peripheral neuropathic pain. J Eval Clin Pract. 2011;18(6):1170–9.
Sicras-Mainar A, Rejas-Gutierrez J, Navarro-Artieda R, et al. Cost comparison of adding pregabalin or gabapentin for the first time to the therapy of patients with painful axial radiculopathy treated in Spain. Clin Exp Rheumatol. 2013;31(3):372–81.
Sicras A, Rejas J, Navarro R, et al. Adding pregabalin or gabapentin for the management of community-treated patients with painful diabetic peripheral neuropathy: a comparative cost analysis. Clin Drug Investig. 2013;33(11):825–35.
Morera-Dominguez C, Ceberio-Balda F, Florez-Garcia M, et al. Healthcare and non-healthcare resources utilization and related costs in subjects with refractory pain associated to neck pain: a post hoc analysis of the effect of pregabalin in a 12-week prospective study under routine medical practice conditions. Value Health. 2008(Suppl.):A637.
Florez-Garcia M, Ceberio-Balda F, Morera-Dominguez C, et al. Effect of pregabalin in the treatment of refractory neck pain: cost and clinical evidence from medical practice in orthopedic surgery and rehabilitation clinics. Pain Pract. 2011;11(4):369–80.
Morera-Dominguez C, Ceberio-Balda F, Florez-Garcia M, et al. A cost–consequence analysis of pregabalin versus usual care in the symptomatic treatment of refractory low back pain: sub-analysis of observational trial data from orthopaedic surgery and rehabilitation clinics. Clin Drug Investig. 2010;30(8):517–31.
de Salas-Cansado M, Perez C, Saldana MT, et al. A cost-effectiveness analysis of the effect of pregabalin versus usual care in the treatment of refractory neuropathic pain in routine medical practice in Spain. Pain Med. 2012;13(5):699–710.
de Salas-Cansado M, Perez C, Saldana MT, et al. An economic evaluation of pregabalin versus usual care in the management of community-treated patients with refractory painful diabetic peripheral neuropathy in primary care settings. Prim Care Diabetes. 2012;6(4):303–12.
Perez C, Saldana MT, Navarro A, et al. Trigeminal neuralgia treated with pregabalin in family medicine settings: its effect on pain alleviation and cost reduction. J Clin Pharmacol. 2009;49(5):582–90.
Saldana MT, Navarro A, Perez C, et al. A cost–consequences analysis of the effect of pregabalin in the treatment of painful radiculopathy under medical practice conditions in primary care settings. Pain Pract. 2010;10(1):31–41.
Navarro A, Saldana MT, Perez C, et al. A cost–consequences analysis of the effect of pregabalin in the treatment of peripheral neuropathic pain in routine medical practice in primary care settings. BMC Neurol. 2011;11:7.
Navarro A, Saldana MT, Perez C, et al. Costs and health resources utilization following switching to pregabalin in individuals with gabapentin-refractory neuropathic pain: a post hoc analysis. Pain Pract. 2012;12(5):382–93.
Perez C, Navarro A, Saldana MT, et al. Cost savings associated with early initiation of pregabalin in the management of peripheral neuropathic pain. Clin J Pain. 2013;29(6):471–7.
Vera-Llonch M, Dukes E, Rejas J, et al. Cost-effectiveness of pregabalin versus venlafaxine in the treatment of generalized anxiety disorder: findings from a Spanish perspective. Eur J Health Econ. 2010;11(1):35–44.
de Salas-Cansado M, Olivares JM, Alvarez E, et al. Pregabalin versus SSRIs and SNRIs in benzodiazepine-refractory outpatients with generalized anxiety disorder: a post hoc cost-effectiveness analysis in usual medical practice in Spain. Clinicoecon Outcomes Res. 2012;4:157–68.
Carrasco Perera JL, Alvarez E, Olivares JM, et al. Análisis comparativo de costes del inicio de terapia con pregabalina o ISRS/ISRN en pacientes resistentes a las benzodiazepinas con trastorno de ansiedad generalizada en España. Actas españolas de psiquiatría. 2013;41(3):164–74.
de Salas-Cansado M, Alvarez E, Olivares JM, et al. Modelling the cost-effectiveness of pregabalin versus usual care in daily practice in the treatment of refractory generalised anxiety disorder in Spain. Soc Psychiatry Psychiatr Epidemiol. 2013;48(6):985–96.
Carrasco JL, Olivares JM, Álvarez E, et al. Adjunctive therapy with pregabalin in generalized anxiety disorder patients with partial response to SSRI treatment: a cost–consequences analysis in medical practice in Spain. ISPOR 16th Annual European Congress; Dublin, Ireland. Value Health. 2013;16:A547.
Organization WH. Disability Assessment Schedule II (WHO-DAS II). Geneva: WHO; 2000.
Diaz S, Argumosa A, Horga de la Parte JF, et al. Analysis of the cost-effectiveness of treatment for refractory partial epilepsy: a simulation model for pregabalin and levetiracetam. Rev Neurol. 2007;45(8):460–7.
Zhao Y, Sun P, Watson P. Medication adherence and healthcare costs among patients with diabetic peripheral neuropathic pain initiating duloxetine versus pregabalin. Curr Med Res Opin. 2011;27(4):785–92.
Prettyjohns M, Sandelin R, Lister S, et al. A cost–utility study of the use of pregabalin added to usual care in refractory neuropathic pain patients in a Swedish setting. J Med Econ. 2012;15(6):1097–109.
Vera-Llonch M, Brandenburg NA, Oster G. Cost-effectiveness of add-on therapy with pregabalin in patients with refractory partial epilepsy. Epilepsia. 2008;49(3):431–7.
Lopez-Bastida J, Oliva J, Antonanzas F, et al. Spanish recommendations on economic evaluation of health technologies. Eur J Health Econ. 2010;11(5):513–20.
Acknowledgments
An unrestricted grant was provided by Pfizer, S.L.U., Madrid, Spain, for the literature search, preparation of the tables, and for writing assistance. The authors wish to thank Emili González-Pérez (TFS Develop, Barcelona, Spain) for his assistance in writing this manuscript. Sponsorship and article processing charges for this study were funded by Pfizer, S.L.U. Dr. Darbà is the guarantor for this article and takes responsibility for the integrity of the work as a whole.
Conflict of interest
J Darbà, L. Kaskens, C. Pérez, E. Álvarez, R. Navarro-Artieda, and A. Sicras-Mainar declare that they have no conflict of interests as a consequence of this manuscript nor have they received any payment related with their authorship.
Compliance with ethics guidelines
This systematic review is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Darbà, J., Kaskens, L., Pérez, C. et al. Pharmacoeconomic Outcomes for Pregabalin: A Systematic Review in Neuropathic Pain, Generalized Anxiety Disorder, and Epilepsy from a Spanish Perspective. Adv Ther 31, 1–29 (2014). https://doi.org/10.1007/s12325-013-0088-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-013-0088-2