Abstract
Introduction
To evaluate the efficacy and safety of onabotulinumtoxinA for the treatment of neurogenic detrusor overactivity (NDO) in subpopulations of etiology (multiple sclerosis [MS] or spinal cord injury [SCI]) and concomitant anticholinergics (use/non-use).
Methods
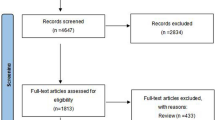
Data were pooled from two double-blind, placebo-controlled, pivotal, phase 3 studies including a total of 691 patients with ≥14 urinary incontinence (UI) episodes/week due to MS (n = 381) or SCI (n = 310). Patients received intradetrusor injections of onabotulinumtoxinA 200U (n = 227), 300U (n = 223), or placebo (n = 241). Change from baseline at week 6 in UI episodes/week (primary endpoint), urodynamics, quality of life (QOL), and adverse events (AEs) were assessed.
Results
Significant and similar reductions in UI episodes were observed regardless of etiology or anticholinergic use: at week 6, mean weekly decreases of −22.6 and −19.6 were seen in MS and SCI patients, respectively, and −20.3 and −22.5 in anticholinergic users and non-users, respectively, treated with onabotulinumtoxinA 200U. The 300U dose did not add to the clinical efficacy in any subpopulation. Similar proportions of patients achieved ≥50% or 100% reductions in UI episodes in all subgroups. Improvements in maximum cystometric capacity, maximum detrusor pressure during first involuntary detrusor contraction, and QOL were significant in both etiologies and were independent of anticholinergic use. The most common AEs in all groups were urinary tract infection and urinary retention.
Conclusion
Regardless of concomitant anticholinergic use or etiology, onabotulinumtoxinA significantly improved UI symptoms, urodynamics, and QOL in patients with UI due to NDO. OnabotulinumtoxinA was well tolerated in all groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with neurologic conditions such as multiple sclerosis (MS) or spinal cord injury (SCI) often have neurogenic detrusor overactivity (NDO), which frequently results in urinary incontinence (UI) and high detrusor pressures [1, 2]. OnabotulinumtoxinA (BOTOX®, Allergan, Inc., Irvine, CA, USA) has been shown to be effective in the treatment of UI due to neurogenic detrusor overactivity in MS and SCI patients in phase 2 trials [3–5] and in two double-blind, placebo-controlled, phase 3 registration trials [6, 7]. The phase 3 trials demonstrated significant reductions in UI as well as improvements in urodynamic parameters and quality of life (QOL) with onabotulinumtoxinA in patients who had been inadequately managed with anticholinergic medications. Where approved, the 200U dose of onabotulinumtoxinA is the registered dose for the treatment of patients with UI due to NDO. Units of biological activity of onabotulinumtoxinA cannot be compared with or converted into units of any other botulinum toxin product, and onabotulinumtoxinA is not interchangeable with other botulinum toxin preparations.
In this analysis, we further evaluated the efficacy and safety of onabotulinumtoxinA in the patients with the two neurologic etiologies (MS and SCI) separately. In addition, there were differences in regard to the use of anticholinergics. The study protocols required all patients to have been inadequately managed with at least one anticholinergic for their UI. Some patients chose to continue using concomitant anticholinergics during the phase 3 studies, while others discontinued their anticholinergics prior to study start and remained off them throughout the study. The trial population thus consisted of two distinct subpopulations of patients: those taking onabotulinumtoxinA plus a concomitant anticholinergic medication, and those who received onabotulinumtoxinA alone. Therefore, we also examined the impact of concomitant anticholinergic use/non-use on the efficacy and safety of onabotulinumtoxinA. Pooling the data from these trials provided a larger sample size to examine the effect of onabotulinumtoxinA 200U and 300U in these two specific subpopulations.
Materials and Methods
Study Design
Details regarding study design and patient selection for these studies have been described previously [6, 7]. Briefly, the pivotal phase 3 trials (DIGNITY studies; ClinicalTrials.gov NCT00311376 and NCT00461292) were international, multicenter, randomized, double-blind, placebo-controlled trials conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000, and all study participants provided written informed consent. The studies included patients with ≥14 UI episodes per week due to NDO from SCI or MS. Study protocols required all patients to have been inadequately managed with at least one anticholinergic for their UI, defined as an inadequate response or intolerable side effects after >1 month on an optimized dose. The protocol design allowed patients to remain on anticholinergic medication to provide more protection to the upper urinary tract for those randomized to the placebo group in treatment cycle 1. Those taking anticholinergics had to maintain them at the baseline dose throughout the study, and those not taking anticholinergics were to remain off them. Patients were either using clean intermittent catheterization (CIC) prior to study entry or had to be willing to initiate CIC if necessary.
Patients were randomized 1:1:1 to receive 30 1-mL intradetrusor injections of placebo, onabotulinumtoxinA 200U, or 300U, administered cystoscopically, avoiding the trigone. Patients were followed for 52 weeks and evaluated post treatment at weeks 2, 6, and 12, and every 6 weeks thereafter. A second treatment could be requested from 12 weeks after treatment 1 onward.
Efficacy and Safety Assessments
Change from baseline in weekly UI episodes, as well as the proportion of patients achieving ≥50% or 100% (complete dryness) reduction from baseline in UI episodes, was evaluated in all subgroups. Changes from baseline in maximum cystometric capacity (MCC), maximum detrusor pressure during first involuntary detrusor contraction (P detmaxIDC), and percentage of patients with no involuntary detrusor contraction (IDC) were assessed. Health-related QOL was evaluated using the change from baseline in the Incontinence Quality of Life (I-QOL) questionnaire total summary score [8]. Other assessments included the time to patient request for retreatment (measuring duration of effect) and a general satisfaction with treatment question (5-point rating scale from very satisfied to very dissatisfied).
Adverse events (AEs) were recorded throughout the study. No distinction was made between asymptomatic and symptomatic urinary tract infections (UTIs) in these studies. The recording of urinary retention as an AE was based on the investigator’s clinical judgment.
Statistical Analysis
Analysis of covariance was used to assess efficacy in the intent-to-treat (ITT; all randomized patients) population, with baseline value as a covariate, and treatment arm and investigative site as factors. The placebo-controlled comparison focused on the first 12 weeks after treatment 1, before patients were eligible for retreatment. In MS patients who were not using CIC at baseline, patient satisfaction with treatment at week 6 was compared between those who initiated CIC and those who remained off CIC post treatment using the Cochran–Mantel–Haenszel test, controlling for treatment group. Patients who responded with “very satisfied” or “somewhat satisfied” to the general satisfaction with treatment question were categorized as “satisfied” in the analysis, whereas patients who responded with “neutral,” “somewhat dissatisfied,” or “very dissatisfied” were categorized as “dissatisfied.” Median time to patient request for retreatment was evaluated using Kaplan–Meier analysis, and 95% confidence intervals (CI) were calculated.
The safety population consisted of all randomized patients treated on day 1 and who received study drug (analyzed according to dose actually received).
Results
Efficacy and Safety by Etiology
The pooled ITT population from both studies combined (N = 691) included 381 patients with MS and 310 with SCI. Most baseline characteristics were comparable between the groups (Table 1). Differences included gender (the majority of SCI patients were male; the majority of MS patients were female), baseline CIC use (SCI 84.8%, MS 29.4%), baseline anticholinergic use (SCI 60.0%, MS 50.7%), and baseline values for P detmaxIDC (SCI 58.1 ± 40.4, MS 39.7 ± 29.8; Table 2).
Both MS and SCI patients exhibited consistently significant decreases from baseline in UI episodes following onabotulinumtoxinA treatment compared with placebo at week 6, with mean weekly decreases of −14.0, −22.6, and −24.0 in MS patients (P < 0.05) and −6.4, −19.6, and −18.2 in SCI patients (P < 0.001) in the placebo, onabotulinumtoxinA 200U, and 300U groups, respectively (Fig. 1a). A significantly higher proportion of MS and SCI patients (P < 0.001 for both) treated with onabotulinumtoxinA achieved ≥50% or 100% reduction (i.e., dry) in weekly UI episodes at week 6 compared with the placebo group (Fig. 1b). At week 6, dry rates were 10.7%, 41.5%, and 44.2% in MS patients and 7.3%, 30.9%, and 35.9% in SCI patients in the placebo, onabotulinumtoxinA 200U, and 300U groups, respectively. No clinically relevant difference in reduction of UI episodes was observed between the dose groups in either etiology.
The change in the number of voluntary voids per week was examined in the non-catheterizing MS subpopulation. In contrast to SCI patients (13.5% voiding voluntarily at baseline), the majority of MS patients were not using CIC at baseline and were voiding spontaneously (69.6%). At week 6 following onabotulinumtoxinA treatment, the number of voluntary voids per week significantly decreased in MS patients who were not catheterizing at baseline compared with placebo (P ≤ 0.05 for both doses; Fig. 2). The number of voluntary voids per week was not assessed in the SCI subpopulation because there were too few SCI patients who were not catheterizing at baseline to allow for a meaningful analysis.
Both MS and SCI patients treated with onabotulinumtoxinA showed significantly greater increases in MCC from baseline at week 6 compared with placebo (P < 0.001 for all; Table 2). The magnitude of increase was similar between the etiologies and between the onabotulinumtoxinA dose groups. A large proportion of onabotulinumtoxinA-treated patients in both etiologies had no IDC (up to a filled volume of 500 mL) at week 6 relative to placebo (18.5%, 68.0%, and 70.9% [P < 0.001] in MS patients and 18.2%, 58.7%, and 57.6% [P < 0.001] in SCI patients in the placebo, onabotulinumtoxinA 200U, and 300U groups, respectively; Table 2). In patients who had an IDC, decreases from baseline in P detmaxIDC were significantly greater compared with placebo at week 6 (P < 0.001 for MS patients, P < 0.05 for SCI patients). SCI patients showed decreases of −42.7 and −35.3 in the respective onabotulinumtoxinA 200U and 300U groups, compared with decreases of −22.1 and −24.1 in MS patients (Table 2).
Both MS and SCI patients demonstrated significant improvements compared with placebo in I-QOL total summary score. The magnitude of change from baseline for both etiologies and both onabotulinumtoxinA doses was considerably greater than 11 points, which is the established minimally important difference (MID) [8] (Fig. 3).
Mean change from baseline at week 6 in the I-QOL total score by etiology. Dashed line indicates the MID of an 11-point increase from baseline [8]. *P < 0.001 vs placebo. I-QOL Incontinence Quality of Life, MID minimally important difference, MS multiple sclerosis, OnabotA onabotulinumtoxinA, SCI spinal cord injury
In the MS population, the median time to patient request for retreatment was 295 and 307 days in the onabotulinumtoxinA 200U and 300U groups, respectively, whereas the SCI population requested retreatment earlier at 253 and 211 days in the onabotulinumtoxinA 200U and 300U groups, respectively. The median time to patient request for retreatment in the placebo group was 92 days for both etiologies, which is close to the minimum permissible time of 12 weeks after initial treatment (P < 0.001 for both doses vs placebo).
Adverse events across treatment cycle 1 for the MS and SCI populations are presented in Table 3. UTI was the most common AE in both etiologies. The incidence of UTIs was similar among all treatment groups for SCI patients (P = 0.534), but was higher in the onabotulinumtoxinA-treated MS patients compared with placebo (P < 0.001). Very few complicated UTIs were reported: pyelonephritis was reported in one MS patient (onabotulinumtoxinA 300U group) and in two SCI patients (both in the placebo group), and urosepsis was reported in two SCI patients (both in the placebo group).
The AE of urinary retention was further examined only in MS patients as most SCI patients were already performing CIC at study entry. Urinary retention appeared to show a dose-dependent increase in those MS patients who were not catheterizing at baseline. The rate of de novo CIC due to urinary retention during treatment cycle 1 was 31.4% (27/86) and 47.1% (41/87) in the onabotulinumtoxinA 200U and 300U groups, respectively, compared with 4.5% (4/88) in the placebo group. The duration of de novo CIC for urinary retention in MS patients treated with onabotulinumtoxinA 200U (the approved dose where licensed) is illustrated in Fig. 4: 15.1% of patients used de novo CIC for ≤36 weeks, while 16.3% used CIC for >36 weeks. Importantly, 68.6% of the MS patients who received onabotulinumtoxinA 200U did not initiate CIC during treatment cycle 1.
The proportion of MS patients who initiated CIC for any reason in treatment cycle 1 was 17%, 40%, and 51% in the placebo, onabotulinumtoxinA 200U, and 300U groups, respectively. In these patients, the mean weekly frequency of CIC was not significantly different among groups; 13.4, 18.1, and 21.1 (P = 0.417) at week 6 after treatment and 9.4, 16.8, and 17.2 (P = 0.365) at week 12 in the placebo, onabotulinumtoxinA 200U, and 300U groups, respectively. The impact of initiation of CIC on patient satisfaction with treatment was assessed in MS patients (Fig. 5). Satisfaction (defined as “very satisfied” or “somewhat satisfied”) with onabotulinumtoxinA treatment remained high regardless of CIC initiation, with no statistically significant difference in satisfaction between the groups initiating CIC and those who did not for the 200U dose group (P = 0.167); however, a significant difference was observed for the 300U dose group (P = 0.048).
Efficacy and Safety by Baseline Anticholinergic Use
At the time of study entry, the majority of the patients had previously tried one (59.2%) or two (21.0%) different anticholinergics (Table 4). Most patients (76.1%) were inadequately managed with anticholinergics due to inadequate efficacy. In the pooled ITT population, 379/691 (55%) of patients were taking anticholinergics at baseline.
Significant reductions in weekly UI episodes were observed with onabotulinumtoxinA 200U and 300U within the anticholinergic user and non-user subgroups (P ≤ 0.05 vs placebo for both subgroups; Fig. 6a). Comparison in UI at week 6 between the two subgroups did not yield statistically significant (P = 0.454) or clinically relevant differences. Likewise, similar proportions of patients within the anticholinergic user and non-user subgroups achieved ≥50% or 100% reductions in weekly UI episodes at week 6 (Fig. 6b). Dry rates for placebo, onabotulinumtoxinA 200U, and 300U were 7.9%, 36.7%, and 39.5% in the anticholinergic user and 10.9%, 37.4%, and 41.3% in the non-user subgroups, respectively (P < 0.001 vs placebo each for users and non-users).
UI by anticholinergic use in the pooled ITT population. a Mean change from baseline in weekly UI episodes. b Responder rates for ≥50% and 100% reductions in UI episodes at week 6. *P < 0.001; † P < 0.05; ‡ P < 0.005 vs placebo. AC anticholinergic, ITT intent-to-treat, OnabotA onabotulinumtoxinA, UI urinary incontinence
Significant and similar increases in MCC in the onabotulinumtoxinA groups compared with placebo were seen in both anticholinergic users and non-users (Table 2). Decreases in P detmaxIDC and increases in I-QOL total summary scores were also similar regardless of anticholinergic use. Mean increases from baseline in I-QOL total summary scores at week 6 were 11.4, 28.7, and 31.9 for users (P = 0.001 vs placebo) and 10.8, 22.7, and 26.3 for non-users of anticholinergics (P ≤ 0.002 vs placebo) in the placebo, onabotulinumtoxinA 200U, and 300U groups, respectively. The median times to patient request for retreatment were 99 (95% CI, 92–127), 269 (95% CI, 211–310), and 296 (95% CI, 253–420) days in anticholinergic users compared with 88 (95% CI, 88–103), 266 (95% CI, 221–337), and 253 (95% CI, 209–295) days in non-users in the placebo, onabotulinumtoxinA 200U, and 300U groups, respectively.
The evaluation of AEs by anticholinergic use showed that for the respective placebo, onabotulinumtoxinA 200U, and 300U groups, incidences of UTI were 43.1%, 58.7%, and 57.4% in users and 26.5%, 43.8%, and 54.5% in non-users, and respective incidences of urinary retention were 2.9%, 14.9%, and 21.7% in users and 4.1%, 25.7%, and 24.8% in non-users.
Discussion
These pooled data from two phase 3 trials include the largest cohorts of MS and SCI patients with UI due to NDO studied to date. Treatment with onabotulinumtoxinA resulted in significant improvements in UI, urodynamic parameters, and QOL in these patients regardless of etiology. Consistent with previous analyses [6, 7], there was no advantage in terms of efficacy for the 300U dose of onabotulinumtoxinA compared with the 200U dose in either the SCI or MS subpopulations. The only notable differences in efficacy between etiologies were that a larger placebo response was seen in change from baseline in UI episodes in the MS population, and a greater magnitude of reduction in P detmaxIDC was observed in the SCI population.
This larger placebo response in the MS population may reflect that the majority of MS patients were spontaneously voiding at baseline, and the observed placebo response is consistent with that of a non-neurogenic population [9]. In addition, just under 20% of the MS patients receiving placebo initiated CIC during the study. Many of these patients would likely have benefited from CIC prior to study entry, and the improved bladder emptying with CIC alone may have contributed to the improvements seen in MS patients receiving placebo. Nevertheless, the treatment effect between onabotulinumtoxinA and placebo in MS and SCI patients was similar. The greater reduction in P detmaxIDC observed in the SCI group is likely a reflection of the higher baseline values in the SCI population.
Patients of both etiologies exhibited improvements in I-QOL total scores that were considerably greater than the established MID of 11 points [8], with the magnitude of change being greatest in the MS population. This implies that these neurogenic populations have an improved health-related QOL when treated with onabotulinumtoxinA.
OnabotulinumtoxinA was well tolerated in both the MS and SCI populations, with the voiding pattern prior to treatment being the key difference between the two etiologies. The majority of MS patients were not using CIC prior to treatment, whereas the majority of SCI patients were. Therefore, the occurrence of urinary retention, initiation of CIC, and UTI rates were higher post treatment in the MS population. Nevertheless, in those MS patients not using CIC at baseline, the majority continued to avoid the need to use CIC for urinary retention post treatment (59/86 [68.6%]) or catheterized for urinary retention for a duration of ≤18 weeks (10/86 [11.6%]). In those who initiated CIC, the mean frequency was about 2.5 times/day, indicating that many maintained some ability to spontaneously void. MS patients’ satisfaction with treatment appeared to be independent of initiation of CIC, in line with previous findings that patient QOL is not affected by initiation of CIC after treatment with onabotulinumtoxinA [10, 11]. Furthermore, the higher incidence of UTI did not result in higher rates of complicated UTI.
In addition to examining the data by etiology, pooling the data provided a large sample size to examine onabotulinumtoxinA treatment with and without concomitant anticholinergic use. Though widely used as first-line treatment for NDO, anticholinergics are not always effective or may have intolerable side effects, and many patients discontinue their use [12, 13]. This study found that improvements in UI, urodynamics, QOL, and duration of effect were independent of anticholinergic use. One possible explanation for the lack of an additional effect of anticholinergics in the presence of onabotulinumtoxinA may be that onabotulinumtoxinA, by directly blocking the release of acetylcholine into the neuromuscular junction [14], may provide a more efficacious method for preventing muscarinic receptor activation than antimuscarinic drugs, which act by competitive blockade of the receptors [12].
A systematic review that examined studies in which patients were treated concomitantly with onabotulinumtoxinA and anticholinergics found that 28–58% of patients treated with onabotulinumtoxinA discontinued anticholinergics and most reduced their dose [15]. However, the pooled studies presented here were not designed to examine the effects of dose decreases or discontinuation of anticholinergics with onabotulinumtoxinA treatment. Rather, the protocols of these pivotal efficacy/safety trials required that anticholinergic doses remained constant during the study so as not to confound the results, and the trials in our analysis only included NDO patients who were inadequately managed by anticholinergics.
Conclusion
OnabotulinumtoxinA significantly improved UI episodes per week, urodynamic parameters, and QOL in both SCI and MS patients with UI due to NDO and regardless of concurrent anticholinergic use. OnabotulinumtoxinA was well tolerated in all subgroups.
References
Foley SJ, McFarlane JP, Shah PJ. Vesico-ureteric reflux in adult patients with spinal injury. Br J Urol. 1997;79:888–91.
Hicken BL, Putzke JD, Richards JS. Bladder management and quality of life after spinal cord injury. Am J Phys Med Rehabil. 2001;80:916–22.
Schurch B, de Seze M, Denys P, et al. Botulinum toxin type a is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol. 2005;174:196–200.
Schurch B, Denys P, Kozma CM, et al. Botulinum toxin A improves the quality of life of patients with neurogenic urinary incontinence. Eur Urol. 2007;52:850–8.
Apostolidis A, Thompson C, Yan X, Mourad S. An exploratory, placebo-controlled, dose-response study of the efficacy and safety of onabotulinumtoxinA in spinal cord injury patients with urinary incontinence due to neurogenic detrusor overactivity. World J Urol. 2012 (Epub ahead of print).
Cruz F, Herschorn S, Aliotta P, et al. Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial. Eur Urol. 2011;60:742–50.
Ginsberg D, Gousse A, Keppenne V, et al. Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity. J Urol. 2012;187:2131–9.
Schurch B, Denys P, Kozma CM, et al. Reliability and validity of the Incontinence Quality of Life questionnaire in patients with neurogenic urinary incontinence. Arch Phys Med Rehabil. 2007;88:646–52.
Dmochowski R, Chapple C, Nitti VW, et al. Efficacy and safety of onabotulinumtoxinA for idiopathic overactive bladder: a double-blind, placebo controlled, randomized, dose ranging trial. J Urol. 2010;184:2416–22.
Khan S, Game X, Kalsi V, et al. Long-term effect on quality of life of repeat detrusor injections of botulinum neurotoxin-A for detrusor overactivity in patients with multiple sclerosis. J Urol. 2011;185:1344–9.
Kessler TM, Khan S, Panicker J, et al. Clean intermittent self-catheterization after botulinum neurotoxin type A injections: short-term effect on quality of life. Obstet Gynecol. 2009;113:1046–51.
Finney SM, Andersson KE, Gillespie JI, Stewart LH. Antimuscarinic drugs in detrusor overactivity and the overactive bladder syndrome: motor or sensory actions? BJU Int. 2006;98:503–7.
Szollar SM, Lee SM. Intravesical oxybutynin for spinal cord injury patients. Spinal Cord. 1996;34:284–7.
Apostolidis A, Dasgupta P, Fowler CJ. Proposed mechanism for the efficacy of injected botulinum toxin in the treatment of human detrusor overactivity. Eur Urol. 2006;49:644–50.
Karsenty G, Denys P, Amarenco G, et al. Botulinum toxin A (Botox) intradetrusor injections in adults with neurogenic detrusor overactivity/neurogenic overactive bladder: a systematic literature review. Eur Urol. 2008;53:275–87.
Acknowledgments
Participating investigators in the individual studies have been listed previously [6, 7]. Assistance with the writing and development of the manuscript was provided by Jennifer L. Giel, Ph.D., of Evidence Scientific Solutions, Philadelphia, PA, USA, and was funded by Allergan, Inc. Dr. Ginsberg is the guarantor for this article, and takes responsibility for the integrity of the work as a whole. Sponsorship and article processing charges for this study were funded by Allergan, Inc.
Conflict of interest
Dr. Ginsberg has received funding or reimbursements from Allergan, Medtronic, and Pfizer. Dr. Cruz is a consultant for Allergan, Astellas, and Recordati and is on the speaker bureau for Allergan, Astellas, Recordati, AMS, Kyorin, and Pfizer. Dr. Herschorn has conducted clinical trials for Allergan, Astellas, Pfizer, American Medical Systems, Contura, Johnson & Johnson, Cook Medical, and Laborie; has served as a consultant for Allergan, Astellas, Pfizer, and American Medical Systems; and is on advisory boards for Allergan, Astellas, and Pfizer. Dr. Gousse declares no conflict of interest. Dr. Keppenne has served as a consultant for Allergan, Astellas, Pfizer, Therabel, Coloplast, and Astratech. Dr. Aliotta is on the speaker bureau for Watson, Astellas, and Eli Lilly. Dr. Sievert is a consultant for Allergan, Astellas, AMS, Medtronic, Neotract, and Janssen; participates in trials for Allergan, Medtronic, and Neotract; receives speaker honoraria from Astellas, AMS, Medtronic, Karl Storz, and Neotract; has received travel grants from Astellas and AMS; and has received research grants or fellowships from AMS, Medtronic, and Karl Storz. Dr. Heesakkers has received research grants from Pfizer, Astellas, Pohl Boskamp, and Uroplasty and has served as a consultant for Pfizer, Astellas, Allergan, Ipsen, Johnson & Johnson, and Uroplasty. Dr. Brin is an employee of Allergan, Inc. Ms. Jenkins is an employee of Allergan, Inc. Dr. Thompson is an employee of Allergan, Inc. Dr. Lam is an employee of Allergan, Inc. Dr. Haag-Molkenteller is an employee of Allergan, Inc.
Compliance with ethics guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Prior presentation
These data have never been previously presented in total, but partial subsets of the data from this manuscript have been presented at the 2011 meetings of the American Spinal Injury Association, North American Spine Society, and Société Internationale d’Urologie; the 2012 meetings of the European Association of Urology, European Committee for Treatment and Research in Multiple Sclerosis, and Dutch Multiple Sclerosis Research Days; and the 2013 meeting of the Society for Urodynamics and Female Urology.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
ClinicalTrials.gov identifiers: NCT00311376 and NCT00461292.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ginsberg, D., Cruz, F., Herschorn, S. et al. OnabotulinumtoxinA is Effective in Patients with Urinary Incontinence due to Neurogenic Detrusor Activity Regardless of Concomitant Anticholinergic Use or Neurologic Etiology. Adv Ther 30, 819–833 (2013). https://doi.org/10.1007/s12325-013-0054-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-013-0054-z