Abstract
Substantial evidence highlights the role of the cerebellum in the pathophysiology of tremor in essential tremor (ET), although its potential involvement in altered movement execution in this condition remains unclear. This study aims to explore potential correlations between the cerebellum and basal ganglia functional connectivity and voluntary movement execution abnormalities in ET, objectively assessed with kinematic techniques. A total of 20 patients diagnosed with ET and 18 healthy subjects were enrolled in this study. Tremor and repetitive finger tapping were recorded using an optoelectronic kinematic system. All participants underwent comprehensive 3T-MRI examinations, including 3D-T1 and blood-oxygen-level dependent (BOLD) sequences during resting state. Morphometric analysis was conducted on the 3D-T1 images, while a seed-based analysis was performed to investigate the resting-state functional connectivity (rsFC) of dorsal and ventral portions of the dentate nucleus and the external and internal segments of the globus pallidus. Finally, potential correlations between rsFC alterations in patients and clinical as well as kinematic scores were assessed. Finger tapping movements were slower in ET than in healthy subjects. Compared to healthy subjects, patients with ET exhibited altered FC of both dentate and globus pallidus with cerebellar, basal ganglia, and cortical areas. Interestingly, both dentate and pallidal FC exhibited positive correlations with movement velocity in patients, differently from that we observed in healthy subjects, indicating the higher the FC, the faster the finger tapping. The findings of this study indicate the possible role of both cerebellum and basal ganglia in the pathophysiology of altered voluntary movement execution in patients with ET.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Essential tremor (ET) is a neurological condition clinically characterized by bilateral action tremor of the upper limb lasting for at least 3 years [1]. Previous neurophysiological studies have demonstrated an altered voluntary movement execution, manifested as movement slowness (bradykinesia) in a significant proportion of ET patients [2,3,4,5,6,7].
It is widely acknowledged that dysfunction within the cerebello-thalamo-cortical circuit plays a significant role in the pathophysiology of ET [8,9,10,11,12]. Resting-state functional magnetic resonance imaging (rs-fMRI) studies have consistently demonstrated impaired functional connectivity (FC) between the cerebellum and both cortical and subcortical regions in ET patients [13,14,15,16,17]. The dentate nucleus (DN), which is the primary cerebellar output, projects to the thalamus and cortical areas. DN is composed by dorsal (motor) and ventral (associative) domains [18]. The dorsal domain receives projection from the lateral cerebellum and is connected via ventro-lateral nuclei of thalamus with motor cortical areas (motor cortex, premotor cortex, supplementary motor area, somatosensory cortex) whereas the ventral domain is connected via dorsomedial thalamus nuclei with associative cortices (prefrontal cortex, intraparietal and inferior parietal cortex) [19,20,21]. Both domains are connected with striatum via intralaminar nuclei of thalamus [22]. Alterations in DN-FC, both within and outside the cerebellum, is present in ET [9]. Tikoo et al., found a correlation between DN functional disconnection and the severity of tremor as well as cognitive impairment in ET patients [17]. Given the key role of the cerebellum in ET pathophysiology, it is plausible that DN dysfunction may also play a role in the pathophysiology of altered voluntary movement execution in ET patients [2, 23, 24]. This hypothesis is supported by the observation that various kinematic parameters, particularly movement direction and velocity, are encoded in cerebellar neural activity. In particular, the spike firing of Purkinje cells, the main output of the cerebellar cortex, is thought to control movement velocity across multiple tasks [2]. Furthermore, several studies have shown that degenerative cerebellar disease, cerebellar tumors and ischemic lesions may be associated with slowed movement execution (bradykinesia) [7, 25]. Additional mechanisms, however, may involve a wider cerebral network, including not only the cerebellum and interconnected cortical motor areas but also the basal ganglia (BG). In this regard, the globus pallidus (GP) serves as the central output hub within the BG circuitry, essential for efficient and fast voluntary movement execution [26, 27]. GP is distinct in two parts, the internal (GPi) is deputed of motor output of BG; and the external (GPe) is a regulatory relay in BG circuit, classically acknowledged in the indirect pathway [28]. GP has been implicated in fine regulation of movement velocity and amplitude, regulating frequency and synchronicity of oscillation in motor network [29,30,31]. ET patients demonstrated reduced structural connectivity within the GP, caudate, and supplementary motor area (SMA) [32]. Hence, together with the cerebellum, the BG may also contribute to the pathophysiology of altered voluntary movement execution in ET, as recently proposed [33].
To the best of our knowledge, there is no research study investigating the relationship between quantitative kinematic measurements of voluntary movement execution, and the activity of brain networks in individuals with ET. Moreover, no previous studies have thoroughly examined possible changes in connectivity within (or between) the cerebellum and BG, focusing on GP network activity as main voluntary movement BG output, and their potential implications in ET pathophysiology. Therefore, the primary objective of this study is to investigate the morphometric and functional changes of the cerebellum and BG in ET patients and to explore the correlations between these changes and kinematic measures of altered movement execution observed during repetitive finger tapping tasks, which are widely employed in clinical practice to evaluate bradykinesia [2, 34]. By conducting this study, we aim to gain deeper insights into the role of the cerebellum and BG in the pathophysiology of movement execution alterations in ET.
Methods
Participants and Clinical Assessment
This study included 20 ET patients (3 females) with a mean age of 67.7 ± 13.4 years and a disease duration of 13.9 ± 9.9 years. ET patients were consecutively enrolled from the Movement Disorder Outpatient Clinic at the Department of Human Neurosciences, Sapienza University of Rome, Italy. The control group consisted of 18 healthy subjects (HS) (6 females) with a mean age of 62.8 ± 7.8 years. The clinical diagnosis of ET was based on the established clinical diagnostic criteria [1]. ET patients with clinically detectable soft-signs (ET-plus patients with rest tremor, questionable dystonia and ataxia) and psychiatric conditions were excluded from the study. Clinical evaluations of the patients were conducted by a neurologist with expertise in movement disorders (MB). To minimize any potential confounding effects of medication, all patients discontinued their medications 48 hours prior to the experiment. Five out of 20 subjects exhibited head tremor, yet this did not lead to significant artifacts, as also demonstrated by ICA-AROMA analysis. Clinical assessment of ET patients was performed using the Fahn-Tolosa-Marin Tremor Rating Scale (FTMTRS) [35] and the Movement Disorder Society -sponsored revision of the Unified Parkinson’s Disease Rating Scale, motor section (MDS-UPDRS-III) [36]. All participants also underwent the Montreal Cognitive Assessment (MoCA) [37] and the Beck Depression Inventory (BDI-II) [38] to define the cognitive profile and depressive symptoms. Study participants underwent the kinematic evaluation and MRI session on two separate days, within one week. All enrolled subjects provided written informed consent for the use of their data for research purposes. The study protocol was approved by the institutional ethics committee and conducted in accordance with the principles outlined in the Declaration of Helsinki.
Kinematic Recordings and Analysis
The kinematic assessment was conducted using an optoelectronic system (SMART motion system, BTS Engineering, Italy), which consisted of three infrared cameras operating at a frequency of 120 Hz. Reflective markers of negligible weight were attached to the participant's hand, with three markers placed at the wrist and two markers on the distal phalanx of the thumb and index finger to evaluate finger tapping movements. Participants were comfortably seated in a chair and instructed to perform ‘as wide and fast as possible’ repetitive opposition movement of the thumb and index finger (finger tapping). Each trial lasted for 15 seconds, and the task was repeated three times for each hand. A rest interval of 60 seconds was provided between trials to prevent fatigue [2, 34, 39].
The kinematic recordings were analyzed using dedicated software (SMART Analyzer, BTS, Milan, Italy). This software utilized an automatized algorithm and linear regression techniques to calculate the relevant kinematic variables, including the number of movements, amplitude (in degrees), velocity (in degrees per second), as well as amplitude and velocity decrement during 15 seconds of repetitive finger movements. Additionally, the coefficient of variation (CV) was also measured to quantify movement rhythm. The CV was calculated by dividing the standard deviation by the mean value of the inter-tap intervals, with higher CV values indicating less rhythmic repetitive movements [2, 34, 39]. In ET, we performed also postural tremor analysis. To this aim, we used two markers placed on each hand. Three 45-sec recordings of postural tremor were obtained with the upper limbs positioned forward to the chest [2, 40,41,42,43]. Tremor analysis was performed using the same dedicated software (SMART Analyzer, BTS Engineering, Italy). The magnitude of tremor was analyzed by measuring the root-mean-square (RMS) of the acceleration traces of the reference marker (on the second metacarpal bone) in 3D space and then was expressed in GRMS^2. Power spectra were quantified by means of fast Fourier transformation [2, 40,41,42,43]. We then measured the dominant frequency peak (Hz) of postural tremor.
MRI Acquisition
Participants underwent a multimodal 3T-MRI scan using a 12-channel head coil for parallel imaging (Verio, Siemens AG). The MRI protocol included a high-resolution 3-dimensional T1-weighted MPRAGE (3D T1) sequence with 176 contiguous sagittal slices, 1-mm thick (TR = 1900 ms, TE = 2.93 ms, flip angle = 9˚, matrix = 256 × 256, FOV = 260 mm^2). T2-weighted images were also acquired (TR = 3320 ms, TE = 10/103 ms, FOV = 220 mm^2, 384 × 384 matrix, 25 4-mm thick slices, 30% gap). Additionally, blood oxygenation level-dependent (BOLD) single-shot echo-planar images were acquired (TR = 3000 ms, TE = 30 ms, flip angle = 89˚, 64 × 64 matrix, 50 slices, 140 volumes, acquisition time = 7 min, voxel size 3 mm^3). During the MRI scan, participants were instructed to lie down with their eyes closed and remain awake.
MRI Analysis
Structural and functional data were pre-processed using FMRIB’s Software Library (FSL), version 6.0.1 (http://fsl.fmrib.ox.ac.uk/fsl).
Structural MRI
Three-dimensional (3D) T1-weighted images were skull stripped using FSL’s Brain Extraction Tool (BET) followed by segmentation into grey matter (GM) white matter (WM) and cerebrospinal fluid (CSF) via FMRIB automated segmentation tool (FAST). Brain tissue volumes, normalized for head size, were estimated with SIENAX [44]. Volumes of subcortical grey matter structures were calculated by FMRIB’s Integrated Registration and Segmentation Tool (FIRST), part of FSL (http://fsl.fmrib.ox.ac.uk/fsl/fslwiki/FIRST).
To calculate cerebellar volume on the 3D T1 images, we used the spatially unbiased infratentorial template toolbox (SUIT), version 3.4 (http://www.diedrichsenlab.org/imaging.suit.htm), implemented in SPM12 (http://www.fil.ion.ucl.ac.uk/spm) running under MATLAB R2020. The following steps were performed with SUIT: 1) extraction of each subject's cerebellum from 3DT1 anatomical images; 2) normalization of the isolated cerebellum to the SUIT atlas template space using the affine transformation matrix and non-linear flow field; in particular, in the present work the suit_normalize_dentate module of SUIT normalization was used to ensure accurate individual isolation of the DN 3) re-slicing of the cerebellum, in order to preserve the volume of cerebellar lobules in the SUIT atlas template space. Lastly, the obtained SUIT atlas was realigned back to the native subject space. For each subject, we parceled and computed 28 cerebellar lobules and 6 nuclei (dentate, interposed and fastigial). Left and right cerebellar volumes were computed as the sum of lobules I–IV, V, VI, Crus I, Crus II, VIIa, VIIIa, VIIIb, IX, and X and used for further statistical analyses. Left and right dentate volumes were also extracted.
Functional MRI
Preprocessing of functional data included the following steps: removal of the first three volumes to allow the signal to reach equilibrium; spatial smoothing at 4 mm full width at half maximum Gaussian kernel; movement removal with independent component analysis- automatic removal of motion artifacts (ICA-AROMA) [45] application of a band-pass filter [0.008-0.09 Hz] to exclude physiological artifacts; and further movement and artifact correction via WM and CSF signal regression. A two-step procedure for the linear/non-linear registration of subject functional images on standard space was implemented using FMRIB’s linear image registration tool (FLIRT) and FMRIB’s non-linear registration tool (FNIRT).
Seed Description
For seed-based analyses, regions of interest (ROIs) were created using 2-mm-radius spheres centered on reference MNI coordinates. For DN, dorsal and ventral seeds, corresponding to motor and non-motor functional territories, were defined following previous studies [46, 47] (right dorsal: x= 12, y= -57, z= -30; left dorsal: x= -12, y= -57, z= -30; right ventral: x= 17, y= -65, z= -35; left ventral: x= -17, y= -65, z= -35).
For the GP, GPe and GPi seeds, corresponding to the inhibitory indirect and excitatory direct pathways, were defined according to Tarcijonas et al. [48] (right GPe: x= 17, y= 4, z= 1; left GPe: x= −15, y= 4, z= −4; right GPi: x= 15, y= −1, z= −2; left GPi: x= −17, y= −3, z= −4).
For each subject, left and right dorsal and ventral DN as well as left and right GPe and GPi were combined in bilateral masks and transformed into the functional space using both linear and non-linear deformations. Seed-based analyses were performed using FSL’s FMRI Expert Analysis Tool (FEAT). For each subject, the mean time series was calculated within each of the selected 4 ROIs and used as seeds in the analyses. Voxel-wise maps of FC were calculated between each seed and the rest of the brain for each individual participant via a general linear model (GLM).
Statistical analysis
Statistical analysis was performed using SPSS software (IBM SPSS Statistics, Version 25.0. Armonk, NY: IBM Corp.). Age was compared using the Mann-Whitney U test, while gender was compared using the Fisher's exact test between the patient and control groups.
Kinematic data
In a preliminary analysis, paired sample t-tests were used to compare the kinematic variables of tremor and finger tapping movements of two sides of the body in both groups (ET and HS). After demonstrating no difference between sides in either group, we calculated the averages of kinematic variables of both sides and used them for group comparison by unpaired sample t-tests. The Bonferroni correction, was to account for multiple comparisons when conducting t-tests, thereby minimizing the risk of type I errors.
MRI Structural data
Group differences in terms of GM and WM volumes, volumes of deep grey matter structures, left and right cerebellar volumes and DN were tested via non-parametric test (Mann-Whitney U test), Bonferroni corrected (21-ROIs; corrected alpha level = 0.002).
MRI Functional data
Maps of dorsal and ventral DN- and GPe and GPi-FC were assessed voxel-wise in the single groups of patients and HS (one-sample t-test), and between groups (two sample unpaired t-test), via non-parametric tests (FSL randomise, 5000 permutations), including age, sex, and GM volume as covariates of no interest.
Results were corrected using false discovery rate (FDR) correction [49] for multiple comparisons (p < 0.05). The minimum cluster extent was set at 100 voxels.
Correlation between kinematic and MRI data
In both HS and ET patients’ groups, voxel-wise correlations between either dorsal and ventral DN- or GPe and GPi-FC maps and finger tapping velocity were non parametrically performed (FSL randomise, 5000 permutations), with age and gender as covariates of no interest. For ET patients we also included tremor severity (GRMS^2) as covariate of no interest. Results were corrected using FDR correction [49] for multiple comparisons (p < 0.05). The minimum cluster extent was set at 100 voxels.
As supplementary analyses, we also performed voxel-wise correlations between dorsal and ventral DN and GPe and GPi FC maps and essential tremor severity (see Supplementary Materials for further details).
Results
Clinical and demographic data
There were no significant differences between ET patients and HS in terms of age (p=0.10), gender distribution (p=0.71), and MOCA scores (p=0.11). The demographic and clinical characteristics of the subjects are presented in Table 1.
In the ET group, the FTMTRS score was 17.7 ± 10.8, and the MDS-UPDRS-III score was 6.2 ± 3.0, with the main influence coming from the postural and kinetic tremor components (as assessed by items 3.14 and 3.15). However, none of the patients exhibited other clinically-detectable symptoms that would warrant an alternative diagnosis [50].
Kinematic Data
ET subjects had postural upper limb tremor characterized by an average frequency of 6.07 ± 1.22 Hz and an amplitude of 0.38 ± 0.21 GRMS^2. The analysis of finger tapping revealed that ET patients had a reduced number of movements and lower velocity in their finger tapping movements compared to HS (number of movements: 41.00 ± 13.36 vs. 54.63 ± 13.76, p<0.01; velocity: 951.51 ± 187.51 vs. 1126.35 ± 142.92, p<0.01). The analysis of finger tapping movements also indicated a tendency for ET patients to exhibit lower amplitude compared to HS (amplitude: 47.49 ± 8.61 vs. 53.41 ± 8.05, p=0.04. However, it is important to note that this difference did not reach statistical significance after applying the Bonferroni correction for multiple comparisons. Finally, no significant differences were observed in terms of rhythm, and amplitude and velocity slope (sequence effect) between ET and HS (p>0.05) (Table 2).
MRI
In terms of structural MRI findings, no significant differences were observed in the volumes of whole brain GM and WM, cerebellum, and deep gray matter structures between ET patients and HS (p>0.05) (Table 3).
Maps of dorsal and ventral DN- and GPe and GPi-FC in the single groups of patients and HS were reported in the Supplementary Materials (Suppl. Fig. 1, Suppl. Fig.2, Suppl. Table 1 and Suppl. Table 2).
DN
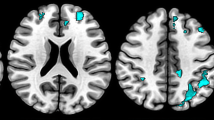
In the between group comparison, ET patients, compared to HS, exhibit higher FC (p < 0.05 FDR corrected) between dorsal DN and several regions, including cerebellum (left lobules VI, VIIb, VIIIa, VIIIb, crus I and II, right lobules I-IV, V and vermis), thalamus and BG, bilateral pre and post-central gyri and bilateral temporal and insular cortices. Additionally, they demonstrate lower FC between dorsal DN and precuneus, right inferior and middle temporal gyri, parieto-occipital cortices and orbitofrontal regions (Fig. 1, Table 4).
Resting-state functional connectivity (rsFC) maps of dorsal and ventral portions of the dentate nucleus (DN) and external and internal segments of the globus pallidus (GPe and GPi) comparing essential tremor (ET) patients with healthy subjects (HS). The color bar represents the t statistic of FC differences between the two groups. Red-yellow areas indicate where FC was significantly higher in ET patients than in HS, and blue-light blue areas indicate where FC was significantly lower in ET patients than in HS. Statistical significance was considered at p<0.05, False Discovery Rate (FDR) corrected
ET patients also showed higher FC when compared to HS between ventral DN and several regions including the cerebellum (left lobule VI and VIIb, right lobules I-IV, lobule V and VI, bilateral crus I and II and vermis), thalamus, BG, insular and temporal cortices, supramarginal gyri and orbitofrontal regions. Additionally, ET patients exhibited lower FC between ventral DN and brainstem, temporal regions including para-hippocampal gyri and left hippocampus (Fig. 1, Table 4).
GP
In the between group comparison, ET patients showed higher FC (p < 0.05 FDR corrected) between the GPe and several regions including the cerebellum (right lobule IX, crus I and left lobule X), brainstem, right putamen, right occipital and parietal regions, insular cortex, bilateral frontal pole and inferior frontal gyri. Additionally, ET patients exhibited lower FC, compared to HS, between GPe and the cerebellum (right lobule VIIb, crus I and II), left superior and middle frontal gyri, left frontal medial cortex and right middle and inferior temporal gyri (Fig. 1, Table 5).
Furthermore, ET compared to HS showed higher FC between the GPi and the cerebellum (bilateral crus I, lobules VI, VIIb, VIIIa, VIIIb, IX, left crus II and lobule X), brainstem, right putamen, right temporal pole and insular cortex, precuneus, parieto-occipital regions, pre- and post-central gyri, middle and inferior frontal gyri and orbitofrontal regions. Additionally, ET exhibited lower FC between GPi and right temporal regions and brainstem (Fig. 1, Table 5).
Correlation Between Kinematic and MRI Data
DN
In HS, dorsal DN-FC with the cerebellum (lobules V-VI, left lobules I-IV, left crus I and II and vermis), brainstem and occipital fusiform cortex was positively correlated with finger tapping velocity. Instead, dorsal DN-FC with left thalamus, lateral occipital cortices, precuneus and left frontal cortex was negatively correlated with finger tapping velocity (Fig. 2, Table 6).
Correlation maps between velocity of finger tapping and dorsal portion of the dentate nucleus (DN) rsFC and external and internal segments of the globus pallidus (GPe and GPi) rsFC in HS and ET patients. Positive correlations are shown in red-yellow color, and negative correlations are shown in blue-light blue color. The color bar represents the t statistic of correlation between rsFC of the ROIs and clinical data. Significant correlation was reached if p < 0.05 (FDR corrected)
In ET patients, dorsal DN-FC with the cerebellum (lobules I-IV and right lobule V), brainstem, BG, left occipital pole, parietal operculum cortex bilaterally, insular and temporal cortices as well as pre and postcentral gyri was positively correlated with finger tapping velocity.
No correlation was found between ventral DN- FC and finger tapping velocity neither in HS nor in ET patients (Fig. 2, Table 6).
GP
In HS, GPe-FC with left putamen and insular cortex was positively correlated with finger tapping velocity. Additionally, GPe-FC with left caudate, pallidum and thalamus, right putamen, hippocampus and amygdala, insular and temporal cortices and right precentral gyrus was negatively correlated with finger tapping velocity (Fig. 2, Table 6).
In ET patients, GPe-FC with several cerebellar regions (lobules I-IV, left lobules V, VI, VIIb, VIIIa and crus I), putamen, left caudate, insular cortex, temporo-parietal regions, supplementary motor area, pre and post-central gyri and frontal cortices was positively correlated with finger tapping velocity. Additionally, GPe-FC with frontal pole, cingulate and paracingulate gyri exhibited a negative correlation between with finger tapping velocity (Fig. 2, Table 6).
In HS, GPi-FC with left putamen and pallidum, paracingulate gyrus and left insular cortex was positively correlated with finger tapping velocity.
In ET patients, GPi-FC with the cerebellum (bilateral crus I, right crus II and lobule VI), right putamen, brainstem, insular and temporal cortices, left postcentral gyrus, right superior and middle frontal gyri was positively correlated with finger tapping velocity (Fig. 2, Table 6).
For ET patients, we also found significant correlations between dorsal and ventral DN and GPe and GPi-FC and essential tremor severity (FMTRS scores). Results are reported in the Supplementary Materials (Suppl. Fig. 3 and Suppl. Table 3).
Discussion
The objective of this study was to explore the potential relationship between the structural and functional characteristics of the cerebellum and BG and objective measures of altered voluntary movement execution in individuals with ET. By doing so, we aimed to better understand the pathophysiology of altered movement execution in ET. Our findings confirm that individuals with ET exhibit altered execution of repetitive finger tapping, characterized by bradykinesia (slowness of movement), without the presence of other abnormalities [6], as identified through kinematic analysis. Our morphometric analysis did not reveal any significant changes in global, cerebellar, and pallidal volumes between individuals with ET and HS, accordingly with previous studies [51, 52]. Although some earlier studies have demonstrated white matter alterations in ET [53], a consistent reproducible pattern of atrophy has not been conclusively demonstrated in this condition [51, 52]. Interestingly, our data demonstrate a trend to volume reduction in bilateral GP of ET patients, in line with previous observations of bilateral GP iron deposition [54]. However, patients exhibited complex patterns of altered FC involving both the cerebellum and the BG. Interestingly, impaired movement execution, i.e., a lower movement velocity, was associated with decreased DN and GP-FC with cerebellar areas, striatum and sensorimotor areas.
Slowed Voluntary Movement Execution in ET
The present study shows that ET patients perform sequential finger movement at lower speed that normal subjects. We have previously interpreted this finding as a consequence of a cerebellum involvement [2, 7, 42, 43], based on experimental observation demonstrating that the cerebellum encodes various kinematic parameters, including movement velocity, and that cerebellar diseases may be associated with movement slowness (bradykinesia) [7, 25].
Increased Cerebellar Activity, and DN Motor Shift in ET
The first novel finding to be discussed is the evidence of increased activity of the cerebellar internal circuitry in ET patients, involving both anterior and posterior lobules. Also, we provided evidence of an altered FC between the cerebellum and various cortical areas, likely mediated by pathways that traverse the thalamic nuclei [18,19,20,21, 55]. In detail, we found that ET patients showed increased FC between both the dorsal and ventral DN and anterior and posterior cerebellar lobules. This finding is in line with existing evidence highlighting the involvement of both anterior and posterior cerebellar lobules in ET, as demonstrated by Buijink and colleagues [56]. ET patients demonstrated increased FC of dorsal DN with areas part of habitual motor network including thalamus, BG and bilateral somatosensory cortices, while demonstrating reduced functional connectivity with multimodal associative cortices. Intriguingly, a similar pattern is evidenced for the ventral portion of the DN, classically deputed to associative connections.
These findings are consistent with previous studies and support the notion of impaired connectivity between the cerebellum and multimodal associative areas, which may contribute to ET pathophysiology [16, 17, 57,58,59]. Moreover, these results evidence a shift of DN towards increased connectivity with motor network areas. This shift may reflect deregulated increased connectivity for dorsal DN, but also a neural plasticity adaptation concerning ventral DN connectivity, that in normal condition has a main associative role.
Increased GPi Connectivity in ET
Equally important, our study highlights the significance of FC abnormalities of both the DN and the striatum as well as between the cerebellar hemispheres responsible for sensory-motor integration (specifically the antero-lateral hemispheric cerebellar lobules) and the GP [17]. The GPe, important relay nuclei in the indirect BG pathway, demonstrated increased connectivity with cerebellar areas and striatum, while demonstrating alternatively increased and decreased connectivity with multiple cortical areas. The GPi, serving as the primary output structure of the BG, demonstrated increased FC with components of habitual motor network such as cerebellar lobules, brainstem, striatum and somatosensory motor cortices, as well as different neocortical areas. The observation of enhanced FC of GP, especially within the habitual motor network, can be interpreted in two distinct ways. Firstly, it might indicate a primary pathological manifestation of altered GP activity, or it could potentially be a compensatory mechanism, in an effort to counterbalance the uncontrolled activation of the cerebellum [60,61,62,63,64]. Remarkably, high-frequency, desynchronized GP activity and increased connectivity with cerebellum and cortical motor areas have been observed in both patients and animal models of Parkinson's disease (PD) [60,61,62,63,64]. These findings have, in some instances, been associated with poorer motor performance or the progression of motor symptoms in patients. In ET patients augmented GP connectivity was associated with poorer cognitive performance [58, 65], but scarce evidences regard motor manifestation in ET and GP activity. The presence of similar abnormalities in GP connectivity patterns in ET patients raises intriguing questions regarding shared neurophysiological mechanisms between ET and PD, particularly concerning voluntary motor execution.
Reduced Voluntary Movement Velocity in ET Associates with Weaker Motor Network FC
When considering the correlations between neuroimaging and kinematic data, our study revealed that decreased finger tapping velocity in ET patients was associated with weaker FC between both dorsal DN and GPi with the motor network encompassing the cerebellar (antero-lateral cerebellar hemispheres)-thalamo-striatal-sensorimotor cortex. GPe exhibited a peculiar relation with finger tapping velocity in ET. In fact while in HS GPe-FC within habitual motor network and temporo-insular cortices had mainly negative correlation with movement velocity, in ET GPe-FC with the same structures was demonstrated to be positive, involving also GPe-FC with cerebellar areas. Repetitive motor tasks, such as finger tapping, require precise and coordinated activation and inhibition of brain regions involved in motor control. Our findings underscore the significance of both cerebellar and BG activity in facilitating optimal motor performance. Proper activity in these structures enables enhanced movement velocity while minimizing reliance on higher cortical structures for movement preparation and planning. As a result, both cerebellar and BG facilitates efficient motor execution [26, 27]. Hence, we observed increased connectivity of GP and DN portions with cerebellar and motor network areas in ET patients and a positive correlation between the GP- and DN-FC and faster voluntary movement execution. This suggests a potential compensatory role of observed findings, in an attempt to counterbalance the reduced voluntary motor performance in ET patients. Adjunctively, connectivity outside habitual motor network, especially with temporo-insular areas, was correlated with better motor performance, thus reinforcing the hypothesis of a compensatory origin of the observed findings. Increased activity within the motor network as well as a recruitment of non-motor areas in an effort to improve motor performance can constitute a compensatory network, that in an overloading context can potentially lead to imbalances in global brain activity with detrimental effects.
Previous studies demonstrated altered FC in cerebellar and pallidal networks, also correlating with poorer motor and non-motor performances, but none of them focused on their role in altered voluntary movement execution in ET patients [15, 17, 55, 56, 58, 59, 65]. Dopamine transporter studies demonstrated reduced striatal dopaminergic uptake in certain subgroups of ET patients [66, 67], and our study recently correlated it with lower finger tapping velocity [33]. Dopaminergic dysfunction can lead to secondary changes in cerebellar activity, in order to sustain motor performance in striatum (putamen)-thalamus-M1 circuit hypofunction, as observed in PD [24]. The potential relationships between alterations in central dopaminergic tone and FC changes between the BG and cerebellum should be object of further exploration in future studies.
Confounding Effect of Tremor and Potential Study Limitations
An important aspect to discuss is the potential confounding effect of tremor on movement related results. The present results extend observations by previous studies that alterations in FC within the cerebellar-thalamus-sensorimotor network is associated with the severity of tremor [17, 55]. More in detail, Tikoo et al demonstrated that tremor severity, tremor amplitude and peak frequency were significantly associated with altered FC of the dentate nucleus with cerebellar areas, sensorimotor cortex and thalamus/BG, respectively as confirmed by our supplementary analyses on clinical tremor severity. In particular, positive correlation with tremor severity included the FC of ventral DN with cerebellar and cortical areas, as well as the GPe-FC with other BG structures, while negative correlation involved both dorsal DN- and GPi-FC with widespread cortical areas. Hence, it could be argued that the results of the present study might reflect the severity of the tremor rather than the impairment of voluntary movement. Importantly, however, in our analysis, we have considered tremor as a covariate of non-interest, thus excluding the possibility that it may have influenced our results. Moreover, a recent study evidenced that movement velocity in ET is not influenced by tremor amplitude, and tremor does not correlate with subtle dopaminergic changes in ET [33]. Thus, we can infer that, like tremor, the underlying pathophysiological mechanisms of impaired movement execution in ET cannot be solely attributed to a singular anatomical structure. Rather, a complex interplay of partially overlapping brain areas contributes to the generation of both tremor and altered movement execution in ET.
This study has some limitations. Firstly, our sample size is relatively small, although it is consistent with the majority of fMRI studies on ET [16, 51], and is composed by a prevalence of men. It is important to consider that ET is a highly heterogeneous condition from a clinical perspective, and our study predominantly focused on patients with intermediate forms of the disease. Therefore, future research is needed to validate the findings of this study on larger and more diverse patient cohorts to further elucidate the potential role played by clinical heterogeneity. Moreover, we excluded patients presenting with ET soft signs, since, especially questionable dystonia, could influence kinematic measures, and alter functional connectivity [68, 69]. Another limitation is the absence of DAT imaging for clinical confirmation of the diagnosis. However, it is important to note that the clinical diagnosis of ET was based on the most recent diagnostic criteria, which do not require DAT imaging [1]. Finally, another potential limitation of the study is that we solely examined repetitive finger movements and did not assess movements of different types or involving other body segments. Consequently, the generalizability of our observations to other types of movements remains uncertain.
Conclusions
Our study contributes to a better understanding of the pathophysiology of ET by highlighting the role of the cerebellum, BG and cerebral cortex within a dysfunctional network. In this regard, functional alterations in the networks may not only influences the generation of tremor but also contributes to impaired motor execution in ET. The results of this study could hold significance within the current research landscape, which is increasingly focused on identifying specific ET subtypes or even distinct individual diseases within the broader spectrum of ET. Such an approach would aid in early recognition of patients who may progress to develop parkinsonian syndromes and shed light on potential diverse underlying causes.
Data Availability
The data of this study are available from the corresponding author, M. Bologna, upon reasonable request.
Abbreviations
- BDI-II:
-
Beck Depression Inventory
- BET:
-
Brain Extraction Tool
- BG:
-
Basal Ganglia
- BOLD:
-
Blood Oxygenation Level-Dependent
- BTS:
-
BTS Engineering
- CSF:
-
Cerebrospinal Fluid
- CV:
-
Coefficient of Variation
- DN:
-
Dentate Nucleus
- ET:
-
Essential Tremor
- FAST:
-
FMRIB Automated Segmentation Tool
- FC:
-
Functional Connectivity
- FDR:
-
False discovery rate
- FIRST:
-
FMRIB's Integrated Registration and Segmentation Tool
- FLIRT:
-
FMRIB's Linear Image Registration Tool
- FNIRT:
-
FMRIB's Non-Linear Image Registration Tool
- FOV:
-
Field of View
- FSL:
-
FMRIB's Software Library
- FTMTRS:
-
Fahn-Tolosa-Marin Tremor Rating Scale
- GM:
-
Grey Matter
- GP:
-
Globus Pallidus
- GPi:
-
Internal Globus Pallidus
- GPe:
-
External Globus Pallidus
- GRMS^2:
-
G root mean square squared
- HS:
-
Healthy Subjects
- ICA-AROMA:
-
Independent Component Analysis-Automatic Removal of Motion Artifacts
- MDS-UPDRS-III:
-
Movement Disorder Society - Unified Parkinson’s Disease Rating Scale, part III (motor section)
- MNI:
-
Montreal Neurological Institute
- MoCA:
-
Montreal Cognitive Assessment
- MPRAGE:
-
Magnetization-Prepared Rapid Gradient-Echo
- MRI:
-
Magnetic Resonance Imaging
- PD:
-
Parkinson's Disease
- RMS:
-
Root-Mean-Square
- rs-fMRI:
-
resting-state functional magnetic resonance imaging
- SIENAX:
-
Structural Imaging Evaluation of Normalized Atrophy
- SMA:
-
Supplementary motor area
- SMART:
-
System SMART motion
- SPSS:
-
Statistical Package for the Social Sciences
- SUIT:
-
Spatially Unbiased Infratentorial Template
- WM:
-
White Matter
References
Bhatia KP, Bain P, Bajaj N, Elble RJ, Hallett M, Louis ED, Raethjen J, Stamelou M, Testa CM, Deuschl G, the Tremor Task Force of the International Parkinson and Movement Disorder Society. Consensus Statement on the classification of tremors. from the task force on tremor of the International Parkinson and Movement Disorder Society: IPMDS Task Force on Tremor Consensus Statement. Mov Disord. 2018;33:75–87. https://doi.org/10.1002/mds.27121.
Bologna M, Paparella G, Colella D, Cannavacciuolo A, Angelini L, Alunni-Fegatelli D, Guerra A, Berardelli A. Is there evidence of bradykinesia in essential tremor? Eur J Neurol. 2020;27:1501–9. https://doi.org/10.1111/ene.14312.
Duval C, Sadikot AF, Panisset M. Bradykinesia in patients with essential tremor. Brain Res. 2006;1115:213–6. https://doi.org/10.1016/j.brainres.2006.07.066.
Goubault E, Nguyen HP, Ayachi FS, Bogard S, Duval C. Do Bradykinesia and Tremor Interfere in Voluntary Movement of Essential Tremor Patients? Preliminary Findings. Tremor Hyperkinetic Mov. 2017;7:459. https://doi.org/10.5334/tohm.341.
Jiménez-Jiménez FJ, Rubio L, Alonso-Navarro H, Calleja M, Pilo-de-la-Fuente B, Plaza-Nieto JF, Benito-León J, García-Ruiz PJ, Agúndez JAG. Impairment of rapid repetitive finger movements and visual reaction time in patients with essential tremor: Motor performance in essential tremor. Eur J Neurol. 2010;17:152–9. https://doi.org/10.1111/j.1468-1331.2009.02784.x.
Bologna M, Espay AJ, Fasano A, Paparella G, Hallett M, Berardelli A. Redefining Bradykinesia. Mov Disord Off J Mov Disord Soc. 2023;38:551–7. https://doi.org/10.1002/mds.29362.
Paparella G, Fasano A, Hallett M, Berardelli A, Bologna M. Emerging concepts on bradykinesia in non-parkinsonian conditions. Eur J Neurol. 2021. https://doi.org/10.1111/ene.14851.
Benito-León J, Labiano-Fontcuberta A. Linking Essential Tremor to the Cerebellum: Clinical Evidence. The Cerebellum. 2016;15:253–62. https://doi.org/10.1007/s12311-015-0741-1.
Fanning A, Kuo S-H. Clinical Heterogeneity of Essential Tremor: Understanding Neural Substrates of Action Tremor Subtypes. The Cerebellum. 2023. https://doi.org/10.1007/s12311-023-01551-3.
Haubenberger D, Hallett M. Essential Tremor. N Engl J Med. 2018;378:1802–10. https://doi.org/10.1056/NEJMcp1707928.
Helmich RC, Toni I, Deuschl G, Bloem BR. The Pathophysiology of Essential Tremor and Parkinson’s Tremor. Curr Neurol Neurosci Rep. 2013;13:378. https://doi.org/10.1007/s11910-013-0378-8.
Muthuraman M, Heute U, Arning K, Anwar AR, Elble R, Deuschl G, Raethjen J. Oscillating central motor networks in pathological tremors and voluntary movements What makes the difference? NeuroImage. 2012;60:1331–9. https://doi.org/10.1016/j.neuroimage.2012.01.088.
Bédard P, Panyakaew P, Cho H-J, Hallett M, Horovitz SG. Multimodal imaging of essential tremor and dystonic tremor. NeuroImage Clin. 2022;36:103247. https://doi.org/10.1016/j.nicl.2022.103247.
Mueller K, Jech R, Hoskovcová M, Ulmanová O, Urgošík D, Vymazal J, Růžička E. General and selective brain connectivity alterations in essential tremor: A resting state fMRI study. NeuroImage Clin. 2017;16:468–76. https://doi.org/10.1016/j.nicl.2017.06.004.
Nicoletti V, Cecchi P, Pesaresi I, Frosini D, Cosottini M, Ceravolo R. Cerebello-thalamo-cortical network is intrinsically altered in essential tremor: evidence from a resting state functional MRI study. Sci Rep. 2020;10:16661. https://doi.org/10.1038/s41598-020-73714-9.
Pietracupa S, Bologna M, Tommasin S, Berardelli A, Pantano P. The Contribution of Neuroimaging to the Understanding of Essential Tremor Pathophysiology: a Systematic Review. The Cerebellum. 2021;21:1029–51. https://doi.org/10.1007/s12311-021-01335-7.
Tikoo S, Pietracupa S, Tommasin S, Bologna M, Petsas N, Bharti K, Berardelli A, Pantano P. Functional disconnection of the dentate nucleus in essential tremor. J Neurol. 2020;267:1358–67. https://doi.org/10.1007/s00415-020-09711-9.
Matano S. Brief communication: Proportions of the ventral half of the cerebellar dentate nucleus in humans and great apes. Am J Phys Anthropol. 2001;114:163–5. https://doi.org/10.1002/1096-8644(200102)114:2%3c163::AID-AJPA1016%3e3.0.CO;2-F.
Hoover JE, Strick PL. The organization of cerebellar and basal ganglia outputs to primary motor cortex as revealed by retrograde transneuronal transport of herpes simplex virus type 1. J Neurosci Off J Soc Neurosci. 1999;19:1446–63. https://doi.org/10.1523/JNEUROSCI.19-04-01446.1999.
Middleton FA, Strick PL. Cerebellar output channels. Int Rev Neurobiol. 1997;41:61–82. https://doi.org/10.1016/s0074-7742(08)60347-5.
Middleton FA, Strick PL. Cerebellar projections to the prefrontal cortex of the primate. J Neurosci Off J Soc Neurosci. 2001;21:700–12. https://doi.org/10.1523/JNEUROSCI.21-02-00700.2001.
Hoshi E, Tremblay L, Féger J, Carras PL, Strick PL. The cerebellum communicates with the basal ganglia. Nat Neurosci. 2005;8:1491–3. https://doi.org/10.1038/nn1544.
Buijink AWG, Broersma M, van der Stouwe AMM, van Wingen GA, Groot PFC, Speelman JD, Maurits NM, van Rootselaar AF. Rhythmic finger tapping reveals cerebellar dysfunction in essential tremor. Parkinsonism Relat Disord. 2015;21:383–8. https://doi.org/10.1016/j.parkreldis.2015.02.003.
Wu T, Hallett M. The cerebellum in Parkinson’s disease. Brain. 2013;136:696–709. https://doi.org/10.1093/brain/aws360.
Bologna M, Paparella G, Fasano A, Hallett M, Berardelli A. Evolving concepts on bradykinesia. Brain J Neurol. 2020;143:727–50. https://doi.org/10.1093/brain/awz344.
Redgrave P, Rodriguez M, Smith Y, Rodriguez-Oroz MC, Lehericy S, Bergman H, Agid Y, DeLong MR, Obeso JA. Goal-directed and habitual control in the basal ganglia: implications for Parkinson’s disease. Nat Rev Neurosci. 2010;11:760–72. https://doi.org/10.1038/nrn2915.
Jahanshahi M, Obeso I, Rothwell JC, Obeso JA. A fronto–striato–subthalamic–pallidal network for goal-directed and habitual inhibition. Nat Rev Neurosci. 2015;16:719–32. https://doi.org/10.1038/nrn4038.
Jaeger D, Kita H. Functional connectivity and integrative properties of globus pallidus neurons. Neuroscience. 2011;198:44–53. https://doi.org/10.1016/j.neuroscience.2011.07.050.
Blenkinsop A, Anderson S, Gurney K. Frequency and function in the basal ganglia: the origins of beta and gamma band activity. J Physiol. 2017;595:4525–48. https://doi.org/10.1113/JP273760.
Nishibayashi H, Ogura M, Kakishita K, Tanaka S, Tachibana Y, Nambu A, Kita H, Itakura T. Cortically evoked responses of human pallidal neurons recorded during stereotactic neurosurgery. Mov Disord. 2011;26:469–76. https://doi.org/10.1002/mds.23502.
Villalobos N, Almazán-Alvarado S, Magdaleno-Madrigal VM. Elevation of GABA levels in the globus pallidus disinhibits the thalamic reticular nucleus and desynchronized cortical beta oscillations. J Physiol Sci JPS. 2022;72:17. https://doi.org/10.1186/s12576-022-00843-3.
Caligiuri ME, Arabia G, Barbagallo G, Lupo A, Morelli M, Nisticò R, Novellino F, Quattrone A, Salsone M, Vescio B, Cherubini A, Quattrone A. Structural connectivity differences in essential tremor with and without resting tremor. J Neurol. 2017;264:1865–74. https://doi.org/10.1007/s00415-017-8553-5.
Colella D, Passaretti M, Frantellizzi V, Silvia De Feo M, Cannavacciuolo A, Angelini L, Birreci D, Costa D, Paparella G, Guerra A, De Vincentis G, Berardelli A, Bologna M. Subtle changes in central dopaminergic tone underlie bradykinesia in essential tremor. NeuroImage Clin. 2023;40:103526. https://doi.org/10.1016/j.nicl.2023.103526.
Bologna M, Leodori G, Stirpe P, Paparella G, Colella D, Belvisi D, Fasano A, Fabbrini G, Berardelli A. Bradykinesia in early and advanced Parkinson’s disease. J Neurol Sci. 2016;369:286–91. https://doi.org/10.1016/j.jns.2016.08.028.
Elble R, Comella C, Fahn S, Hallett M, Jankovic J, Juncos JL, LeWitt P, Lyons K, Ondo W, Pahwa R, Sethi K, Stover N, Tarsy D, Testa C, Tintner R, Watts R, Zesiewicz T. Reliability of a new scale for essential tremor. Mov Disord. 2012;27:1567–9. https://doi.org/10.1002/mds.25162.
MDS-UPDRS Italian Validation Study Group, Antonini A, Abbruzzese G, Ferini-Strambi L, Tilley B, Huang J, Stebbins GT, Goetz CG, Barone P, Bandettini di Poggio M, Fabbrini G, Di Stasio F, Tinazzi M, Bovi T, Ramat S, Meoni S, Pezzoli G, Canesi M, Martinelli P, Maria Scaglione CL, Rossi A, Tambasco N, Santangelo G, Picillo M, Morgante L, Morgante F, Quatrale R, Sensi M, Pilleri M, Biundo R, Nordera G, Caria A, Pacchetti C, Zangaglia R, Lopiano L, Zibetti M, Zappia M, Nicoletti A, Quattrone A, Salsone M, Cossu G, Murgia D, Albanese A, Del Sorbo F. Validation of the Italian version of the Movement Disorder Society—Unified Parkinson’s Disease Rating Scale. Neurol Sci. 2013. 34:683–687 https://doi.org/10.1007/s10072-012-1112-z
Freitas S, Simões MR, Alves L, Santana I. Montreal Cognitive Assessment: Validation Study for Mild Cognitive Impairment and Alzheimer Disease. Alzheimer Dis Assoc Disord. 2013;27:37–43. https://doi.org/10.1097/WAD.0b013e3182420bfe.
Beck AT. An Inventory for Measuring Depression. Arch Gen Psychiatry. 1961;4:561. https://doi.org/10.1001/archpsyc.1961.01710120031004.
Colella D, Guerra A, Paparella G, Cioffi E, Di Vita A, Trebbastoni A, Berardelli A, Bologna M. Motor dysfunction in mild cognitive impairment as tested by kinematic analysis and transcranial magnetic stimulation. Clin Neurophysiol. 2021;132:315–22. https://doi.org/10.1016/j.clinph.2020.10.028.
Paparella G, Angelini L, De Biase A, Cannavacciuolo A, Colella D, Di Bonaventura C, Giallonardo AT, Berardelli A, Bologna M. Clinical and Kinematic Features of Valproate-Induced Tremor and Differences with Essential Tremor. Cerebellum Lond Engl. 2020. https://doi.org/10.1007/s12311-020-01216-5.
Paparella G, Ferrazzano G, Cannavacciuolo A, Cogliati Dezza F, Fabbrini G, Bologna M, Berardelli A. Differential effects of propranolol on head and upper limb tremor in patients with essential tremor and dystonia. J Neurol. 2018. https://doi.org/10.1007/s00415-018-9052-z.
Angelini L, Paparella G, De Biase A, Maraone A, Panfili M, Berardelli I, Cannavacciuolo A, Di Vita A, Margiotta R, Fabbrini G, Berardelli A, Bologna M. Longitudinal study of clinical and neurophysiological features in essential tremor. Eur J Neurol. 2022. https://doi.org/10.1111/ene.15650.
Passaretti M, De Biase A, Paparella G, Angelini L, Cannavacciuolo A, Colella D, Berardelli A, Bologna M. Worsening of Essential Tremor After SARS-CoV-2 Infection. Cerebellum Lond Engl. 2022. https://doi.org/10.1007/s12311-022-01366-8.
Smith SM, Zhang Y, Jenkinson M, Chen J, Matthews PM, Federico A, De Stefano N. Accurate, Robust, and Automated Longitudinal and Cross-Sectional Brain Change Analysis. NeuroImage. 2002;17:479–89. https://doi.org/10.1006/nimg.2002.1040.
Pruim RHR, Mennes M, Buitelaar JK, Beckmann CF. Evaluation of ICA-AROMA and alternative strategies for motion artifact removal in resting state fMRI. NeuroImage. 2015;112:278–87. https://doi.org/10.1016/j.neuroimage.2015.02.063.
Anteraper SA, Guell X, Taylor HP, D’Mello A, Whitfield-Gabrieli S, Joshi G. Intrinsic Functional Connectivity of Dentate Nuclei in Autism Spectrum Disorder. Brain Connect. 2019;9:692–702. https://doi.org/10.1089/brain.2019.0692.
Bernard JA, Peltier SJ, Benson BL, Wiggins JL, Jaeggi SM, Buschkuehl M, Jonides J, Monk CS, Seidler RD. Dissociable functional networks of the human dentate nucleus. Cereb Cortex N Y N. 2014;1991(24):2151–9. https://doi.org/10.1093/cercor/bht065.
Tarcijonas G, Foran W, Haas GL, Luna B, Sarpal DK. Intrinsic Connectivity of the Globus Pallidus: An Uncharted Marker of Functional Prognosis in People With First-Episode Schizophrenia. Schizophr Bull. 2020;46:184–92. https://doi.org/10.1093/schbul/sbz034.
Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J R Stat Soc Ser B Methodol. 1995;57:289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x.
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord Off J Mov Disord Soc. 2015;30:1591–601. https://doi.org/10.1002/mds.26424.
Holtbernd F, Shah NJ. Imaging the Pathophysiology of Essential Tremor-A Systematic Review. Front Neurol. 2021;12:680254. https://doi.org/10.3389/fneur.2021.680254.
Luo R, Pan P, Xu Y, Chen L. No reliable gray matter changes in essential tremor. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. 2019;40:2051–63. https://doi.org/10.1007/s10072-019-03933-0.
Pietracupa S, Bologna M, Bharti K, Pasqua G, Tommasin S, Elifani F, Paparella G, Petsas N, Grillea G, Berardelli A, Pantano P. White matter rather than gray matter damage characterizes essential tremor. Eur Radiol. 2019;29:6634–42. https://doi.org/10.1007/s00330-019-06267-9.
Novellino F, Cherubini A, Chiriaco C, Morelli M, Salsone M, Arabia G, Quattrone A. Brain iron deposition in essential tremor: a quantitative 3-Tesla magnetic resonance imaging study. Mov Disord Off J Mov Disord Soc. 2013;28:196–200. https://doi.org/10.1002/mds.25263.
Fang W, Chen H, Wang H, Zhang H, Puneet M, Liu M, Lv F, Luo T, Cheng O, Wang X, Lu X. Essential tremor is associated with disruption of functional connectivity in the ventral intermediate Nucleus-Motor Cortex–Cerebellum circuit. Hum Brain Mapp. 2016;37:165–78. https://doi.org/10.1002/hbm.23024.
Buijink AWG, van der Stouwe AMM, Broersma M, Sharifi S, Groot PFC, Speelman JD, Maurits NM, van Rootselaar A-F. Motor network disruption in essential tremor: a functional and effective connectivity study. Brain. 2015;138:2934–47. https://doi.org/10.1093/brain/awv225.
Lenka A, Bhalsing KS, Panda R, Jhunjhunwala K, Naduthota RM, Saini J, Bharath RD, Yadav R, Pal PK. Role of altered cerebello-thalamo-cortical network in the neurobiology of essential tremor. Neuroradiology. 2017;59:157–68. https://doi.org/10.1007/s00234-016-1771-1.
Benito-León J, Sanz-Morales E, Melero H, Louis ED, Romero JP, Rocon E, Malpica N. Graph theory analysis of resting-state functional magnetic resonance imaging in essential tremor. Hum Brain Mapp. 2019;40:4686–702. https://doi.org/10.1002/hbm.24730.
Fang W, Chen H, Wang H, Zhang H, Liu M, Puneet M, Lv F, Cheng O, Wang X, Lu X, Luo T. Multiple Resting-State Networks Are Associated With Tremors and Cognitive Features in Essential Tremor. Mov Disord Off J Mov Disord Soc. 2015;30:1926–36. https://doi.org/10.1002/mds.26375.
Filion M, Tremblay L. Abnormal spontaneous activity of globus pallidus neurons in monkeys with MPTP-induced parkinsonism. Brain Res. 1991;547:142–51.
Alamy M, Pons JC, Gambarelli D, Trouche E. A defective control of small-amplitude movements in monkeys with globus pallidus lesions: an experimental study on one component of pallidal bradykinesia. Behav Brain Res. 1995;72:57–62. https://doi.org/10.1016/0166-4328(96)00048-4.
Johnson LA, Aman JE, Yu Y, Escobar Sanabria D, Wang J, Hill M, Dharnipragada R, Patriat R, Fiecas M, Li L, Schrock LE, Cooper SE, Johnson MD, Park MC, Harel N, Vitek JL. High-Frequency Oscillations in the Pallidum A Pathophysiological Biomarker in Parkinson’s Disease? Mov Disord Off J Mov Disord Soc. 2021;36:1332–41. https://doi.org/10.1002/mds.28566.
Connolly AT, Jensen AL, Bello EM, Netoff TI, Baker KB, Johnson MD, Vitek JL. Modulations in oscillatory frequency and coupling in globus pallidus with increasing parkinsonian severity. J Neurosci Off J Soc Neurosci. 2015;35:6231–40. https://doi.org/10.1523/JNEUROSCI.4137-14.2015.
Obeso JA, Rodríguez-Oroz MC, Benitez-Temino B, Blesa FJ, Guridi J, Marin C, Rodriguez M. Functional organization of the basal ganglia: therapeutic implications for Parkinson’s disease. Mov Disord Off J Mov Disord Soc. 2008;23(Suppl 3):S548-559. https://doi.org/10.1002/mds.22062.
Wang L, Lei D, Suo X, Li N, Lu Z, Li J, Peng J, Gong Q, Peng R. Resting-state fMRI study on drug-naive patients of essential tremor with and without head tremor. Sci Rep. 2018;8:10580. https://doi.org/10.1038/s41598-018-28778-z.
Isaias IU, Canesi M, Benti R, Gerundini P, Cilia R, Pezzoli G, Antonini A. Striatal dopamine transporter abnormalities in patients with essential tremor. Nucl Med Commun. 2008;29:349–53. https://doi.org/10.1097/MNM.0b013e3282f4d307.
Isaias IU, Marotta G, Hirano S, Canesi M, Benti R, Righini A, Tang C, Cilia R, Pezzoli G, Eidelberg D, Antonini A. Imaging essential tremor. Mov Disord. 2010;25:679–86. https://doi.org/10.1002/mds.22870.
Brinker D, Granert O, Gövert F, Tödt I, Baumann A, Zeuner KE, Wolke R, Deuschl G, Becktepe JS. Grey matter correlates of dystonic soft signs in essential tremor. Parkinsonism Relat Disord. 2023;112:105457. https://doi.org/10.1016/j.parkreldis.2023.105457.
Nieuwhof F, Toni I, Dirkx MF, Gallea C, Vidailhet M, Buijink AWG, van Rootselaar A-F, van de Warrenburg BPC, Helmich RC. Cerebello-thalamic activity drives an abnormal motor network into dystonic tremor. NeuroImage Clin. 2022;33:102919. https://doi.org/10.1016/j.nicl.2021.102919.
Acknowledgements
The authors express their gratitude to the all the subjects who participated in this study.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. This work was supported by the Italian Ministry of Health (Current Research 2024).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. MP, CP, VB, GaP, DC, SP, NP, LA, AC, GiP: data collection and analysis. MP, GaP, CP, DC: writing of the first draft of the manuscript. PP, AB and MB: study supervision and manuscript revision. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
The study protocol was approved by the institutional ethics committee and conducted in accordance with the principles outlined in the Declaration of Helsinki. Written informed consent to participate and to publish data was provided by each subject involved in the study.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Passaretti, M., Piervincenzi, C., Baione, V. et al. The Role of Cerebellum and Basal Ganglia Functional Connectivity in Altered Voluntary Movement Execution in Essential Tremor. Cerebellum (2024). https://doi.org/10.1007/s12311-024-01699-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s12311-024-01699-6