Abstract
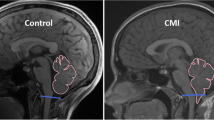
Chiari malformation type I (CMI) provides an opportunity for examining possible moderators of allostatic load. CMI patients who had (n = 43) and had not (n = 19) undergone decompression surgery completed questionnaires regarding pain, disability, and loneliness, and provided serum samples for IL-6, CRP, estrogen, and free estradiol assays, and saliva samples to assess diurnal cortisol curves. ANOVAs examining surgical status (decompressed versus non-decompressed), loneliness (high vs. low), and disability (high vs. low) as independent variables and biomarker variables as dependent factors found that loneliness was associated with higher levels of cortisol, F(1, 37) = 4.91, p = .04, η2P = .11, and lower levels of estrogen, F(1, 36) = 7.29, p = .01, η2P = .17, but only in decompressed patients. Results highlight the possible impact of loneliness on biological stress responses and the need to intervene to reduce loneliness in patients with symptomatic CMI.








Similar content being viewed by others
References
Smith BW, Strahle J, Bapuraj JR, Muraszko KM, Garton HJL, Maher CO. Distribution of cerebellar tonsil position: implications for understanding Chiari malformation: clinical article. J Neurosurg. 2013;119(3):812–9. https://doi.org/10.3171/2013.5.JNS121825.
Chiari Malformation Fact Sheet | National Institute of Neurological Disorders and Stroke. 2016. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Chiari-Malformation-Fact-Sheet.
Fischbein R, Saling JR, Marty P, Kropp D, Meeker J, Amerine J, et al. Patient-reported Chiari malformation type I symptoms and diagnostic experiences: a report from the national Conquer Chiari Patient Registry database. Neurol Sci. 2015;36(9):1617–24. https://doi.org/10.1007/s10072-015-2219-9.
Garcia MA, Allen PA, Li X, Houston JR, Loth F, Labuda R, et al. An examination of pain, disability, and the psychological correlates of Chiari malformation pre- and post-surgical correction. Disabil Health J. 2019;12:649–56. https://doi.org/10.1016/j.dhjo.2019.05.004.
Biswas D, Eppelheimer MS, Houston JR, Ibrahimy A, Bapuraj JR, Labuda R, et al. Quantification of cerebellar crowding in type I chiari malformation. Ann Biomed Eng. 2019;47(3):731–43. https://doi.org/10.1007/s10439-018-02175-z.
Eppelheimer MS, Biswas D, Braun AM, Houston JR, Allen PA, Bapuraj JR, et al. Quantification of changes in brain morphology following posterior fossa decompression surgery in women treated for Chiari malformation type 1. Neuroradiology. 2019;61(9):1011–22. https://doi.org/10.1007/s00234-019-02206-z.
Heiss JD, Patronas N, DeVroom HL, Shawker T, Ennis R, Kammerer W, et al. Elucidating the pathophysiology of syringomyelia. J Neurosurg. 1999;91(4):553–62. https://doi.org/10.3171/jns.1999.91.4.0553.
Khalsa S, Geh N, Allen P, Strahle J, Loth F, Habtzghi D, et al. Morphometric and volumetric comparison of 102 children with symptomatic and asymptomatic Chiari malformation type I. - PubMed—NCBI. J Neurosurg Pediatr. 2018;21(1):65–71. https://doi.org/10.3171/2017.8.PEDS17345.
Smith BW, Strahle J, Kazarian E, Muraszko KM, Garton HJL, Maher CO. Impact of body mass index on cerebellar tonsil position in healthy subjects and patients with Chiari malformation. J Neurosurg. 2015;123(1):226–31. https://doi.org/10.3171/2014.10.JNS141317.
Houston JR, Hughes ML, Lien M-C, Martin BA, Loth F, Luciano MG, et al. An electrophysiological study of cognitive and emotion processing in type I Chiari malformation. Cerebellum. 2018;17(4):404–18. https://doi.org/10.1007/s12311-018-0923-8.
Houston JR, Allen PA, Rogers JM, Lien M-C, Allen NJ, Hughes ML, et al. Type I Chiari malformation, RBANS performance, and brain morphology: connecting the dots on cognition and macrolevel brain structure. Neuropsychology. 2019;33(5):725–38. https://doi.org/10.1037/neu0000547.
Cremeans-Smith JK, Contrera K, Speering L, Miller ET, Pfefferle K, Greene K, et al. Using established predictors of post-traumatic stress to explain variations in recovery outcomes among orthopedic patients. J Health Psychol. 2015;20(10):1296–304. https://doi.org/10.1177/1359105313511135.
Cremeans-Smith JK, Millington K, Sledjeski E, Greene K, Delahanty D. Sleep disruptions mediate the relationship between early postoperative pain and later functioning following total knee replacement surgery. J Behav Med. 2006;29:215–22. https://doi.org/10.1007/s10865-005-9045-0.
Reijnders T, Schuler M, Jelusic D, Troosters T, Janssens W, Schultz K, et al. The Impact of Loneliness on Outcomes of Pulmonary Rehabilitation in Patients with COPD. COPD. 2018;15:446–53. https://doi.org/10.1080/15412555.2018.1471128.
McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896(1):30–47. https://doi.org/10.1111/j.1749-6632.1999.tb08103.x.
Juster R-P, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35(1):2–16. https://doi.org/10.1016/j.neubiorev.2009.10.002.
Allen PA, Houston JR, Pollock JW, Buzzelli C, Li X, Harrington AC, et al. Task-specific and general cognitive effects in Chiari malformation Type I. PLoS ONE. 2014;9(4):e94844. https://doi.org/10.1371/journal.pone.0094844
Garcia M, Amayra I, Lázaro E, López-Paz JF, Martínez O, Pérez M, Berrocoso S, Al-Rashaida M. Comparison between decompressed and non-decompressed Chiari Malformation Type I patients: A neuropsychological study. Neuropsychologia. 2018;121:135–143. https://doi.org/10.1016/j.neuropsychologia.2018.11.002
García M, Amayra I, López-Paz JF, Martínez O, Lázaro E, Pérez M, et al. Social cognition in Chiari malformation type I: a preliminary characterization. Cerebellum. 2020;19:392–400.
Hoche F, Guell X, Vangell MG, Sherman JC, Schmahmann JD. The cerebellar cognitive affective/Schmahmann syndrome scale. Brain. 2018;141:248–70.
Allen PA, Delahanty D, Kaut KP, Li X, Garcia M, Houston JR, et al. Chiari 1000 Registry Project: assessment of surgical outcome on self-focused attention, pain, and delayed recall. Psychol Med. 2018;48(10):1634–43. https://doi.org/10.1017/S0033291717003117.
Trapnell PD, Campbell JD. Private self-consciousness and the five-factor model of personality: distinguishing rumination from reflection. J Pers Soc Psychol. 1999;76:284–304.
Leggio M, Olivito G. Topography of the cerebellum in relation to social brain regions and emotions. Handb Clin Neurol. 2018;154:71–84. https://doi.org/10.1016/B978-0-444-63956-1.00005-9.
Overwalle FV, Manto M, Leggio M, Delgado-García JM. The sequencing process generated by the cerebellum crucially contributes to social interactions. Med Hypotheses. 2019;128:33–42.
Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66(1):20–40. https://doi.org/10.1207/s15327752jpa6601_2.
Meeker J, Amerine J, Kropp D, Chyatte M, Fischbein R. The impact of Chiari malformation on daily activities: a report from the national Conquer Chiari Patient Registry database. Disabil Health J. 2015;8(4):521–6. https://doi.org/10.1016/j.dhjo.2015.01.003.
Mueller DM, Oro’ JJ. Prospective analysis of presenting symptoms among 265 patients with radiographie evidence of Chiari malformation type I with or without syringomyelia. J Am Acad Nurse Pract. 2004;16(3):134–8. https://doi.org/10.1111/j.1745-7599.2004.tb00384.x.
Mueller DM, Oro’ JJ. Prospective analysis of self-perceived quality of life before and after posterior fossa decompression in 112 patients with Chiari malformation with or without syringomyelia. Neurosurg Focus. 2005;18(2):ECP2.
Pant H, Bhatki AM, Snyderman CH, Vescan AD, Carrau RL, Gardner P, et al. Quality of life following endonasal skull base surgery. Skull Base. 2010;20(1):35–40. https://doi.org/10.1055/s-0029-1242983.
Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21(1):55–89. https://doi.org/10.1210/edrv.21.1.0389.
Kamali A, Karbasianb N, Rabieia P, Canoa A, Riascosa RF, Tandonc N, et al. Revealing the cerebello-ponto-hypothalamic pathway in the human brain. Neurosci Lett. 2018;677:1–5.
Onat F, Cavdar S. Cerebellar connections: hypothalamus. Cerebellum. 2003;2:263–0.
Burford NG, Webster NA, Cruz-Topete D. Hypothalamic-pituitary-adrenal axis modulation of glucocorticoids in the cardiovascular system. Int J Mol Sci. 2017;18(10). https://doi.org/10.3390/ijms18102150.
Du X, Pang TY. Is dysregulation of the HPA-axis a core pathophysiology mediating co-morbid depression in neurodegenerative diseases? Front Psychiatry. 2015;6. https://doi.org/10.3389/fpsyt.2015.00032.
Adam EK, Kumari M. Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology. 2009;34(10):1423–36. https://doi.org/10.1016/j.psyneuen.2009.06.011.
Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S, et al. Free cortisol levels after awakening: a reliable biological marker for the assessment of adrenocortical activity. Life Sci. 1997;61(26):2539–49. https://doi.org/10.1016/S0024-3205(97)01008-4.
Adam EK, Quinn ME, Tavernier R, McQuillan MT, Dahlke KA, Gilbert KE. Diurnal cortisol slopes and mental and physical health outcomes: a systematic review and meta-analysis. Psychoneuroendocrinology. 2017;83:25–41. https://doi.org/10.1016/j.psyneuen.2017.05.018.
Varghese FP, Brown ES. The hypothalamic-pituitary-adrenal axis in major depressive disorder: a brief primer for primary care physicians. Prim Care Companion J Clin Psychiatry. 2001;3(4):151–5. https://doi.org/10.4088/pcc.v03n0401.
Elenkov IJ. Neurohormonal-cytokine interactions: implications for inflammation, common human diseases and well-being. Neurochem Int. 2008;52(1):40–51. https://doi.org/10.1016/j.neuint.2007.06.037.
Silverman MN, Pearce BD, Biron C, Miller AH. Immune modulation of the hypothalamic-pituitary-adrenal (HPA) axis during viral infection. Viral Immunol. 2005;18(1):41–78. https://doi.org/10.1089/vim.2005.18.41.
Girotti M, Donegan JJ, Morilak DA. Influence of hypothalamic IL-6/gp130 receptor signaling on the HPA axis response to chronic stress. Psychoneuroendocrinology. 2013;38(7):1158–69. https://doi.org/10.1016/j.psyneuen.2012.11.004.
Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci. 2008;31(9):464–8. https://doi.org/10.1016/j.tins.2008.06.006.
Kiecolt-Glaser JK, Glaser R. Depression and immune function: central pathways to morbidity and mortality. J Psychosom Res. 2002;53(4):873–6. https://doi.org/10.1016/S0022-3999(02)00309-4.
Cacioppo JT, Cacioppo S, Capitanio JP, Cole SW. The neuroendocrinology of social isolation. Annu Rev Psychol. 2015a;66:733–67. https://doi.org/10.1146/annurev-psych-010814-015240.
McEwen BS, Alves SE. Estrogen actions in the central nervous system. Endocr Rev. 1999;20(3):279–307. https://doi.org/10.1210/edrv.20.3.0365.
Gillies GE, McArthur S. Estrogen actions in the brain and the basis for differential action in men and women: a case for sex-specific medicines. Pharmacol Rev. 2010;62(2):155–98. https://doi.org/10.1124/pr.109.002071.
Laird KT, Krause B, Funes C, Lavretsky H. Psychobiological factors of resilience and depression in late life. Transl Psychiatry. 2019;9:88. https://doi.org/10.1038/s41398-019-0424-7.
Chai NC, Peterlin BL, Calhoun AH. Migraine and estrogen. Curr Opin Neurol. 2014;27(3):315–24. https://doi.org/10.1097/WCO.0000000000000091.
Rieder JK, Darabos K, Weierich MR. Estradiol and women’s health: considering the role of estradiol as a marker in behavioral medicine. Int J Behav Med. 2020;27:294–304. https://doi.org/10.1007/s12529-019-09820-4.
Straub RH. The complex role of estrogens in inflammation. Endocr Rev. 2007;28(5):521–74. https://doi.org/10.1210/er.2007-0001.
Faith RE, Murgo AJ, Good RA, Plotnikoff NP. Cytokines: Stress and Immunity. Second ed: Florida: CRC Press Taylor & Francis Group Boca Raton; 2006.
Bennett JM, Reeves G, Billman GE, Sturmberg JP. Inflammation–nature’s way to efficiently respond to all types of challenges: implications for understanding and managing “the Epidemic” of chronic diseases. Front Med. 2018;5. https://doi.org/10.3389/fmed.2018.00316.
Salem ML. Estrogen, a double-edged sword: modulation of TH1- and TH2-mediated inflammations by differential regulation of TH1/TH2 cytokine production. Curr Drug Targets Inflamm Allergy. 2004;3(1):97–104. https://doi.org/10.2174/1568010043483944.
Helgason S, Carlström K, Damber M-G, Damber JE, Selstam G, Von Schoultz B. Effects of various oestrogens on circulating androgens and cortisol during replacement therapy in post-menopausal women. Maturitas. 1981;3(3):301–8. https://doi.org/10.1016/0378-5122(81)90038-4.
Serova LI, Harris HA, Maharjan S, Sabban EL. Modulation of several responses to stress by estradiol benzoate and selective estrogen receptor agonists. J Endocrinol. 2010;205(3):253–62. https://doi.org/10.1677/JOE-10-0029.
Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015b;10(2):238–49. https://doi.org/10.1177/1745691615570616.
Clark MS, Bond MJ, Hecker JR. Environmental stress, psychological stress and allostatic load. Psychol Health Med. 2007;12(1):18–30. https://doi.org/10.1080/13548500500429338.
Cole SW, Hawkley LC, Arevalo JMG, Cacioppo JT. Transcript origin analysis identifies antigen-presenting cells as primary targets of socially regulated gene expression in leukocytes. Proc Natl Acad Sci U S A. 2011;108(7):3080–5. https://doi.org/10.1073/pnas.1014218108.
Cole SW, Hawkley LC, Arevalo JM, Sung CY, Rose RM, Cacioppo JT. Social regulation of gene expression in human leukocytes. Genome Biol. 2007;8(9):R189. https://doi.org/10.1186/gb-2007-8-9-r189.
Taylor SE, Burklund LJ, Eisenberger NI, Lehman BJ, Hilmert CJ, Lieberman MD. Neural bases of moderation of cortisol stress responses by psychosocial resources. J Pers Soc Psychol. 2008;95(1):197–211. https://doi.org/10.1037/0022-3514.95.1.197.
Hackett RA, Hamer M, Endrighi R, Brydon L, Steptoe A. Loneliness and stress-related inflammatory and neuroendocrine responses in older men and women. Psychoneuroendocrinology. 2012;37(11):1801–9. https://doi.org/10.1016/j.psyneuen.2012.03.016.
Cole SW. Social regulation of human gene expression: mechanisms and implications for public health. Am J Public Health. 2013;103(Suppl 1):S84–92. https://doi.org/10.2105/AJPH.2012.301183.
Creswell JD, Irwin MR, Burklund LJ, Lieberman MD, Arevalo JMG, Ma J, et al. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav Immun. 2012;26(7):1095–101. https://doi.org/10.1016/j.bbi.2012.07.006.
Holmes S, Gonzalez A, Allen P, Johnson D. Utilizing group acceptance and commitment therapy (ACT) to address chronic pain, coping, and functioning for patients with Chiari malformation: a case example. Prof Psychol Res Pract. 2019;50:296–306. https://doi.org/10.1037/pro0000247.
Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940–52; discussion 2952. https://doi.org/10.1097/00007632-200011150-00017.
Zhang J-M, An J. Cytokines, inflammation and pain. Int Anesthesiol Clin. 2007;45(2):27–37. https://doi.org/10.1097/AIA.0b013e318034194e.
Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–43. https://doi.org/10.1016/0005-7967(94)00075-U.
Dworkin RH, Turk DC, Revicki DA, Harding G, Coyne KS, Peirce-Sandner S, et al. Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2). Pain. 2009;144(1–2):35–42. https://doi.org/10.1016/j.pain.2009.02.007.
Henry JD, Crawford JR .The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–239. https://doi.org/10.1348/014466505X29657
Woo AK. Depression and anxiety in pain. Rev Pain. 2010;4(1):8–12. https://doi.org/10.1177/204946371000400103.
Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manip Physiol Ther. 1991;14(7):409–15.
Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273.
Houston JR, Hughes ML, Bennett IJ, Allen PA, Rogers JM, Lien M-C, et al. Evidence of neural microstructure abnormalities in type I Chiari malformation: associations among fiber tract integrity, pain, and cognitive dysfunction. Pain Med. 2020;21:2323–35. https://doi.org/10.1093/pm/pnaa094.
Acknowledgements
We would like to thank the Conquer Chiari Foundation for financially supporting this work. Furthermore, we would like to thank all the participants for their time and dedication to the research study; without their efforts, none of this research would have been possible.
Funding
This research was funded by a grant from Conquer Chiari.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Garcia, M.A., Li, X., Allen, P.A. et al. Impact of Surgical Status, Loneliness, and Disability on Interleukin 6, C-Reactive Protein, Cortisol, and Estrogen in Females with Symptomatic Type I Chiari Malformation. Cerebellum 20, 872–886 (2021). https://doi.org/10.1007/s12311-021-01251-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-021-01251-w