Abstract
The patient is a woman in her 60s with a history of plasma cell myeloma, status post high-dose melphalan and autologous stem cell transplant, followed by maintenance lenalidomide. She was admitted for severe headaches with concern for meningitis. CSF culture yielded Cryptococcus neoformans. Cryptococcal antigen was present at high titer in the CSF (1:640) but was negative in serum. A diagnosis of cryptococcal meningitis was rendered. She was treated with over 2 weeks of intravenous amphotericin plus flucytosine. Upon discharge, her CSF cryptococcal antigen test remained positive (1:2560) but CSF culture was negative. She continued to experience mild headaches after discharge and was maintained on daily oral fluconazole. Several months later, a bone marrow biopsy was performed to evaluate for residual myeloma post-transplant. There was no morphologic, immunohistochemical, or flow cytometric evidence of residual plasma cell neoplasm. However, the core biopsy revealed suspicious clusters of histiocytes (A) with numerous cytoplasmic inclusions, some of which appeared to contain thick cell wall-like structures (B). Special stains, including periodic acid-Schiff (PAS, C) and Grocott’s methenamine silver (GMS, D), identified variably sized yeast forms, morphologically compatible with Cryptococcus. Infected histiocytes were not visualized on the aspirate smears. A repeat serum cryptococcal antigen test was positive (1:640). She was kept on daily oral fluconazole and is being closely followed by infectious disease. Immunocompromised patients are at increased risk for a variety of marrow infections, including Cryptococcus. Patients with plasma cell myeloma are at risk for invasive fungal infections after autologous stem cell transplant and while taking lenalidomide, which alters CD4 + and CD8 + T-cell function through multiple mechanisms. Due to a lack of standardized treatment protocols for therapy-refractory non-pulmonary non-meningeal cryptococcal disease, therapy regimens are often tailored on a case-by-case basis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The patient is a woman in her 60s with a history of plasma cell myeloma, status post high-dose melphalan and autologous stem cell transplant, followed by maintenance lenalidomide. She was admitted for severe headaches with concern for meningitis. CSF culture yielded Cryptococcus neoformans. Cryptococcal antigen was present at high titer in the CSF (1:640) but was negative in serum. A diagnosis of cryptococcal meningitis was rendered. She was treated with over 2 weeks of intravenous amphotericin plus flucytosine. Upon discharge, her CSF cryptococcal antigen test remained positive (1:2560) but CSF culture was negative. She continued to experience mild headaches after discharge and was maintained on daily oral fluconazole.
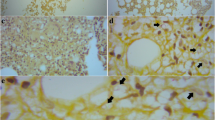
Several months later, a bone marrow biopsy was performed to evaluate for residual myeloma post-transplant. There was no morphologic, immunohistochemical, or flow cytometric evidence of residual plasma cell neoplasm. However, the core biopsy revealed suspicious clusters of histiocytes (A) with numerous cytoplasmic inclusions, some of which appeared to contain thick cell wall-like structures (B). Special stains, including periodic acid-Schiff (PAS, C) and Grocott’s methenamine silver (GMS, D), identified variably sized yeast forms, morphologically compatible with Cryptococcus (Fig. 1). Infected histiocytes were not visualized on the aspirate smears. A repeat serum cryptococcal antigen test was positive (1:640). She was kept on daily oral fluconazole and is being closely followed by infectious disease.
A Hematoxylin and eosin (H&E)-stained section of the marrow core biopsy with clusters of vacuolated histiocytes. 10x magnification. B H&E stain, showing some vacuoles with thickened cell wall-like structures. 40x magnification. C PAS stain, highlighting fungal cell walls. 20x magnification. D GMS stain, highlighting fungal cell walls. 20x magnification
Immunocompromised patients are at increased risk for a variety of marrow infections, including Cryptococcus[1]. Patients with plasma cell myeloma are at risk for invasive fungal infections after autologous stem cell transplant[2] and while taking lenalidomide[3], which alters CD4 + and CD8 + T-cell function through multiple mechanisms[4]. Due to a lack of standardized treatment protocols for therapy-refractory non-pulmonary non-meningeal cryptococcal disease, therapy regimens are often tailored on a case-by-case basis[5].
References
Vechi HT, Theodoro RC, de Oliveira AL, et al. (2019) Invasive fungal infection by Cryptococcus neoformans var. grubii with bone marrow and meningeal involvement in a HIV-infected patient: a case report. BMC Infect Dis. 19(1):220. Published 2019 Mar 4. doi:https://doi.org/10.1186/s12879-019-3831-8
Nematollahi S, Dioverti-Prono V (2020) Cryptococcal infection in haematologic malignancies and haematopoietic stem cell transplantation. Mycoses 63(10):1033–1046. https://doi.org/10.1111/myc.13153
Sato S, Kambe E, Tamai Y (2019) Disseminated cryptococcosis in a patient with multiple myeloma treated with daratumumab, lenalidomide, and dexamethasone. Intern Med 58(6):843–847. https://doi.org/10.2169/internalmedicine.1726-18
Busch A, Zeh D, Janzen V et al (2014) Treatment with lenalidomide induces immunoactivating and counter-regulatory immunosuppressive changes in myeloma patients. Clin Exp Immunol 177(2):439–453. https://doi.org/10.1111/cei.12343
Perfect JR, Dismukes WE, Dromer F et al (2010) Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 50(3):291–322. https://doi.org/10.1086/649858
Acknowledgements
Figure assembly and layout provided by Steve Conlon from Duke’s PhotoPath Laboratory in the Department of Pathology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was granted exemption by the Duke University Health System Institutional Review Board.
Consent to participate/informed consent
This was not deemed necessary by the IRB since no identifiable data is being reported and only histologic images are being presented.
Consent for publication
This was not deemed necessary by the IRB since no identifiable data is being reported and only histologic images are being presented.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Charles, M.G.K., Carlsen, E.D. Marrow cryptococcosis in an autologous stem cell transplant patient after standard therapy for cryptococcal meningitis. J Hematopathol 15, 279–280 (2022). https://doi.org/10.1007/s12308-022-00507-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12308-022-00507-6