Abstract
A dry tap obtained on bone marrow aspiration is considered a failure to aspirate marrow particles. However, it is often related to an underlying bone marrow pathology that hinders successful aspiration of hematopoietic cells. In this retrospective analysis, 2768 bone marrow aspirates and trephine biopsies were reviewed. Of these, 223 patients with bone marrow aspirations which yielded no marrow particles (dry tap) were included in the study. Patients in whom adequate trephine biopsy could not be obtained were excluded from the study. The final diagnosis was made by studying the trephine biopsy and correlating it with other ancillary investigations. Of the 2768 bone marrow aspirations studied, dry tap was seen in 223 (8.0%) patients. Of these, 209 (93.7%) patients had an underlying bone marrow pathology while 14 (6.3%) patients had dry tap due to faulty technique. Hematological malignancies were seen in 164 (73.5%) patients, benign hematological disorders in 33 (14.9%) patients while 4% patients had non-hematological disorders. Among hematological malignancies, leukemia (acute and chronic) was the commonest cause of a dry tap seen in 40.3% of the patients. Dry tap obtained on bone marrow aspiration should serve as a red flag for the hematologist rather than a failed procedure. In most cases, it indicates the possibility of underlying bone marrow pathology. Trephine biopsy should always be studied in such cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone marrow aspiration is a commonly performed procedure and is indicated in many hematological disorders. These include unexplained cytopenia/s, leukemia, staging of lymphoma, pyrexia of unknown origin, aplastic anemia, myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPN), plasma cell dyscrasias, storage disorders, and suspected metastatic cancer [1].
Bone marrow examination includes the study of aspirate smears (squash and/or wedge), trephine biopsy, imprint smears, and clot section [2,3,4,5,6,7,8]. The former is the most often carried out and the latter the least commonly studied modality [9].
Failure to obtain the aspirate on bone marrow aspiration is termed as “dry tap or a blood tap.” It has been reported in 2.7 to 10% of marrow aspirates in different studies. Although faulty technique may also result in a dry tap, on most occasions, dry tap is often related to an underlying bone marrow pathology that hinders successful aspiration of hematopoietic cells [10,11,12,13,14,15,16]. This may occur due to marrow fibrosis, markedly hypercellular marrow, hypocellularity with increased adipose tissue, neoplastic infiltration, or primary bone disorders. In the evaluation of a patient with dry tap during bone marrow aspiration, study of the trephine biopsy is vital in reaching a diagnosis [5, 8, 17, 18].
Materials and methods
This study was carried out in the Department of Pathology of a tertiary care teaching hospital over a period of five and a half years. In this retrospective analysis, 2768 bone marrow aspirates and trephine biopsies were reviewed. Of these, 223 patients with bone marrow aspirations which yielded no marrow particles (dry tap) were included in the study. Patients in whom adequate trephine biopsy could not be obtained were excluded from the study.
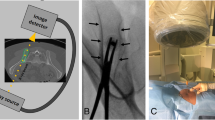
Bone marrow aspiration was done from the posterior superior iliac spine using Jamshidi’s needle. Bone marrow aspiration and biopsy were done by certified physician assistants, junior, senior consultants, and trainee residents under supervision. In all patients in whom dry tap was seen, hemodiluted aspirate smears, touch imprints, clot section, and trephine biopsy were also studied.
The trephine biopsy was fixed in 10% neutral buffered formalin for 24 h followed by overnight decalcification in 10% formic acid. Following standard automated tissue processing protocols, biopsies were embedded in paraffin blocks and 3-μm sections were prepared. Hematoxylin and Eosin (H & E), reticulin, and Periodic Acid Schiff (PAS) stains were done in all cases. In cases where reticulin fibrosis was extensive, Masson’s trichrome stain was done to demonstrate collagen.
Relevant clinical details (presenting symptoms, physical examination findings), complete blood count, touch imprints, and trephine biopsy findings were recorded. Immunohistochemistry was done wherever required. The final diagnosis was made by studying the trephine biopsy and correlating it with other ancillary investigations. Descriptive statistics were used to analyze the data. The study was approved by the institutional research committee.
Results
Of the 2768 bone marrow aspirations studied over the 5½-year period, dry tap was seen in 223 (8.0%) patients. Of the 223 patients, 125 (56.1%) were males and 98 (43.9%) were females (M:F = 1.3:1). The age of the patients ranged from 1 to 85 years with a mean age of 41.9 ± 21.7 years. The most common indication for bone marrow examination was leukemia (acute and chronic) in 99 (44.4%) patients followed by 25 (11.2%) patients with suspected MPN and 20 (8.9%) patients with pancytopenia. The details of clinical indications are shown in Table 1.
Of the 223 patients with dry tap, 209 (93.7%) had an underlying bone marrow pathology while 14 (6.3%) patients had dry tap due to faulty technique. Of the 209 patients, 164 (73.5%) were diagnosed to have hematological malignancies while 33 (14.9%) patients had benign hematological disorders. Other diagnoses made are shown in Fig. 1.
The details of final diagnosis in 223 patients with dry tap included in the study and their comparison with frequency of similar diagnosis in patients who did not have dry tap are shown in Table 2. These included acute leukemia, chronic myeloid leukemia, NHL (Fig. 2), Hairy cell leukemia, and myeloproliferative disorders (Fig. 3), Aplastic anemia, renal osteodystrophy, metastatic deposits, and granulomatous inflammation (Fig. 4).
a Hypercellular marrow with increase in blasts in a 68-year-old male with acute myeloid leukemia. (× 100), (H&E). Inset shows blasts with high N:C ratio, vesicular nuclei, inconspicuous nucleoli, and scanty cytoplasm. b A 6-year-old boy with acute lymphoblastic leukemia showing increase in blasts with coarse to clumped chromatin, inconspicuous nucleoli, and scanty cytoplasm. (× 200), (H&E). c Chronic myeloid leukemia in chronic phase: Markedly hypercellular marrow with myeloid predominance and numerous megakaryocytes. (× 200), (H&E). d Nodular bone marrow involvement in a patient with non-Hodgkin lymphoma. (× 100), (H&E)
a Hairy cell leukemia in a 65-year-old male. The marrow shows infiltration by lymphoid cells with pericellular clearing. A cluster of erythroblasts is seen at the top left. (× 200), (H&E). b Polycythemia vera in a 56-year-old male: Cellular marrow shows panmyelosis. Numerous megakaryocytes are also seen. (× 100), (H&E). c Primary myelofibrosis: Hypocellular marrow shows scattered dysplastic megakaryocytes along with streaming of cells, dilated sinusoids (arrow), and increased fibrosis. (× 100), (H&E). d Reticulin stain in a patient with primary myelofibrosis showing increased fibrosis and a dilated sinusoid (arrow)
a Markedly hypocellular marrow in a 24-year-old woman with severe aplastic anemia. (× 100), (H&E). b Cellular marrow in a 56-year-old male with renal osteodystrophy. Irregular bony trabeculae show resorption bays (Howship’s lacunae) (arrows) and fibrosis (arrow heads) Other areas show erythroid hyperplasia (× 100), (H&E). c Bone marrow shows extensive infiltration by metastatic ductal carcinoma, breast (arrows). Marked desmoplastic reaction is also seen. (× 400), (H&E). d Granuloma seen in the paratrabecular region of the bone marrow
Discussion
Our study has shown that majority of the patients who had a dry tap on bone marrow aspiration showed pathological findings in the trephine biopsy. A dry tap obtained on bone marrow aspiration may be the indication of an underlying hematological or less commonly, non-hematological disorders.
In our study, of the 2768 bone marrows studied, 223 (8%) yielded a dry tap. Similar studies that have selectively assessed patients with dry tap following bone marrow aspiration have reported an incidence of 2.7 to 10% [10,11,12,13,14,15,16].
Just over half (51.1%) of the patients in our study were above 40 years of age. Dry tap was seen more in males as compared to females (M:F = 1.3:1). Similar findings were also observed by Ahmad et al [13]. The most plausible explanation for this difference is the higher prevalence of most hematological and other malignancies in males and older age group.
Of the 223 patients with dry tap in our study, nearly three-fourths (73.5%) had hematological malignancies, 14.9% had benign hematological disorders, 4% had non-hematological disorders, and 6.3% had dry tap due to faulty technique.
Similar to our study, Ahmad et al analyzed 548 bone marrows and reported 52 (9.5%) patients with dry tap. Of these, 73% had hematological malignancies [13]. In a large study of 2235 bone marrows, 87 patients had dry tap on aspiration. Of these, 87.3% had underlying malignancies [10]. Another study including 500 consecutive bone marrows also reported 66.7% of the patients with dry tap to have an underlying malignancy [14]. In contrast, another large study that included 2008 bone marrow examinations reported 37% of the patients with dry tap to have malignant disorders [15].
Among hematological malignancies, leukemia (acute and chronic) was the commonest cause of a dry tap in our study seen in 40.3% patients. In a study of 87 patients who had dry tap, Humphries reported 41.3% of the patients to have leukemia [10]. A similar Fig. (43.1%) was reported in another study of 51 patients [14]. In contrast, Ahmad et al reported acute leukemia as a cause of dry tap in 15.3% patients [13].
In our study, bone marrow fibrosis was seen in 13.7% of the patients with dry tap. These patients had primary myelofibrosis, other myeloproliferative disorders, or secondary fibrosis induced by other pathologies in the marrow (leukemias, lymphoma, myelodysplastic syndrome, and granulomas). A study from UK in 87 patients with dry tap reported 13.8% patients to have marrow fibrosis [10]. A study by Khanum et al showed 13.7% of the patients to have marrow fibrosis [14]. Ahmad et al reported bone marrow fibrosis in 5.8% of patients [13].
In some of the disorders, the cause for bone marrow dry tap could be a combination of factors. In patients with leukemia, lymphoma, multiple myeloma, MDS, and myeloproliferative disorders, extreme marrow cellularity and resultant reactive fibrosis could both contribute to a poor particle yield. Comparison of conditions with dry tap with patients who did not have dry tap did not show a trend that reflected the population frequency of the diseases.
All three patients with miscellaneous disorders (renal osteodystrophy, auto-immune myelofibrosis, and connective tissue disorder) in our study had possible reactive fibrosis related to the primary disorder.
Bone marrow metastasis was seen in 2.7% patients in the present study. Humphries et al reported 17.2% patients to have metastatic bone marrow infiltration [10]. Two other studies on dry tap of bone marrow aspirate reported 15.4% [13] and 9.8% [14] patients with metastatic deposits seen on trephine biopsy.
Benign hematological disorders (aplastic anemia and nutritional anemia) with dry tap consisted of 33 (14.9%) cases in our study. The dry tap in such a setting could be due to marked marrow hypocellularity in the former and packed cellular marrow with erythroid hyperplasia in the latter.
Similar to our study, benign disorders constituted 12.6% of patients with dry tap in a study of 2235 bone marrows [10]. Ahmad et al also reported 11 (21.1%) patients in their study with benign disorders [13]. In developing countries, bone marrow granulomas should always be considered as one of the causes of dry tap. This can occur due to physical space occupied by granulomas as well as secondary reactionary fibrosis. Our study showed three patients with granulomas in the trephine biopsy. A study from Pakistan in 52 patients with dry tap showed 7.7% of patients to have granulomas [13].
Our study showed 14 (6.3%) patients with dry tap due to faulty technique. Although this category can be conjectural in hindsight, the dry tap obtained on aspiration in these patients was not expected based on the clinical profile and complete blood count. The trephine biopsy in all these patients was unremarkable with no pathology that could explain the dry tap. In a few of the cases, on follow-up, repeat aspiration was done which yielded sufficient particles.
Ahmad et al [13] and Humphries [10] in their studies reported faulty technique to the possible cause of dry tap in 7.7% and 6.9% patients respectively. Faulty technique, a much rarer cause of dry tap than is generally believed, maybe a consequence of inexperience of the operator, Ill-fitting stylets, or reused aspiration needles [13].
Dry tap on bone marrow aspirate usually causes alarm due to a failure to obtain diagnostic material from the aspirate smears. However, as is evident from the findings of the present study and also in previous studies, in majority of the cases, dry tap occurs due to underlying specific bone marrow pathology. Contrary to popular belief, faulty technique is the least common cause of dry tap. Rarely, limited material obtained even with failed marrow aspirate may yield diagnostic information [19]. A trephine biopsy should always be undertaken in patients with dry tap so as not to miss an underlying pathology. Clues in the peripheral blood smear like leukoerythroblastic picture or evidence of micro-angiopathic hemolytic anemia may also indicate marrow pathology in such patients [20].
In centers that do not perform a trephine biopsy as a routine practice, it is highly recommended that in all cases of dry tap, a trephine biopsy should be done.
Conclusion
Dry tap obtained on bone marrow aspiration should serve as a red flag for the hematologist and the clinician rather than a failed procedure. In most cases, it indicates the possibility of underlying bone marrow pathology. Trephine biopsy should always be studied in such cases.
Data availability
Yes, original instrument printouts are available for all cases.
Code availability
Not applicable.
References
Bain B (2001) Bone marrow aspiration. J Clin Pathol 54:657–663
Cotelingam JD (2003) Bone marrow biopsy: interpretive guidelines for the surgical pathologist. Adv Anat Pathol 10:8–26
Nanda A, Basu S, Marwaha N (2002) Bone marrow trephine biopsy as an adjunct to bone marrow aspiration. J Assoc Physicians India 50:893–895
Lee SH, Erber WN, Porwit A, Tomonaga M, Peterson LC, International Council for Standardization in Hematology (2008) ICSH guidelines for the standardization of bone marrow specimens and reports. Int J Lab Hematol. 30:349–364
Chandra S, Chandra H, Saini S (2010) Bone marrow metastasis by solid tumors – probable hematological indicators and comparison of bone marrow aspirate, touch imprint and trephine biopsy. Hematology 15:368–372
Khan TA, Khan IA, Mahmood K (2014) Diagnostic role of bone marrow aspiration and trephine biopsy in haematological practice. J Postgrad Med Inst 28:217–221
Parajuli S, Tuladhar A (2014) Correlation of bone marrow aspiration and biopsy findings in diagnosing hematological disorders – a study of 89 cases. J Pathol Nepal 4:534–538
Riley RS, Hogan TF, Pavot DR et al (2004) A pathologist’s perspective on bone marrow aspiration and biopsy: I. Performing a bone marrow examination. J Clin Lab Anal 18:70–90
Cantadori LO, Gaiolla RD, Niero-Melo L, Oliveira CC (2019) Bone marrow aspirate clot: a useful technique in diagnosis and follow-up of hematological disorders. Case Rep Hematol 2019:7590948
Humphries JE (1990) Dry tap bone marrow aspiration: clinical significance. Am J Hematol 35:247–250
Navone R, Colombano MT (1984) Histopathological trephine biopsy findings in cases of ‘dry tap’ bone marrow aspirations. Appl Pathol 2:264–271
Reid MM (1991) Dry tap marrow aspiration. Am J Hematol 37:218–219
Ahmad SQ, Yusuf R, Zafar N, Ali N (2015) Dry tap: a diagnostic alert for underlying bone marrow pathology. J Ayub Med Coll Abbottabad 27:120–123
Khanum F, Rehman A, Ahmad S, Anwar J (2009) Dry tap of bone marrow and its clinical importance. PJMHS 3:292–294
Awaad MH (2018) A review of bone marrow examinations in Ibn Sena Teaching Hospital in Mosul. Ann Coll Med Mosul 40:69–73
Mukiibi JM, Paul B, Gordeuk VR (1989) The significance of ‘dry tap’ bone marrow aspirations in Zimbabweans. East Afr Med J 66:481–484
Bain B (2001) Bone marrow trephine biopsy. J Clin Pathol 54:737–742
Sitalakshmi S, Srikrishna A, Devi S, Damodar P, Alexander B (2005) The diagnostic utility of bone marrow trephine biopsies. Indian J Pathol Microbiol 48:173–176
Islam A (2018) Diagnostic value of preparing bone marrow smears from the small amount of material left within the aspiration needle following a dry tap. Clin Case Rep 6:2427–2430
Lin YC, Chang HK, Sun CF, Shih LY (1995) Microangiopathic hemolytic anemia as an initial presentation of metastatic cancer of unknown primary origin. South Med J 88:683–687
Acknowledgements
The study was conducted at the Christian Medical College & Hospital, Ludhiana, Punjab, India.
Author information
Authors and Affiliations
Contributions
SD collected the data and took the microphotographs. SD and NK reviewed the literature, analyzed the data, and drafted the manuscript. NK edited the microphotographs. All authors have read and approved the final submission.
Corresponding author
Ethics declarations
Ethics approval
This study has been approved by the institutional research committee and by the Dean (Principal) of the Christian Medical College & Hospital, Ludhiana, Punjab, India, where it was conducted.
Consent to participate
Since this was a study based on a review of retrospective data, consent was not obtained. Individual consent was taken for the bone marrow procedure.
Consent for publication
Patient consent is not required as this was a retrospective analysis and no patient identifying information has been used. Consent for publishing the research has been obtained by from the institutional research committee.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
ESM 1
(XLSX 211 kb)
Rights and permissions
About this article
Cite this article
Donald, S., Kakkar, N. Dry tap on bone marrow aspiration: a red flag. J Hematopathol 14, 125–130 (2021). https://doi.org/10.1007/s12308-021-00450-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12308-021-00450-y