Abstract
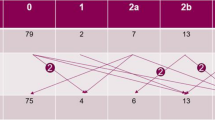
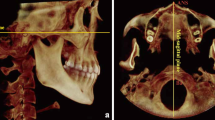
The purpose of this study was to investigate the long-term effects of chemoradiotherapy and transplantation on the temporomandibular joint (TMJ) and dental status in leukemia and stem cell transplantation (SCT) patients. The study included 44 patients and 22 controls. Participants were categorized into three groups: patients with leukemia in Group-1 (n = 22), patients with SCT in Group-2 (n = 22), and controls in Group-3 (n = 22). All patients were evaluated using the Diagnostic Criteria for TMJ Disorders (TMD), as well as clinical and radiographic assessments. TMD was found in 19 (86%) of the 22 patients in Group-1, 12 (54%) of the 22 patients in Group-2, and 4 (18%) of the 22 controls. The brushing habit was significantly lower in Group-2 than in other Groups (p < 0.05). Group-3 had significantly higher mean values for painless, maximum assisted, and unassisted mouth opening than the other Groups (p < 0.05). The rate of click and crepitation sounds was significantly higher in Group-1 and Group-2 than in Group-3 (p < 0.05). The rate of nondental pain was significantly higher in Group-1 than in other Groups (p < 0.05). The rate of disc displacement with a reduction in both TMJ was significantly higher in Group-1 than in Group-3 (p < 0.05). Radiological studies revealed flattening in at least one condyle in 9 (20%) of both Group-1 and Group-2 patients. Flattening of both condyles and thinning of the mandibular cortex due to osteoporosis were found in 2 (9%) of Group-2. Our data suggest that screening for TMD after chemoradiotherapy and SCT may be beneficial for pediatric leukemia.

Similar content being viewed by others
References
Jovičić O, Mandić J, Mandinić Z, Čolović A (2021) Oral changes in patients before and after transplantation of solid organs and hematopoietic stem cells. Srp Arh Celok Lek 149(5–6):381–386
Çetiner D, Çetiner S, Uraz A, Alpaslan GH, Alpaslan C, Toygar Memikoğlu TU et al (2019) Oral and dental alterations and growth disruption following chemotherapy in long-term survivors of childhood malignancies. Support Care Cancer 27:1891–1899
Frascino AV, Coracin FL, da Silva Santos PS, Júnior LAV, Fava M, OdoneFilho V (2015) Long-term dental follow-up in hematological stem cells transplantation children. Braz Dent Sci 18(4):12–8
American Academy of Pediatric Dentistry (2016) Guideline on dental management of pediatric patients receiving chemotherapy, hematopoietic cell transplantation, and/or radiation therapy. Pediatr Dent 38(6):334–342.5
Glenny A, Gibson F, Auld E, Coulson S, Clarkson J, Craig J et al (2010) The development of evidence-based guidelines on mouth care for children, teenagers and young adults treated for cancer. Eur J Cancer 46(8):1399–1412
Sung L, Robinson P, Treister N, Baggott T, Gibson P, Tissing W, Wiernikowski J, Brinklow J, Dupuis LL (2017) Guideline for the prevention of oral and oropharyngeal mucositis in children receiving treatment for cancer or undergoing hematopoietic stem cell transplantation. BMJ Support Palliat Care 7(1):7–16
Uderzo C, Fraschini D, Balduzzi A, Galimberti S, Arrigo C, Biagi E et al (1997) Long-term effects of bone marrow transplantation on dental status in children with leukemia. Bone Marrow Transplant 20(10):865–869
Welbury R, Craft A, Murray J, Kernahan J (1984) Dental health of survivors of malignant disease. Arch Dis Child 59(12):1186–1187
Dahllöf G, Krekmanova L, Kopp S, Borgström B, Forsberg C-M, Ringdén O (1994) Craniomandibular dysfunction in children treated with total-body irradiation and bone marrow transplantation. Acta Odontol Scand 52(2):99–105
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet J-P et al (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 28(1):6
Girard P, Auquier P, Barlogis V, Contet A, Poiree M, Demeocq F et al (2013) Symptomatic osteonecrosis in childhood leukemia survivors: prevalence, risk factors and impact on quality of life in adulthood. Haematologica 98(7):1089
Kim SY, Yoo DM, Kwon MJ, Kim JH, Kim J-H, Byun S-H et al (2022) Increased risk of temporomandibular joint disorder in osteoporosis patients: a longitudinal study. Front Endocrinol (Lausanne) 13:835923
Kaya Z, Gursel T, Bakkaloglu SA, Kocak U, Atasever T, Oktar SO (2007) Evaluation of renal function in Turkish children receiving BFM-95 therapy for acute lymphoblastic leukemia. Pediatr Hematol Oncol 24(4):257–267
Gibson BE, Wheatley K, Hann I, Stevens R, Webb D, Hills RK et al (2005) Treatment strategy and long-term results in paediatric patients treated in consecutive UK AML trials. Leukemia 19(12):2130–2138
Organization WHO (2013) Oral health surveys: basic methods: World Health Organization, 5th edition, pp 125
Gawade PL, Hudson MM, Kaste SC, Neglia JP, Constine LS, Robison LL et al (2014) A systematic review of dental late effects in survivors of childhood cancer. Pediatr Blood Cancer 61(3):407–416
Effinger KE, Migliorati CA, Hudson MM, McMullen KP, Kaste SC, Ruble K et al (2014) Oral and dental late effects in survivors of childhood cancer: a Children’s Oncology Group report. Support Care Cancer 22(7):2009–2019
Halperson E, Matalon V, Goldstein G, Saieg Spilberg S, Herzog K, Fux-Noy A et al (2022) The prevalence of dental developmental anomalies among childhood cancer survivors according to types of anticancer treatment. Sci Rep 12(1):1–8
da Silva CG, Pacheco-Pereira C, Porporatti AL, Savi MG, Peres MA, Flores-Mir C et al (2016) Prevalence of clinical signs of intra-articular temporomandibular disorders in children and adolescents: a systematic review and meta-analysis. J Am Dent Assoc 147(1):10–8.e8
Al-Khotani A, Naimi-Akbar A, Albadawi E, Ernberg M, Hedenberg-Magnusson B, Christidis N (2016) Prevalence of diagnosed temporomandibular disorders among Saudi Arabian children and adolescents. J Headache Pain 17(1):1–11
Goodman J, McGrath P (1991) The epidemiology of pain in children and adolescents: a review. Pain 46(3):247–264
Alajbeg IZ, Gikić M, Valentić-Peruzović M (2015) Mandibular range of movement and pain intensity in patients with anterior disc displacement without reduction. Acta Stomatol Croat 49(2):119
Nilsson I-M, List T, Drangsholt M (2005) Prevalence of temporomandibular pain and subsequent dental treatment in Swedish adolescents. J Orofac Pain 19(2):144–150
Poluha RL, Canales GDlT, Costa YM, Grossmann E, Bonjardim LR, Conti PCR (2019) Temporomandibular joint disc displacement with reduction: a review of mechanisms and clinical presentation. J Appl Oral Sci 27:e20180433
Pasinato F, Souza JA, Corrêa ECR, da Silva AMT (2011) Temporomandibular disorder and generalized joint hypermobility: application of diagnostic criteria. Braz J Otorhinolaryngol 77(4):418–425
Dias IM, Coelho PR, Assis NMSP, Leite FPP, Devito KL (2012) Evaluation of the correlation between disc displacements and degenerative bone changes of the temporomandibular joint by means of magnetic resonance images. Int J Oral Maxillofac Surg 41(9):1051–1057
Powell C, Chang C, Naguwa SM, Cheema G, Gershwin ME (2010) Steroid induced osteonecrosis: An analysis of steroid dosing risk. Autoimmun Rev 9(11):721–743
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Z.K, S.K, and Ü.K. recruited patients. Material preparation, data collection and analysis were performed by Z.K, Ö.Ö.G, Z.A, and D.Ç. The first draft of the manuscript was written by Z.K, D.Ç, and Ö.Ö.G. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study is by recognized standards of ethics as Declaration of Helsinki and approval was granted by the Ethics Committee of the Gazi University Faculty of Dentistry Turkey (Date: 11.03.2022 /No: E.311745). Written informed consent was obtained from all individual participants included in the study.
Conflicts of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gündoğdu, Ö.Ö., Cankal, D.A., Kaya, Z. et al. Temporomandibular Joint and Dental Complications in Long-Term Survivors of Children with Leukemia after Chemoradiotherapy and Stem Cell Transplantation. Indian J Hematol Blood Transfus (2024). https://doi.org/10.1007/s12288-024-01786-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12288-024-01786-y