Abstract
Objective
The application of immediate breast reconstruction (IBR) for post-neoadjuvant therapy (NAT) patients was controversial. The aim of this study was to investigate the long-term survival outcomes of IBR for these patients.
Methods
Data between January 2010 and November 2017 were extracted from the Surveillance, Epidemiology, and End Results (SEER) database. Propensity score matching (PSM) was performed to reduce the influence of confounding factors between the mastectomy alone group (MA) and the mastectomy with IBR group (IBR). The rates of 5 year breast cancer-specific survival (BCSS) were compared by Kaplan–Meier curves with log-rank test.
Results
The IBR was associated with improved 5-year BCSS in the IBR group before PSM (88.5 vs. 79.1%, P < 0.001). The proportion of IBR increased from 21.5% in 2010 to 28.2% in 2017. After PSM, a total of 9,610 patients were enrolled for survival analysis (4,805 in each group). In the complete response (CR) group, the 5-year BCSS rates did not differ (93.4 vs. 95.6%, P = 0.16). In the non-CR group, the 5-year BCSS rate was higher in patients who received IBR (82.5% 79.4%, P = 0.034).
Conclusion
In general, the application of IBR among post-NAT patients has steadily increased from 2010 to 2017. In the CR group, survival outcomes of post-NAT patients who received IBR were similar to those who received mastectomy alone. In the non-CR group, IBR was associated with potential survival benefits. More studies are expected to validate our findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant therapy (NAT) plays a vital role in the treatment of breast cancer, which includes neoadjuvant chemotherapy (NACT), neoadjuvant radiotherapy (NART), endocrine therapy and targeted therapy. NACT was originally recommended to treat locally advanced breast cancer, because of the effectiveness of downstaging tumors to facilitate surgery, as well as facilitating breast conservation in such cases [1, 2]. To date, the indications of NACT have gradually expanded to triple-negative, human epidermal growth factor receptor 2 positive (HER2 +), or early-stage breast cancer [3, 4]. Meanwhile, during the treatment, NART was typically used in conjunction with NACT to treat initial inoperable breast cancer [5]. Furthermore, drug sensitivity of breast cancer patients could be studied during the treatment to guide subsequent therapy to improve outcomes.
Mastectomy followed by immediate breast reconstruction (IBR), involving autologous flap reconstruction and implant-based reconstruction, has gained popularity among patients. In comparison to delayed breast reconstruction, IBR offers better cosmetic outcomes, more positive psychological impact, and only one operation with less financial burden [6,7,8]. However, the issue of IBR for post-NAT patients was controversial, with different conclusions being reached by different studies. Gouy et al. confirmed that IBR after NACT did not significantly affect the local relapse-free or distant disease-free survival [9]. Wu et al. also demonstrated the comparable long-term oncologic outcomes of IBR with nipple-sparing or skin-sparing mastectomy to conventional mastectomy alone [10]. However, according to a previous study which was based on data from the Korean Breast Cancer Society, IBR following mastectomy was associated with worse prognoses than mastectomy alone in non-pCR patients with advanced clinical stages of cancer [11]. Meanwhile, a number of studies were concerned that NACT may increase local recurrence risk after breast-conserving surgery (BCS) [12, 13]. In addition, discrepancies in complication rates across studies hindered decision-making about whether to receive IBR in the setting of NAT [14,15,16].
In view of the personal preference of patients to breast reconstruction, it is difficult to conduct a randomized controlled trial to investigate IBR’s outcomes. Meanwhile, prior studies, mainly retrospective single-center studies, provided insufficient evidence. Consequently, we used the SEER database to perform this large population-based research that investigate the long-term prognosis of post-NAT patients who underwent IBR.
Materials and methods
Population
Approximately 28% of the national population was included in SEER, which collected data from 18 cancer registries across the United States. Using the SEER*Stat 8.4.0.1, 20–80 years old women who were diagnosed with primary M0 stage breast cancer and received neoadjuvant therapy between January 2010 and November 2017 were initially identified. Exclusion criteria included: (1) more than one malignant tumor; (2) T0 or Tis stage; (3) bilateral breast cancer; (4) not receive surgery or with unknown surgical information. Finally, all the eligible patients were divided into breast-conserving group (BCS, surgery codes 19–24), mastectomy alone group (MA, surgery codes 40–42, 50–52, 60–62, 70–72) and mastectomy with IBR group (IBR, surgery codes 30, 43–49, 53–59, 63–69, 73–75).
Variables and definitions
An unmarried status was defined as divorced, separated, single, domestic partner, or widowed at the time of diagnosis. Grade 1–4 were defined as well, moderately, poorly and undifferentiated in ICD-O-2, respectively. Histologic type included infiltrating duct carcinoma (IDC, ICD-O-3 code 8500), infiltrating lobular carcinoma (ILC, ICD-O-3 code 8520), infiltrating duct and lobular carcinoma (ICD-O-3 code 8500) and others. Contralateral breast mastectomy (CPM) and reconstruction type were based on surgery codes. The order of radiotherapy and systemic therapy was preoperative, intraoperative, postoperative or perioperative. Both therapies were reduced to given and not given for analysis. According to the SEER Program Coding and Staging Manual 2022 [17], response to neoadjuvant therapy (RNT) was recorded based on the surgical pathology report. Complete pathological response (CR) denoted the absence of the primary tumor. A partial response (PR) was defined as a decrease in tumor size/extent and evidence of tumor regression. No definite response (NR) referred to a tumor's size or extent showing no change at all or showing considerable remaining invasive malignancy. Unknown response indicated that NAT was completed but there was no documented treatment response in the surgical pathology report. Non-CR in this work included PR and NR. The cutoff date for this research was November 2017. The time from diagnosis to death related to breast cancer was the definition of BCSS.
Propensity score matching
Propensity score matching (PSM) was carried out in a 1:1 ratio in the comparison between the MA group and the IBR group using the R package "MatchIt", with the parameters of the "nearest" method and a caliper of 0.02. This was done to lessen the impact of confounding factors on prognosis. Age, year of diagnosis, race, marital status at diagnosis, grade, histology, T stage, N stage, CPM, RNT, radiation, systemic therapy, estrogen receptor (ER) status, progesterone receptor (PR) status, HER2 status, and median household income were the baseline characteristics used for matching.
Statistical analysis
All analyses were performed using R software (version 4.2.1; http://www.r-project.org/). To compare normally distributed data that were expressed as mean ± standard deviation (x ± s), Student's t-test was utilized. Non-normally distributed data that were reported as median (interquartile range, IQR) were analyzed using the Mann–Whitney U test. Categorical data was presented as n (%) and was then examined using the Chi-square test or the Fisher's exact test. Kaplan–Meier method with log-rank test was used to assess 5 year BCSS. The statistical significance levels were both two-sided and set at P < 0.05.
Results
We obtained information on 31,054 female patients aged 20 to 80 who had M0 stage breast cancer and had undergone NAT between 2010 and 2017. In Fig. 1, the screening flow is displayed. A total of 24,537 eligible patients were eventually enrolled, of whom 9,017 underwent breast-conserving surgery, 9,064 had a mastectomy alone and 6,456 underwent mastectomy with IBR. The MA group and the IBR group were further compared.
Demographic features
Trends in the application of the three treatments are shown in Fig. 2. Generally, the proportion of post-NAT patients who underwent either breast-conserving surgery (28.8 to 41.5%) or mastectomy with IBR (21.5 to 28.2%) was increasing from 2010 to 2017, and the proportion of mastectomy alone was declining (49.7 to 30.3%). Table 1 reports the comparison of the MA group and the IBR group. Mastectomy with IBR was associated with younger, white or married patients (P < 0.001, respectively). In addition, patients in both groups mostly earned between $50,000 and $70,000, while the patients with income higher than $70,000 were more in the IBR group (P < 0.001).
Clinical and pathological characteristics
With the exception of laterality, every clinical and pathological characteristic between groups was statistically significant (Table 1). Grade III/IV (55.5% in the MA group and 56.8% in the IBR group) and IDC (79.3% in the MA group and 83.3% in the IBR group) made up the majority in each group. The IBR group related to more patients with T1-2 and N0 stage breast cancer, but fewer patients with T3-4 and N1-3 stage breast cancer. In the IBR group, CR was more prevalent (32.0 vs. 25.2%), whereas in the MA group, NR was more prevalent (10.4 vs. 7.2%, P < 0.001). The most prevalent breast subtype was HR + /HER2- (40.8% in the MA group and 37.8% in the IBR group), whereas HR-/HER2 + was the least common (12.5% in the MA group and 11.1% in the IBR group).
Therapeutic characteristics
In the IBR group compared to the MA group, CPM was more prevalent (55.2% vs. 31.6%, P < 0.001). In the IBR group, implant-based reconstruction (34.2%) was the most common. In the both groups, systemic therapy was given to the vast majority of the patients. However, radiation was given to more patients in the MA group (60.7 vs. 49.7%, P < 0.001).
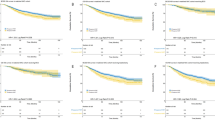
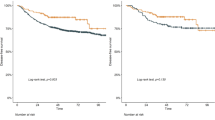
Comparison of survival outcomes
The IBR group had a significantly higher 5-year BCSS rate prior to PSM (88.5 vs. 79.1%, P < 0.001) (Fig. 3). After PSM, a total of 9,610 individuals were enrolled for further survival analysis (Table 1). Kaplan–Meier curves with log-rank tests revealed a significant between-group difference in the 5 year BCSS rate (87.3 vs. 84.7%, P = 0.004) (Fig. 4). According to subgroup analysis, the 5 year BCSS rate was higher in the IBR group of the non-CR group (82.5 vs. 79.4%, P = 0.034) (Fig. 5), but did not differ in the CR or the unknown-response groups. There were no statistically significant between-group differences across the various stages after further stratification by the AJCC stage.
Breast cancer-specific survival rates of the MA versus IBR groups after propensity score matching. A All the patients; B The CR group; C The non-CR group; D The unknown-response group. BCSS breast cancer-specific survival, CR complete response, MA mastectomy alone, IBR immediate breast reconstruction
Discussion
To our knowledge, the current work was the first SEER database-based research on the application of IBR for post-NAT patients. Our study showed a steady increase in IBR for post-NAT patients over the past few years. Meanwhile, IBR was proper and worthy of consideration for post-NAT patients, which might improve the 5-year BCSS.
Several reasons gave rise to the increase of IBR in the setting of NAT. On the one hand, the use of NAC has gradually increased since 2010, of which the aim gradually expanded from breast conservation to personalized treatment [18, 19]. The population base of our study kept growing for this reason. On the other hand, the Women's Health and Cancer Rights Act, which was passed in the US in 1998, mandated comprehensive coverage for breast reconstruction following mastectomy. An earlier study showed that the percentage of women getting breast reconstruction increased steadily over time [20]. Furthermore, several studies investigated the application of breast reconstruction in patients who were traditionally considered at high risk, and had achieved acceptable outcomes, which further improved the increase of IBR [21,22,23].
Before-PSM comparison showed IBR following NAT was associated with younger age, married status, earlier tumor stage and higher income, which were consistent with previous researches [11, 24, 25]. Analysis of prognosis showed the IBR was associated with improved BCSS. However, this beneficial association should be cautious, although several small-sample, single-center studies had demonstrated the feasibility and safety of IBR following NAT [9, 10, 26]. IBR lowered breast cancer-specific mortality in a prior sizable population-based trial, according to Bezuhly M et al. However, they also observed that these results were due to imbalances in socioeconomic factors and access to care rather than insufficient adjustment for tumor features and disease severity [27]. When the confounding effect of family income was taken into account, another study showed that immediate postmastectomy reconstruction had little benefits for survival [28]. In contrast, the previous Korean nationwide study confirmed that IBR following mastectomy was associated with worse prognoses than mastectomy alone among patients with advanced clinical stage tumor of the non-pCR group [11].
Although PSM was performed in this present work, some confounding factors were still unbalanced due to their unavailability in the SEER database such as baseline health status. Patients at a poor health status such as obesity, cardiovascular disease, and smoking history might not consider the IBR, but were associated with worse prognosis. We believe this potential imbalance caused the improved 5-year BCSS in the non-CR group. Additionally, the impact of IBR on personal life quality and psychology should also be considered. A previous meta-analysis demonstrated a better health-related quality of life (HRQOL) outcomes of breast reconstruction [29]. Another study revealed that reconstruction following a mastectomy significantly affects body image and sexual function [30]. Furthermore, a recent study demonstrated that poor HRQOL might increase the mortality risk [31]. Some patients with inoperable breast cancer in our study received NAT for breast conservation or reconstruction purpose, but might failed because of the severity of the disease (non-CR), which caused anxiety and depression. This potential psychological fluctuation during the treatment was a probable adverse factor, which led to a worse HRQOL with worse prognosis. However, in the absence of relevant data in the SEER database, we were unable to investigate the impact of personal life quality and psychology. Further researches to estimate HRQOL of the patients who received breast reconstruction after NAT are required.
There are several limitations in the use of the SEER database. Firstly, selection bias was inevitable in this retrospective study. Secondly, due to the lack of data on local recurrence, adequate evaluation of the oncology outcome is limited. Meanwhile, we are unable to access the perioperative complications among different treatments because of the unavailable data. Finally, this work was only based on population in the United States, and more real-word studies in other countries or regions are expected. Nonetheless, our retrospective work is able to provide some valuable reference in the absence of randomized controlled trials.
Conclusion
The application of IBR in post-NAT patients has steadily increased. In the CR group, survival outcomes of post-NAT patients who received IBR were similar to those who received mastectomy alone. In the non-CR group, IBR was associated with potential survival benefits. More studies are expected to validate our findings.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Heil J, Kuerer HM, Pfob A, Rauch G, Sinn HP, Golatta M, et al. Eliminating the breast cancer surgery paradigm after neoadjuvant systemic therapy: current evidence and future challenges. Ann Oncol. 2020;31:61–71.
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from national surgical adjuvant breast and bowel project B-18. J Natl Cancer Inst Monogr. 2001;2001:96–102.
Smith IE, Lipton L. Preoperative/neoadjuvant medical therapy for early breast cancer. Lancet Oncol. 2001;2:561–70.
Mieog JS, van der Hage JA, van de Velde CJ. Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev. 2007;2007:005002.
Singh P, Hoffman K, Schaverien MV, Krause KJ, Butler C, Smith BD, et al. Neoadjuvant radiotherapy to facilitate immediate breast reconstruction: a systematic review and current clinical trials. Ann Surg Oncol. 2019;26:3312–20.
Cordeiro PG. Breast reconstruction after surgery for breast cancer. N Engl J Med. 2008;359:1590–601.
Chen W, Lv X, Xu X, Gao X, Wang B. Meta-analysis for psychological impact of breast reconstruction in patients with breast cancer. Breast Cancer. 2018;25:464–9.
Retrouvey H, Kerrebijn I, Metcalfe KA, O’Neill AC, McCready DR, Hofer SOP, et al. Psychosocial functioning in women with early breast cancer treated with breast surgery with or without immediate breast reconstruction. Ann Surg Oncol. 2019;26:2444–51.
Gouy S, Rouzier R, Missana MC, Atallah D, Youssef O, Barreau-Pouhaer L. Immediate reconstruction after neoadjuvant chemotherapy: effect on adjuvant treatment starting and survival. Ann Surg Oncol. 2005;12:161–6.
Wu ZY, Kim HJ, Lee JW, Chung IY, Kim JS, Lee SB, et al. Long-term oncologic outcomes of immediate breast reconstruction vs conventional mastectomy alone for breast cancer in the setting of neoadjuvant chemotherapy. JAMA Surg. 2020;155:1142–50.
Park S, Jeong J, Han W, Lee YJ, Kim HA, Lee S, et al. Is mastectomy with immediate reconstruction safe for patients undergoing neoadjuvant chemotherapy? A nationwide study from Korean Breast Cancer Society. Breast Cancer. 2021;28:874–83.
Early Breast Cancer Trialists Collaborative. Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol. 2018;19:27–39.
Wong SM, Chun YS, Sagara Y, Golshan M, Erdmann-Sager J. National patterns of breast reconstruction and nipple-sparing mastectomy for breast cancer, 2005–2015. Ann Surg Oncol. 2019;26:3194–203.
Abt NB, Flores JM, Baltodano PA, Sarhane KA, Abreu FM, Cooney CM, et al. Neoadjuvant chemotherapy and short-term morbidity in patients undergoing mastectomy with and without breast reconstruction. JAMA Surg. 2014;149:1068–76.
Narui K, Ishikawa T, Satake T, Adachi S, Yamada A, Shimada K, et al. Outcomes of immediate perforator flap reconstruction after skin-sparing mastectomy following neoadjuvant chemotherapy. Eur J Surg Oncol. 2015;41:94–9.
Beugels J, Bod L, van Kuijk SMJ, Qiu SS, Tuinder SMH, Heuts EM, et al. Complications following immediate compared to delayed deep inferior epigastric artery perforator flap breast reconstructions. Breast Cancer Res Treat. 2018;169:349–57.
SEER Program Coding and Staging Manual 2022. Available at: https://seer.cancer.gov/archive/manuals/2022/AppendixC/Treatment_Effect_Codes_Breast_2022.pdf
An J, Peng C, Tang H, Liu X, Peng F. New advances in the research of resistance to neoadjuvant chemotherapy in breast cancer. Int J Mol Sci. 1944;2021:22.
Murphy BL, Day CN, Hoskin TL, Habermann EB, Boughey JC. Neoadjuvant chemotherapy use in breast cancer is greatest in excellent responders: triple-negative and HER2+ subtypes. Ann Surg Oncol. 2018;25:2241–8.
Nayyar A, Reddy KG, Strassle PD, Moses CG, Roughton MC, Gallagher KK, et al. Temporal trends in immediate post-mastectomy breast reconstruction. J Plast Reconstr Aesthet Surg. 2019;72:513–27.
Agarwal S, Kidwell KM, Farberg A, Kozlow JH, Chung KC, Momoh AO. Immediate reconstruction of the radiated breast: recent trends contrary to traditional standards. Ann Surg Oncol. 2015;22:2551–9.
Sada A, Day CN, Hoskin TL, Degnim AC, Habermann EB, Hieken TJ. Mastectomy and immediate breast reconstruction in the elderly: Trends and outcomes. Surgery. 2019;166:709–14.
Nair AG, Giannakeas V, Semple JL, Narod SA, Lim DW. Contemporary trends in breast reconstruction use and impact on survival among women with inflammatory breast cancer. Ann Surg Oncol. 2022;29:8702.
Ishiba T, Aruga T, Miyamoto H, Ishihara S, Nara M, Adachi M, et al. Short-and long-term outcomes of immediate breast reconstruction surgery after neoadjuvant chemotherapy. Surg Today. 2022;52:129–36.
Fu M, Chen Q, Zeng L, Hong T, Zou Q, Yuan Y, et al. Prognosis comparison between nipple-sparing mastectomy and total mastectomy in breast cancer: a case-control study after propensity score matching. Ann Surg Oncol. 2022;29:2221–30.
Pazos M, Corradini S, Dian D, von Bodungen V, Ditsch N, Wuerstlein R, et al. Neoadjuvant radiotherapy followed by mastectomy and immediate breast reconstruction : An alternative treatment option for locally advanced breast cancer. Strahlenther Onkol. 2017;193:324–31.
Bezuhly M, Temple C, Sigurdson LJ, Davis RB, Flowerdew G, Cook EF Jr. Immediate postmastectomy reconstruction is associated with improved breast cancer-specific survival: evidence and new challenges from the Surveillance, Epidemiology, and End Results database. Cancer. 2009;115:4648–54.
Jiang YZ, Liu YR, Yu KD, Zuo WJ, Shao ZM. Immediate postmastectomy breast reconstruction showed limited advantage in patient survival after stratifying by family income. PLoS ONE. 2013;8:e82807.
Zehra S, Doyle F, Barry M, Walsh S, Kell MR. Health-related quality of life following breast reconstruction compared to total mastectomy and breast-conserving surgery among breast cancer survivors: a systematic review and meta-analysis. Breast Cancer. 2020;27:534–66.
Fortunato L, Loreti A, Cortese G, Spallone D, Toto V, Cavaliere F, et al. Regret and quality of life after mastectomy with or without reconstruction. Clin Breast Cancer. 2021;21:162–9.
Park J, Rodriguez JL, O’Brien KM, Nichols HB, Hodgson ME, Weinberg CR, et al. Health-related quality of life outcomes among breast cancer survivors. Cancer. 2021;127:1114–25.
Acknowledgements
The National Science and Technology Foundation Project (No. 2019-JCJQ-JQ-069) and the National Natural Science Foundation of China (No. 81672927) provided funding for this work.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors affirm that they have no known financial or interpersonal conflicts that would have appeared to have an impact on the present study.
Ethical approval
All data in this work were obtained from the SEER database. Thus, the ethical approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Pan, J., Peng, L., Tong, X. et al. Prognosis of post-neoadjuvant therapy patients who underwent immediate breast reconstruction: a SEER-based, propensity-matched study. Breast Cancer 30, 986–996 (2023). https://doi.org/10.1007/s12282-023-01489-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-023-01489-8