Abstract
Background
Persistent post-surgical pain (PPSP) is associated with upper limb dysfunction and decreased quality of life and causes long-term suffering for breast cancer survivors after surgery. However, the predictors of PPSP remain unclear. The purpose of this study was to examine predictors of PPSP intensity and interference at 1 year postoperatively, focusing on treatment-related factors, pre- and postoperative central sensitization (CS), CS-related symptoms (e.g., muscle stiffness, fatigue, sleep disturbances), and psychological factors.
Methods
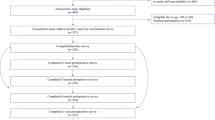
Eighty-eight women with planned unilateral breast cancer surgery were included in this longitudinal study. CS, CS-related symptoms, and psychological factors were assessed preoperatively, 1 month postoperatively, and 1 year postoperatively. Analysis of covariance was used to compare the groups with and without PPSP, accounting for treatment-related factors. Multiple regression analysis was performed to identify predictors of PPSP intensity and interference at 1 year postoperatively.
Results
Even after adjusting for covariates, preoperative and 1-month postoperative Central Sensitization Inventory scores in the PPSP group were significantly higher than scores in the group without PPSP. Multiple regression analysis showed that axillary lymph node dissection (ALND) and 1-month postoperative CS-related symptoms were independent predictors of PPSP intensity and interference at 1 year postoperatively (p < 0.01).
Conclusion
We found that ALND and 1-month postoperative CS-related symptoms were predictors of PPSP intensity and interference at 1 year postoperatively.

Similar content being viewed by others
Availability of data and materials
The datasets are available from the corresponding author on reasonable request.
References
Wang K, Yee C, Tam S, Drost L, Chan S, Zaki P, et al. Prevalence of pain in patients with breast cancer post-treatment: a systematic review. Breast. 2018;42:113–27.
Wang L, Guyatt GH, Kennedy SA, Romerosa B, Kwon HY, Kaushal A, et al. Predictors of persistent pain after breast cancer surgery: a systematic review and meta-analysis of observational studies. CMAJ. 2016;4(188):E352–61.
Manfuku M, Nishigami T, Mibu A, Tanaka K, Kitagaki K, Sumiyoshi K. Comparison of central sensitization-related symptoms and health-related quality of life between breast cancer survivors with and without chronic pain and healthy controls. Breast Cancer. 2019;26:758–65.
Kojima K, Kitahara M, Matoba M, Shimoyama N, Uezono S. Survey on recognition of post-mastectomy pain syndrome by breast specialist physician and present status of treatment in Japan. Breast Cancer. 2014;21:191–7.
Leysen L, Beckwée D, Nijs J, Pas R, Bilterys T, Vermeir S, et al. Risk factors of pain in breast cancer survivors: a systematic review and meta-analysis. Support Care Cancer. 2017;25:3607–43.
McCowat M, Fleming L, Vibholm J, Dixon D. The psychological predictors of acute and chronic pain in women following breast cancer surgery: a systematic review. Clin J Pain. 2019;35:261–71.
Mustonen L, Aho T, Harno H, Sipilä R, Meretoja T, Kalso E. What makes surgical nerve injury painful? A 4-year to 9-year follow-up of patients with intercostobrachial nerve resection in women treated for breast cancer. Pain. 2019;160:246–56.
Schreiber KL, Zinboonyahgoon N, Flowers KM, Hruschak V, Fields KG, Patton ME, et al. Prediction of persistent pain severity and impact 12 months after breast surgery using comprehensive preoperative assessment of biopsychosocial pain modulators. Ann Surg Oncol. 2021;28:5015–38.
Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(S2–15):16.
Nijs J, Leysen L, Adriaenssens N, Aguilar Ferrándiz ME, Devoogdt N, Tassenoy A, et al. Pain following cancer treatment: guidelines for the clinical classification of predominant neuropathic, nociceptive and central sensitization pain. Acta Oncol. 2016;55:659–63.
Scerbo T, Colasurdo J, Dunn S, Unger J, Nijs J, Chad C. Measurement properties of the central sensitization inventory: a systematic review. Pain Pract. 2018;18:544–54.
Cuesta-Vargas AI, Neblett R, Nijs J, Chiarotto A, Kregel J, van Wilgen CP, et al. Establishing central sensitization-related symptom severity subgroups: a multicountry study using the central sensitization inventory. Pain Med. 2020;21(10):2430–40.
Kim SH, Yoon KB, Yoon DM, Yoo JH, Ahn KR. Influence of centrally mediated symptoms on postoperative pain in osteoarthritis patients undergoing total knee arthroplasty: a prospective observational evaluation. Pain Pract. 2015;15:E46-53.
Bennett EE, Walsh KM, Thompson NR, Krishnaney AA. Central sensitization inventory as a predictor of worse quality of life measures and increased length of stay following spinal fusion. World Neurosurg. 2017;104:594–600.
Lundblad H, Kreicbergs A, Jansson KA. Prediction of persistent pain after total knee replacement for osteoarthritis. J Bone Jt Surg Br. 2008;90:166–71.
Schreiber KL, Zinboonyahgoon N, Xu X, Spivey T, King T, Dominici L, et al. Preoperative psychosocial and psychophysical phenotypes as predictors of acute pain outcomes after breast surgery. J Pain. 2019;20:540–56.
Sipilä RM, Haasio L, Meretoja TJ, Ripatti S, Estlander AM, Kalso EA. Does expecting more pain make it more intense? Factors associated with the first week pain trajectories after breast cancer surgery. Pain. 2017;158:922–30.
Dams L, Van der Gucht E, Haenen V, Lauwers M, De Pauw S, Steurs T, et al. Biopsychosocial risk factors for pain and pain-related disability 1 year after surgery for breast cancer. Supp Care Cancer. 2022;30:4465–75.
Smith G. Step away from stepwise. J Big Data. 2018;5:32.
Uki J, Mendoza T, Cleeland CS, Nakamura Y, Takeda F. A brief cancer pain assessment tool in Japanese: the utility of the Japanese Brief Pain Inventory—BPI-J. J Pain Symptom Manage. 1998;16:364–73.
Harrington S, Gilchrist L, Sander A. Breast cancer EDGE task force outcomes: clinical measures of pain. Rehabil Oncol. 2014;32:13–21.
Tanaka K, Nishigami T, Mibu A, Manfuku M, Yono S, Shinohara Y, et al. Validation of the Japanese version of the Central Sensitization Inventory in patients with musculoskeletal disorders. PLoS ONE. 2017;12: e0188719.
Hurth A, Steege JN, Scheepbouwer P, Roose E, Lahousse A, Leysen L, et al. Assessment of central sensitization in breast cancer survivors: convergent validity and use of the central sensitization inventory (CSI) and its short-form as a clustering tool. Clin Pract. 2021;1131:607–18.
Sullivan M, Bishop S, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7:524–32.
Sullivan ML. The pain catastrophizing scale—user manual. Montreal, Quebec: McGill University; 2009.
Wheeler CHB, Williams AC, Morley SJ. Meta-analysis of the psychometric properties of the pain catastrophizing scale and associations with participant characteristics. Pain. 2019;160:1946–53.
Staples LG, Dear BF, Gandy M, Fogliati V, Fogliati R, Karin E, et al. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: the PHQ-2, GAD-2, and K-6. Gen Hosp Psychiatry. 2019;56:13–8.
Rolke R, Baron R, Maier C, Tölle TR, Treede DR, Beyer A, et al. Quantitative sensory testing in the German research network on neuropathic pain (DFNS): standardized protocol and reference values. Pain. 2006;123:231–43.
Neogi T, Frey-Law L, Scholz J, Niu J, Arendt-Nielsen L, Woolf C, et al. Sensitivity and sensitisation in relation to pain severity in knee osteoarthritis: trait or state? Ann Rheum Dis. 2015;74:682–8.
Dams L, Haenen V, Van der Gucht E, Devoogdt N, Smeets A, Bernar K, et al. Absolute and relative reliability of a comprehensive quantitative sensory testing protocol in women treated for breast cancer. Pain Med. 2022;23:1162–75.
Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. 1st ed. New York, NY: Springer-Verlag; 2001.
Leysen L, Cools W, Nijs J, Adriaenssens N, Pas R, Van Wilgen CP, et al. The mediating effect of pain catastrophizing and perceived injustice in the relationship of pain on health-related quality of life in breast cancer survivors. Support Care Cancer. 2021;29:5653–61.
Lahousse A, Ivakhnov S, Nijs J, Beckwée D, Cools W, de Las F, Penas C, et al. The mediating effect of perceived injustice and pain catastrophizing in the relationship of pain on fatigue and sleep in breast cancer survivors: a cross-sectional study. Pain Med. 2022;10:006.
Lautenbacher S, Peters JH, Heesen M, Scheel J, Kunz M. Age changes in pain perception: a systematic-review and meta-analysis of age effects on pain and tolerance thresholds. Neurosci Biobehav Rev. 2017;75:104–13.
Johansen A, Schirmer H, Stubhaug A, Nielsen CS. Persistent post-surgical pain and experimental pain sensitivity in the Tromsø study: comorbid pain matters. Pain. 2014;155:341–8.
Arendt-Nielsen L, Nie H, Laursen MB, Laursen BS, Madeleine P, Simonsen OH, et al. Sensitization in patients with painful knee osteoarthritis. Pain. 2010;149:573–81.
Johannsen M, Frederiksen Y, Jensen AB, Zachariae R. Psychosocial predictors of posttreatment pain after nonmetastatic breast cancer treatment: a systematic review and meta-analysis of prospective studies. J Pain Res. 2018;11:23–36.
Yuksel SS, Chappell AG, Jackson BT, Wescott AB, Ellis MF. Post mastectomy pain syndrome: a systematic review of prevention modalities. JPRAS Open. 2022;31:32–49.
Mathieu J, Daneau C, Lemeunier N, Doyon A, Marchand AA, Descarreaux M. Conservative interventions and clinical outcome measures used in the perioperative rehabilitation of breast cancer patients undergoing mastectomy: a scoping review. BMC Womens Health. 2022;22:343.
Huang J, Chan PSF, Lok V, Chen X, Ding H, Jin Y, et al. Global incidence and mortality of breast cancer: a trend analysis. Aging (Albany NY). 2021;13:5748–803.
Acknowledgements
The authors are extremely grateful to the survivors who participated in this study and Izumi Kameyama, Yumi Nakakura, Yasuko Tanaka, and Naoko Takahashi for assistance with data collection. We thank the Edanz for editing a draft of this manuscript.
Funding
The authors declare no funding sources directly relevant to the study.
Author information
Authors and Affiliations
Contributions
All authors contributed significantly to the preparation of this manuscript. Concept/idea/research design: M.M, T.N. Writing: M.M, T.N, A.M, H.Y, R.I, Data collection: M.M, H.K, K.S. Data analysis: M.M, T.N, R.I. Project management: T.N. Providing participants: K.S.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval, consent to participate, and consent for publication
This study was ethical approval by the Institutional Ethics Committee of Konan Women’s University (2017006). All participants have provided written informed consent to participate in the study and to present or publish anonymized data before the study and consent has been obtained. The study was conducted according to the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Manfuku, M., Nishigami, T., Mibu, A. et al. Predictors of persistent post-surgical pain intensity and interference at 1 year after breast cancer surgery: assessing central sensitization, central sensitivity symptoms, and psychological factors. Breast Cancer 30, 271–281 (2023). https://doi.org/10.1007/s12282-022-01420-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-022-01420-7