Abstract
Purpose
Knowledge regarding risk factors for pain in the long term after surgery for breast cancer may be of great value in preventing this prevalent and debilitating side effect. Despite the biopsychosocial nature of pain, the predictive value of both pre- and postoperative biopsychosocial functioning for long-term pain intensity and pain-related disability has not yet been studied.
Methods
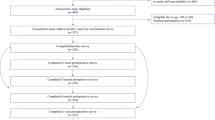
One hundred sixty-six women planned for unilateral breast cancer surgery were included in this prospective cohort study. Pre- and postoperative outcomes related to pain, psychosocial, and somatosensory functioning (questionnaires and quantitative sensory testing) were evaluated as risk factors for pain intensity (visual analog scale) and pain-related disability (pain disability index) 1 year after surgery for breast cancer. Both bivariable and stepwise linear regression analyses were performed.
Results
The most consistent biopsychosocial risk factors were symptoms related to altered central somatosensory functioning (central sensitization inventory), psychological symptoms, and social support (psychological symptoms and support subscale of McGill Quality of Life Questionnaire). Results also showed that a pre- and postoperative disturbed functioning of the somatosensory nervous system in the surgical area could provide additional information regarding pain intensity or pain-related disability in the long term after surgery for breast cancer.
Conclusion
This study revealed several biopsychosocial characteristics that might be used to identify women more vulnerable to have pain and pain-related disability in the long term after surgery for breast cancer, allowing for more effective pain management and prevention.
Similar content being viewed by others
Data availability
All authors have full control of all primary data and agree to allow the journal to review their data if requested.
Code availability
Not applicable.
References
Wang L, Cohen JC, Devasenapathy N et al (2020) Prevalence and intensity of persistent post-surgical pain following breast cancer surgery: a systematic review and meta-analysis of observational studies. Br J Anaesth 125(3):346–357
Sung H, Ferlay J, Siegel RL et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021
Mattiuzzi C, Lippi G (2019) Current Cancer Epidemiology. J Epidemiol Glob Health 9(4):217–222
Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I (2016) A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res 9:457–467
Ferreira VT, Dibai-Filho AV, Kelly de Oliveira A, Gomes CA, Melo ES, Maria de Almeida A (2015) Assessing the impact of pain on the life of breast cancer survivors using the Brief Pain Inventory. J Phys Ther Sci. 27(5):1361–3
Habib AS, Kertai MD, Cooter M, Greenup RA, Hwang S (2019) Risk factors for severe acute pain and persistent pain after surgery for breast cancer: a prospective observational study. Reg Anesth Pain Med 44(2):192–199
Leysen L, Beckwée D, Nijs J et al (2017) Risk factors of pain in breast cancer survivors: a systematic review and meta-analysis. Support Care Cancer 25(12):3607–3643
Nishimura D, Kosugi S, Onishi Y et al (2017) Psychological and endocrine factors and pain after mastectomy. Eur J Pain 21(7):1144–1153
Bruce J, Thornton AJ, Powell R et al (2014) Psychological, surgical, and sociodemographic predictors of pain outcomes after breast cancer surgery: a population-based cohort study. Pain 155(2):232–243
Mejdahl MK, Mertz BG, Bidstrup PE, Andersen KG (2015) Preoperative distress predicts persistent pain after breast cancer treatment: a prospective cohort study. J Natl Compr Canc Netw. 13(8):995–1003 (quiz 1003)
Baudic S, Jayr C, Albi-Feldzer A et al (2016) Effect of alexithymia and emotional repression on postsurgical pain in women with breast cancer: a prospective longitudinal 12-month study. J Pain 17(1):90–100
Schreiber KL, Zinboonyahgoon N, Flowers KM et al. (2021) Prediction of persistent pain severity and impact 12 months after breast surgery using comprehensive preoperative assessment of biopsychosocial pain modulators. Ann Surg Oncol
Mustonen L, Vollert J, Rice ASC, Kalso E, Harno H (2020) Sensory profiles in women with neuropathic pain after breast cancer surgery. Breast Cancer Res Treat 182(2):305–315
Martland ME, Rashidi AS, Bennett MI et al (2020) The use of quantitative sensory testing in cancer pain assessment: A systematic review. Eur J Pain 24(4):669–684
Arendt-Nielsen L, Morlion B, Perrot S et al (2018) Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur J Pain 22(2):216–241
Treede RD, Jensen TS, Campbell JN et al (2008) Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 70(18):1630–1635
Mayer TG, Neblett R, Cohen H et al (2012) The development and psychometric validation of the central sensitization inventory. Pain Pract 12(4):276–285
Andersen KG, Duriaud HM, Aasvang EK, Kehlet H (2015) Association between sensory dysfunction and pain 1 week after breast cancer surgery: a psychophysical study. Acta Anaesthesiol Scand 60(2):259–269
Reid-Arndt SA, Cox CR (2012) Stress, coping and cognitive deficits in women after surgery for breast cancer. J Clin Psychol Med Settings 19(2):127–137
De Groef A, Devoogdt N, Van der Gucht E et al (2019) EduCan trial: study protocol for a randomised controlled trial on the effectiveness of pain neuroscience education after breast cancer surgery on pain, physical, emotional and work-related functioning. BMJ Open. 9(1):e025742
Kjeldsen HB, Klausen TW, Rosenberg J (2016) Preferred presentation of the visual analog scale for measurement of postoperative pain. Pain Pract 16(8):980–984
Harrington S, Gilchrist L, Sander A (2014) Breast cancer EDGE task force outcomes: clinical measures of pain. Rehabil Oncol 32(1):13–21
Pollard CA (1984) Preliminary validity study of the pain disability index. Percept Mot Skills 59(3):974
Soer R, Köke AJ, Vroomen PC et al. Extensive validation of the pain disability index in 3 groups of patients with musculoskeletal pain. Spine (Phila Pa 1976). 2013;38(9):E562–8.
Rolke RMW, Campbell KA, Schalber C, Caspari S, Birklein F, Treede RD (2006) Quantitative sensory testing: a comprehensive protocol for clinical trials. Eur J Pain 10(1):77–88
Granovsky YM-BA, Goldstein O, Sprecher E, Yarnitsky D (2016) CPM Test-retest reliability: “standard” vs “single test-stimulus” protocols. Pain Med. 17(3):521–9
Sullivan MJL, Bishop SR, Pivik J (1995) The Pain Catastrophizing Scale: development and validation. Psychol Assess 7:524–532
Cohen SR, Mount BM (2000) Living with cancer: “good” days and “bad” days–what produces them? Can the McGill quality of life questionnaire distinguish between them? Cancer 89(8):1854–1865
Portney LG (2020) Foundations of clinical research: applications to evidence-based practice. In: WM. PL, editor. Philadelphia: F.A. Davis Company
Edwards RR, Mensing G, Cahalan C et al (2013) Alteration in pain modulation in women with persistent pain after lumpectomy: influence of catastrophizing. J Pain Symptom Manage 46(1):30–42
Burns LC, Ritvo SE, Ferguson MK, Clarke H, Ze Seltzer, Katz J (2015) Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: a systematic review. Journal of Pain Research. 8:21–32
Woolf CJ (2011) Central sensitization: implications for the diagnosis and treatment of pain. Pain 152(3 Suppl):S2-s15
Coronado RA, George SZ (2018) The Central Sensitization Inventory and Pain Sensitivity Questionnaire: an exploration of construct validity and associations with widespread pain sensitivity among individuals with shoulder pain. Musculoskelet Sci Pract 36:61–67
Bezerra MC, Bittencourt JV, Reis FJJ, de Almeida RS, Meziat-Filho NAM, Nogueira LAC (2020) Central Sensitization Inventory is a useless instrument for detection of the impairment of the conditioned pain modulation in patients with chronic musculoskeletal pain. Joint Bone Spine. 105127
Gervais-Hupé J, Pollice J, Sadi J, Carlesso LC (2018) Validity of the central sensitization inventory with measures of sensitization in people with knee osteoarthritis. Clin Rheumatol 37(11):3125–3132
Kregel J, Schumacher C, Dolphens M et al (2018) Convergent validity of the Dutch central sensitization inventory: associations with psychophysical pain measures, quality of life, disability, and pain cognitions in patients with chronic spinal pain. Pain Pract 18(6):777–787
Hendriks E, Voogt L, Lenoir D, Coppieters I, Ickmans K (2020) Convergent validity of the central sensitization inventory in chronic Whiplash-associated disorders; associations with quantitative sensory testing, pain intensity, fatigue, and psychosocial factors. Pain Med
Clark JR, Nijs J, Yeowell G, Holmes P, Goodwin PC (2019) Trait sensitivity, anxiety, and personality are predictive of central sensitization symptoms in patients with chronic low back pain. Pain Pract 19(8):800–810
Dijkstra PU, Rietman JS, Geertzen JH (2007) Phantom breast sensations and phantom breast pain: a 2-year prospective study and a methodological analysis of literature. Eur J Pain 11(1):99–108
Leung J, Pachana NA, McLaughlin D (2014) Social support and health-related quality of life in women with breast cancer: a longitudinal study. Psychooncology 23(9):1014–1020
Johannsen M, Frederiksen Y, Jensen AB, Zachariae R (2018) Psychosocial predictors of posttreatment pain after nonmetastatic breast cancer treatment: a systematic review and meta-analysis of prospective studies. J Pain Res 11:23–36
Kerns RD, Rosenberg R, Otis JD (2002) Self-appraised problem solving and pain-relevant social support as predictors of the experience of chronic pain. Ann Behav Med 24(2):100–105
Andersen KG, Duriaud HM, Kehlet H, Aasvang EK (2017) The relationship between sensory loss and persistent pain 1 year after breast cancer surgery. J Pain 18(9):1129–1138
van Helmond N, Aarts HM, Timmerman H et al (2020) Is preoperative quantitative sensory testing related to persistent postsurgical pain? A Systematic Literature Review Anesth Analg 131(4):1146–1155
Dams L, Haenen V, Van der Gucht E et al (2021) Absolute and relative reliability of a comprehensive quantitative sensory testing protocol in women treated for breast cancer. Pain Med
Funding
The study is funded by Research Foundations—Flanders (FWO) (T005117N).
Author information
Authors and Affiliations
Contributions
Mrs. Lore Dams: defining the study concept and design, recruitment of participants, acquisition, analysis and interpretation of data, drafting the manuscript for important intellectual content, manuscript writing, approval of the final version to be published.
Mr. Vincent Haenen, Mrs. Elien Van der Gucht, Mrs. Magalie Lauwers, Mrs. Tinne Steurs, Mrs. Sofie De Pauw, Mr. Koen Bernar, Dr. Tessa De Vrieze: recruitment of participants, acquisition, analysis and interpretation of data, drafting the manuscript for important intellectual content, approval of the final version to be published.
Prof. Dr. Ann Smeets: recruitment of participants, drafting the manuscript for important intellectual content, approval of the final version to be published.
Prof. Dr. Nele Devoogdt, Dr. An De Groef, Prof. Dr. Mira Meeus: defining the study concept and design, analysis and interpretation of data, drafting the manuscript for important intellectual content, approval of the final version to be published.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethical Committee of the University Hospitals of Leuven (s60702).
Consent to participate
All included patients provided written informed consent.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dams, L., Van der Gucht, E., Haenen, V. et al. Biopsychosocial risk factors for pain and pain-related disability 1 year after surgery for breast cancer. Support Care Cancer 30, 4465–4475 (2022). https://doi.org/10.1007/s00520-022-06805-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06805-0