Abstract
Background
The role of elastography for breast tumors is still ambiguous. The purpose of this study was to inquire how effectively elastography can be used in the diagnosis of breast tumors.
Methods
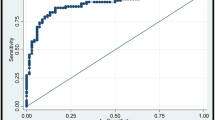
The fat lesion ratio (FLR) of 244 lesions (99 malignant and 145 benign lesions) was calculated using tissue Doppler imaging with elastography. The pathological confirmations were performed by core needle or excisional biopsy. Conventional ultrasonography (US) findings were classified according to the Breast Imaging Reporting and Data System. We tried to set the region of interest (ROI) at the hardest area of the target and measured the maximum FLR (max-FLR) of the target with elastography, whereas the control ROI was placed in the subcutaneous adipose tissue. The diagnostic potential of the max-FLR combined with the US category was evaluated.
Results
The mean max-FLR of malignant lesions was significantly greater than that of benign lesions, at 11.0 and 4.4, respectively (p < 0.01). The max-FLR showed a wide overlap range between benign and malignant lesions, but there were no malignant lesions showing a less than 2.0 max-FLR. Ninety-six percent of the lesions interpreted as category 3 were benign, and the negative predictive value measuring the max-FLR was kept at 98% as long as the max-FLR was less than 4.0. Measuring the max-FLR may reduce unnecessary biopsies by 57.5% in the category 3 group.
Conclusions
Combining conventional US categories and measuring max-FLR with elastography may be helpful in reducing the number of unnecessary biopsies in category 3 lesions.



Similar content being viewed by others
References
Cho N, Moon WK, Park JS, Cha JH, Jang M, Seong MH. Nonpalpable breast masses evaluation by elastography. Korean J Radiol. 2008;9(2):111–8.
Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, et al. Clinical application of US elastography for diagnosis. Radiology. 2006;239(2):341–50.
Fleury EFC, Fleury JCV, Piato S, Jr Roveda D, et al. New elastographic classification of breast lesions during and after compression. Diagn Interv Radiol. 2009;15:96–103.
Kumm TR, Szabunio MM. Elastography for the characterization of breast lesions: initial clinical experience. Cancer Control. 2010;17(3):56–61.
American College of Radiology. Breast imaging reporting and data system (BI-RADS), ultrasound. 4th ed. Reston : American College of Radiology; 2003.
Moon WK, Huang CS, Shen WC, Takada E, Chang RF, Joe J, et al. Analysis of elatographic features at sonoelastography for breast tumor classification. Ultrasound Med Biol. 2009; 35(11):1794–802.
Raza S, Odulate A, Ong EMW, Ong EMW, Chikarmane S. Using real-time tissue elastography for breast lesion evaluation. J Ultrasound Med. 2010;29:551–63.
Schaefer FK, Heer I, Schaefer PJ, Mundhenke C, Osterholz S, Order BM, et al. Breast ultrasound elastography—results of 193 breast lesions in a prospective study with histopathologic correlation. Eur J Radiol. 2009; doi:10.1016/j.ejrad.2009.08.026.
Sohn YM, Kim MJ, Kim EK, Kwak JY, Moon HJ, Kim SJ. Sonographic elastography combined with conventional sonography. How much is it helpful for diagnostic performance? J Ultrasound Med. 2009;28:413–20.
Cho N, Moon WK, Kim HY, Chang JM, Park SH, Lyou CY. Sonoelastographic strain index for differentiation of benign and malignant nonpalpable breast masses. J Ultrasound Med. 2010;29:1–7.
Zhi H, Xiao XY, Yang HY, Ou B, Wen YL, Luo BM. Ultrasonic elastography in breast cancer diagnosis: strain ratio vs 5-point scale. Acad Radiol. 2010; doi:10.1016/j.acra.2010.05.004.
Thomas A, Degenhardt F, Farrokh A, Wojcinski S, Slowinski T, Fisher T. Significant differentiation of focal breast lesions: calculation of strain ratio in breast sonoelastography. Acad Radiol. 2010;17:558–63.
Farrokh A, Wojcinski S, Degenhardt F. Diagnostic value of strain ratio measurement in the differentiation of malignant and benign breast lesions (in French with English abstract). Ultraschall Med. 2010. doi: 10.1055/s-0029-1245335 accessed 10 Aug 2010.
Tardvion A, EI Khoury C, Thibault F, Wyler A, Barreau B, Neuenschwander S, et al. Elastography of the breast: a prospective study of 122 lesions (in French with English abstract). J Radiol. 2007;88(5 Pt 1):657–62.
Acknowledgments
This study was supported by Dr. Masatsugu Shiba and the sonographers working at Osaka City General Hospital in Osaka City who analyzed and collected our data.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ikeda, K., Ogawa, Y., Takii, M. et al. A role for elastography in the diagnosis of breast lesions by measuring the maximum fat lesion ratio (max-FLR) by tissue Doppler imaging. Breast Cancer 19, 71–76 (2012). https://doi.org/10.1007/s12282-011-0274-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-011-0274-5