Abstract
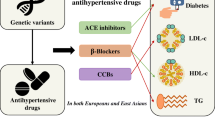
In this work, we aim to evaluate the association of the genetically proxied effect of metformin on blood pressure (BP) and hypertension through a drug target-based Mendelian randomization (MR) analysis. Thirty-two instrumental variables for five metformin targets (i.e., AMP-activated protein kinase (AMPK), growth differentiation factor 15 (GDF15), mitochondrial glycerol 3 (MG3), mitochondrial complex I (MCI), and glucagon (GCG)) were introduced to the MR analysis on the datasets of hypertension, systolic and diastolic blood pressure (SBP and DBP). The MR analyses demonstrated that the MCI- and MG3-specific metformin’s use would significantly reduce SBP, DBP, and hypertension risk. The meta-analyses showed that the genetically proxied metformin’s use equivalent to a 6.75 mmol/mol reduction on HbA1c could decrease both the SBP (beta = − 1.05, P < 0.001) and DBP (beta = − 0.51, P = 0.096). Furthermore, metformin’s use was also implied to reduce the hypertension risk. The MG3- and MCI-dependent metformin’s effect may play key roles in the anti-hypertension function.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is the leading modifiable risk factor for cardiovascular diseases, affecting more than 1.5 billion people globally [1]. Metformin, one of the most widely recommended first-line pharmacotherapies for managing type 2 diabetes (T2D), has been reported to improve cardiovascular outcomes which probably via lowering blood pressure (BP) [2]. Fanghänel et al. [3] noted that metformin treatment lowered BP in patients with diabetes. Similar findings were reported in several randomized controlled trials (RCTs) involving patients with portal hypertension [4]. A meta-analysis of 26 RCTs containing 4119 patients indicated that metformin could effectively decrease systolic blood pressure (SBP) [5]. However, previous findings were inconsistent, with some studies indicating no remarkable effect of metformin on reducing BP [5]. A meta-analysis based on 41 RCTs (3074 patients) reached the opposite conclusion that metformin had no significant effect on BP [6]. Notably, these studies had intrinsic methodologic limitations, including small sample sizes and selection bias. Whether metformin had an effect on BP and hypertension is currently unclear.
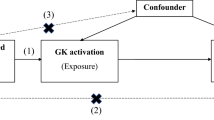
Mendelian randomization (MR) analysis, a complementary and alternative approach to RCTs, is a powerful statistical method that uses the significantly associated single nucleotide polymorphisms (SNPs) as instrumental variables (IVs) to quantify potential causal effects. Drug exerts their effects by regulating the pharmacological targets’ expression, and the naturally occurring human genetic variation can serve as a proxy for therapeutic drug targets’ reaction [7]. A recently developed extension to the MR paradigm, i.e., the drug target-based MR study, has been used to find the drug-repurposing candidates for various diseases [8]. The objective of this study was to estimate the causal effect of metformin on hypertension in a larger European population using drug target-based MR. The present findings may potentially offer novel prevention and treatment strategies for hypertension.
Methods
The Genetic IVs for Five Metformin Targets
Zheng and colleagues have explored the causal relationship between metformin and Alzheimer’s disease risk through a drug target-based MR approach [9]. They have identified 32 IVs for five primary drug targets (i.e., AMP-activated protein kinase (AMPK), growth differentiation factor 15 (GDF15), mitochondrial glycerol 3 (MG3), mitochondrial complex I (MCI), and glucagon (GCG)) and 23 drug target-associated genes (DTGs) of metformin (see Fig. 1 and supplementary Table 7A of Zheng et al. [9]). In order to identify the valid IVs, their selection process not only complied with the three key assumptions of MR analysis but also performed additional tests. For instance, they confirmed the human tissue expression of the selected genes with the data from GTEX, eQTLGen, and Zheng et al. [10,11,12]. Besides, as a positive control, the authors verified metformin’s effect on reducing T2D risk and HbA1c using the MR method [9]. According to the authors, one standard deviation (SD) unit lowering of the HbA1c equals to 6.75 mmol/mol reduction of HbA1c [9]. Besides, the current study was also conducted under the guidance of the STROBE-MR checklist (see Table S1).
The Information on the Outcome Datasets of Hypertension and Blood Pressure
The GWAS datasets for hypertension were acquired from two independent cohorts. Hypertension cohort 1 came from the UK biobank and contained 462,933 participants (119,731 hypertension patients and 343,202 healthy controls) [13]. Hypertension cohort 2 derived from the Finnish biobank project FinnGen (https://www.finngen.fi/fi). Its sample size was 218,754, with 55,917 being hypertension patients and 162,837 being healthy controls [14]. Their GWAS summary statistics data were acquired through the platform of the IEU OpenGWAS project (https://gwas.mrcieu.ac.uk/datasets, GWAS ID: “ukb-b-14057,” “finn-b-I9_HYPTENS”) [15]. The GWAS data for SBP and diastolic blood pressure (DBP) were provided by the International Consortium of Blood Pressure (ICBP) [16]. The study included 757,601 participants of European descent. The basic information of the included four outcome datasets was summarized in Fig. 1.
MR Analysis and Meta-analysis
In the MR analysis, the inverse-variance weighted (IVW) (when IVs > 2) and Wald ratio (when IVs ≤ 2) approaches were selected to be the major analytical tools. Other sensitivity methods such as MR Egger, weighted median, weighted mode, and simple mode were employed to assess the robustness of the conclusions of the MR analysis with IVs > 2. The fixed-effect and random-effect statistical models were employed for the meta-analysis. All analyses were conducted with R packages MRPRESSO (version 1.0), ieugwasr (version 0.1.5), TwoSampleMR (version 0.5.6), and meta (version 6.0–0) [15, 17, 18]. A P value less than 0.05 was considered statistically significant.
Test the Influence of Potential Confounders
To test whether the metformin target-associated blood lowering effect was influenced by the confounders such as body mass index (BMI), smoking, and alcohol consumption, the multiple variable Mendelian randomization (MVMR) was performed. Their GWAS summary statistics data were acquired through the platform of the IEU OpenGWAS project (https://gwas.mrcieu.ac.uk/datasets, GWAS ID: “ukb-b-19953,” “ieu-b-4877,” and “ukb-b-5779”).
Results
The MR Analyses of 5 Drug Targets on SBP, DBP, and Hypertension
The MR estimates of metformin drug targets on SBP, DBP, and 2 hypertension cohorts were summarized in Table 1. When the IVs for exposure and its potential proxy SNPs cannot be found in the outcome dataset, they were excluded from further analyses. Therefore, only four targets were kept for the analyses on SBP. We noticed that the MG3- and MCI-dependent metformin effects were confirmed to reduce both SBP and DBP significantly. Consistently, the MCI-specific metformin influence was also identified to remarkably diminish the risk of hypertension in both tested hypertension cohorts. Besides, in hypertension cohort 1, the MG3- and AMPK-dependent metformin effects also demonstrated obvious anti-hypertension function. As shown in Supplementary Table S2-S5, the pleiotropy tests of AMPK- and MCI-specific metformin’s effect on SBP, DBP, and hypertension indicated no significant results. We also did not detect remarkable heterogeneity results in the AMPK study. However, the test of MCI demonstrated significant heterogeneity results (Supplementary Table S2-S5). The sensitivity analyses on AMPK and MCI suggested that the effects were robust to various MR approaches (Supplementary Table S6-S7).
Metformin’s Effect on the SBP and DBP
In the MR analysis, the GCG-specific SNP and its proxy were not found in the GWAS dataset of SBP, and therefore, it was excluded from the meta-analysis. As shown in Fig. 2A, the metformin’s targets could decrease both the SBP and DBP. In the analysis of SBP, four metformin targets were all confirmed to influence blood pressure reduction. The MG3-, MIC-, and AMPK-specific metformin’s effects were statistically significant. Similarly, these four targets also demonstrated the ability to reduce DBP, with the MG3- and MCI-specific effects being proven to be statistically significant (see Fig. 2B). Notably, the MG3-specific influence was confirmed to have the most substantial effect among the four targets.
Metformin’s Effect on the Risk of Hypertension
In the MR analysis, we evaluated the effects of metformin on two independent hypertension cohorts. Though the random effect model meta-analysis suggested no remarkable effect of metformin target on reducing hypertension’s risk, the common effect model indicated a significant effect of metformin targets on decreasing hypertension risk (see Fig. 2C and D). Among five targets, the AMPK- and MCI-specific effects of metformin were consistent in two MR analyses and played key roles in reducing hypertension’s risk. In the MR analysis on hypertension cohort 2, the MG3-specific metformin’s effect showed no significant effect on the risk of hypertension. However, it was identified to reduce the risk of hypertension in cohort 1 significantly. The GCG-specific metformin’s effect was confirmed to have little effect on hypertension’s risk. The GDF15-specific metformin effect was implied to increase hypertension risk in two MR analyses.
The Analyses of Potential Confounders
In order to rule out the potential influence of some potential confounding factors (e.g., BMI, smoking, and alcohol consumption) on the metformin targets-specific HbA1c lowering effect, the MVMR analyses were conducted. The basic information of three potential confounder datasets was summarized in Supplementary Table S8. However, during the process of extracting the IVs of exposures for MVMR, we noticed that the valid IVs representing the BMI, smoking, and alcohol consumption had no significant effect sizes on HbA1c levels (all relevant SNPs with a P value more than 5E − 8, see Table S9-S11). It indicates that the MVMRs were unfeasible here and those factors were hardly to influence our abovementioned conclusions.
Discussion
To the best of our knowledge, the present work is the first MR study to investigate metformin’s genetically predicted therapeutic effects on BP and hypertension. Basing on the data from large‐scale GWAS studies in two independent hypertension cohorts of 175,648 patients, we observed that genetically proxied metformin use leads to a 13% reduction of hypertension risk, which may be owed to its ability to decrease SBP and DBP. Among five drug targets, metformin may exert its anti-blood pressure activities majorly through regulating MG3 and MCI. Collectively, these findings reported a suggestive benefit of metformin in reducing BP and provided novel evidence to guide hypertension prevention.
Metformin is recommended as the first-line treatment for T2D and is proposed to be beneficial for cardiovascular outcomes. Several earlier RCTs have suggested that metformin can significantly reduce BP in diabetic and hypertensive individuals. In addition to these human studies, several rodent studies have also provided evidence for BP-lowering effect of metformin. Kosegawa et al. observed that the SBP levels were significantly lower in the metformin group than in the controls group [19]. The effect of metformin on reducing BP in streptozotocin-induced diabetic rats was also observed in another animal trial conducted by Majithiya and Balaraman [20]. These results from RCTs and experimental studies are consistent with our findings. However, in contrast, some studies did not confirm a significant effect of metformin on reducing BP. Although the reason is unclear, the conflictive results might be due to multiple causes, such as small sample sizes, selection bias, differences in study populations, and strategies of BP measurement. Further prospective RCTs with multi-ethnic, larger sample sizes are needed.
Our findings suggest that MG3 and MCI may be the potential target for the effect of metformin on reducing BP. The MG3 target-associated gene GPD2 encoded the mitochondrial glycerol 3-phosphate dehydrogenase (mGPDH), which is further partly used as a glycerol backbone for lipid molecules. Recent studies have shown that mGPDH was associated with kidney disease and macrophage inflammatory activities [21, 22]. We hypothesized that metformin might reduce BP through these mechanisms [23]. Furthermore, we also found that the inhibition of expression of an MCI-related gene could be associated with the effect of metformin on reducing BP. Intriguingly, the previous report has also confirmed that the inhibition of MCI would diminish hypertension in mice model [24].
The current work still has limitations. First, though the 5 drug targets may recapitulate the major effect of metformin use, the possibility that some undiscovered targets would greatly affect the metformin response cannot be totally precluded. Second, future studies focusing on the validation of the included DTGs are still needed since the present DTGs derive from the database and systemic literature review and thus lack the direct evidences from biological tests [9]. Third, our study analyzed only the data from European participants which may limit the generalizability of the conclusion in other populations.
Conclusion
In summary, the present study provided novel evidences to support the causal effect of metformin on reducing hypertension risk. We revealed that metformin might decrease BP through the inhibition of MG3 and MCI. These findings implied the repurposing of metformin for cardiovascular diseases. However, randomized trials with large samples are still warranted to provide more robust conclusions.
Data availability
The used GWAS data were publicly available and their origins were described appropriately in the manuscript. The detailed information and codes required to reanalyze the data in this work are available from the corresponding authors upon reasonable request.
References
GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923–94.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-Year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–89.
Fanghänel G, Sánchez-Reyes L, Trujillo C, Sotres D, Espinosa-Campos J. Metformin’s effects on glucose and lipid metabolism in patients with secondary failure to sulfonylureas. Diabetes Care. 1996;19(11):1185–9.
Rittig N, Aagaard NK, Villadsen GE, Sandahl TD, Jessen N, Grønbaek H, et al. Randomised clinical study: acute effects of metformin versus placebo on portal pressure in patients with cirrhosis and portal hypertension. Aliment Pharmacol Ther. 2021;54(3):320–8.
Zhou L, Liu H, Wen X, Peng Y, Tian Y, Zhao L. Effects of metformin on blood pressure in nondiabetic patients: a meta-analysis of randomized controlled trials. J Hypertens. 2017;35(1):18–26.
Wulffelé MG, Kooy A, de Zeeuw D, Stehouwer CD, Gansevoort RT. The effect of metformin on blood pressure, plasma cholesterol and triglycerides in type 2 diabetes mellitus: a systematic review. J Intern Med. 2004;256(1):1–14.
Holmes MV. Human genetics and drug development. N Engl J Med. 2019;380(11):1076–9.
Gordillo-Marañón M, Zwierzyna M. Validation of lipid-related therapeutic targets for coronary heart disease prevention using human genetics. Nat Commun. 2021;12(1):6120.
Zheng J, Xu M, Walker V, Yuan J, Korologou-Linden R, Robinson J, et al. Evaluating the efficacy and mechanism of metformin targets on reducing Alzheimer’s disease risk in the general population: a Mendelian randomisation study. Diabetologia. 2022;65(10):1664–75.
GTEx Consortium. The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science. 2020;369(6509):1318–30.
Võsa U, Claringbould A, Westra H-J, Bonder MJ, Deelen P, Zeng B, et al. Large-scale cis- and trans-eQTL analyses identify thousands of genetic loci and polygenic scores that regulate blood gene expression. Nat Genet. 2021;53(9):1300–10.
Zheng J, Haberland V, Baird D, Walker V, Haycock PC, Hurle MR, et al. Phenome-wide Mendelian randomization mapping the influence of the plasma proteome on complex diseases. Nat Genet. 2020;52(10):1122–31.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562(7726):203–9.
Kurki MI, Karjalainen J, Palta P, Sipilä TP, Kristiansson K, Donner KM, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature. 2023;613(7944):508–18.
Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife. 2018;7:e34408.
Giri A, Hellwege JN, Keaton JM, Park J, Qiu C, Warren HR, et al. Trans-ethnic association study of blood pressure determinants in over 750,000 individuals. Nat Genet. 2019;51(1):51–62.
Verbanck M, Chen C-Y, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693–8.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153–60.
Kosegawa I, Katayama S, Kikuchi C, Kashiwabara H, Negishi K, Ishii J, et al. Metformin decreases blood pressure and obesity in OLETF rats via improvement of insulin resistance. Hypertens Res: Off J Japan Soc Hypertens. 1996;19(1):37–41.
Majithiya JB, Balaraman R. Metformin reduces blood pressure and restores endothelial function in aorta of streptozotocin-induced diabetic rats. Life Sci. 2006;78(22):2615–24.
Qu H, Gong X, Liu X, Zhang R, Wang Y, Huang B, et al. Deficiency of mitochondrial glycerol 3-phosphate dehydrogenase exacerbates podocyte injury and the progression of diabetic kidney disease. Diabetes. 2021;70(6):1372–87.
Langston PK, Nambu A. Glycerol phosphate shuttle enzyme GPD2 regulates macrophage inflammatory responses. Nat Immunol. 2019;20(9):1186–95.
Justin Rucker A, Crowley SD. The role of macrophages in hypertension and its complications. Pflugers Arch. 2017;469(3–4):419–30.
Zhang A, Jia Z, Wang N, Tidwell TJ, Yang T. Relative contributions of mitochondria and NADPH oxidase to deoxycorticosterone acetate-salt hypertension in mice. Kidney Int. 2011;80(1):51–60.
Acknowledgements
The authors want to express great thanks to the researchers and participants who made the relevant GWAS summary statistics publicly available.
Author information
Authors and Affiliations
Consortia
Contributions
Conception, supervision, and administration: ZL and QZ; data curation: JJ and DH; investigation: JJ and DH; methodology: ZL and QZ; writing—original draft: JJ and DH; writing—review and editing: ZL and QZ.
Corresponding authors
Ethics declarations
Ethics Approval
The used GWAS data were publicly available and approved by their corresponding institutions. An ethics approval for the current work is not required. No animal subjects were used in this work.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Editor-in-Chief Enrique Lara-Pezzi oversaw the review of this article
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, J., Hu, D., Zhang, Q. et al. Genetically Proxied Therapeutic Effect of Metformin Use, Blood Pressure, and Hypertension’s Risk: a Drug Target-Based Mendelian Randomization Study. J. of Cardiovasc. Trans. Res. 17, 716–722 (2024). https://doi.org/10.1007/s12265-023-10460-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-023-10460-z