Abstract
Global longitudinal strain and circumferential strain are found to be reduced in HFpEF, which some have interpreted that the global left ventricular (LV) contractility is impaired. This finding is, however, contradicted by a preserved ejection fraction (EF) and confounded by changes in LV geometry and afterload resistance that may also affect the global strains. To reconcile these issues, we used a validated computational framework consisting of a finite element LV model to isolate the effects of HFpEF features in affecting systolic function metrics. Simulations were performed to quantify the effects on myocardial strains due to changes in LV geometry, active tension developed by the tissue, and afterload. We found that only a reduction in myocardial contractility and an increase in afterload can simultaneously reproduce the blood pressures, EF and strains measured in HFpEF patients. This finding suggests that it is likely that the myocardial contractility is reduced in HFpEF patients.

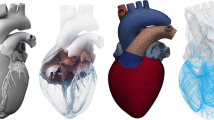
Graphical abstract






Similar content being viewed by others
Abbreviations
- DBP:
-
Diastolic blood pressure
- EF:
-
Ejection fraction
- EDV:
-
End-diastolic volume
- E ll :
-
Global longitudinal strain
- E cc :
-
Global circumferential strain
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- HF:
-
Heart failure
- FE:
-
Finite element
- LV:
-
Left ventricle
- R a, d :
-
Peripheral resistance parameter
- SBP:
-
Systolic blood pressure
- T ref :
-
Active tension parameter
References
Bhatia, R. S., Tu, J. V., Lee, D. S., et al. (2006). Outcome of heart failure with preserved ejection fraction in a population-based study. The New England Journal of Medicine, 355(3), 260–269. https://doi.org/10.1056/NEJMoa051530.
Owan, T. E., Hodge, D. O., Herges, R. M., Jacobsen, S. J., Roger, V. L., & Redfield, M. M. (2006). Trends in prevalence and outcome of heart failure with preserved ejection fraction. The New England Journal of Medicine, 355(3), 251–259. https://doi.org/10.1056/NEJMoa052256.
Borlaug, B. A., & Paulus, W. J. (2011). Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. European Heart Journal, 32(6), 670–679. https://doi.org/10.1093/eurheartj/ehq426.
Somaratne, J. B., Berry, C., McMurray, J. J. V., Poppe, K. K., Doughty, R. N., & Whalley, G. A. (2009). The prognostic significance of heart failure with preserved left ventricular ejection fraction: a literature-based meta-analysis. European Journal of Heart Failure, 11(9), 855–862. https://doi.org/10.1093/eurjhf/hfp103.
Tribouilloy, C., Rusinaru, D., Mahjoub, H., et al. (2008). Prognosis of heart failure with preserved ejection fraction: a 5 year prospective population-based study. European Heart Journal, 29(3), 339–347. https://doi.org/10.1093/eurheartj/ehm554.
Asif, M., Egan, J., Vasan, S., et al. (2000). An advanced glycation endproduct cross-link breaker can reverse age-related increases in myocardial stiffness. Proceedings of the National Academy of Sciences. https://doi.org/10.1073/pnas.040558497.
Liu, J., Masurekar, M. R., Vatner, D. E., et al. (2003). Glycation end-product cross-link breaker reduces collagen and improves cardiac function in aging diabetic heart. American Journal of Physiology. Heart and Circulatory Physiology. https://doi.org/10.1152/ajpheart.00516.2003.
Solomon, S. D., Zile, M., Pieske, B., et al. (2012). The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet. https://doi.org/10.1016/S0140-6736(12)61227-6.
Van Tassell, B. W., Arena, R., Biondi-Zoccai, G., et al. (2014). Effects of interleukin-1 blockade with anakinra on aerobic exercise capacity in patients with heart failure and preserved ejection fraction (from the D-HART Pilot Study). The American Journal of Cardiology. https://doi.org/10.1016/j.amjcard.2013.08.047.
Yamagami, K., Oka, T., Wang, Q., et al. (2015). Pirfenidone exhibits cardioprotective effects by regulating myocardial fibrosis and vascular permeability in pressure overloaded hearts. American Journal of Physiology. Heart and Circulatory Physiology. https://doi.org/10.1152/ajpheart.00137.2015.
Roh, J., Houstis, N., & Rosenzweig, A. (2017). Why don’t we have proven treatments for HFpEF? Circulation Research, 120(8), 1243–1245. https://doi.org/10.1161/CIRCRESAHA.116.310119.
Ponikowski, P., Voors, A. A., Anker, S. D., et al. (2016). ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal, 37(27), 2129-2200m. https://doi.org/10.1093/eurheartj/ehw128.
Sengupta, P. P., & Marwick, T. H. (2018). The many dimensions of diastolic function: a curse or a blessing? JACC: Cardiovascular Imaging. https://doi.org/10.1016/j.jcmg.2017.05.015.
Zile, M. R., Baicu, C. F., & Gaasch, W. H. (2004). Diastolic heart failure—abnormalities in active relaxation and passive stiffness of the left ventricle. The New England Journal of Medicine, 350(19), 1953–1959. https://doi.org/10.1056/NEJMoa032566.
Velagaleti, R. S., Gona, P., Pencina, M. J., et al. (2014). Left ventricular hypertrophy patterns and incidence of heart failure with preserved versus reduced ejection fraction. The American Journal of Cardiology, 113(1), 117–122. https://doi.org/10.1016/j.amjcard.2013.09.028.
Zile, M. R., Gaasch, W. H., Carroll, J. D., et al. (2001). Heart failure with a normal ejection fraction: is measurement of diastolic function necessary to make the diagnosis of diastolic heart failure? Circulation, 104, 779–782. https://doi.org/10.1161/hc3201.094226.
Kraigher-Krainer, E., Shah, A. M., Gupta, D. K., et al. (2014). Impaired systolic function by strain imaging in heart failure with preserved ejection fraction. Journal of the American College of Cardiology, 63(5), 447–455. https://doi.org/10.1016/j.jacc.2013.09.052.
Zou, H., Xi, C., Zhao, X., et al. (2018). Quantification of biventricular strains in heart failure with preserved ejection fraction patient using hyperelastic warping method. Frontiers in Physiology, 9, 1295. https://doi.org/10.3389/fphys.2018.01295.
Morris, D. A., Ma, X.-X., Belyavskiy, E., et al. (2017). Left ventricular longitudinal systolic function analysed by 2D speckle-tracking echocardiography in heart failure with preserved ejection fraction: a meta-analysis. Open Hear, 4(2). https://doi.org/10.1136/openhrt-2017-000630.
Shah, A. M., Claggett, B., Sweitzer, N. K., et al. (2015). Prognostic importance of changes in cardiac structure and function in heart failure with preserved ejection fraction and the impact of spironolactone. Circulation. Heart Failure. https://doi.org/10.1161/CIRCHEARTFAILURE.115.002249.
Kawaguchi, M., Hay, I., Fetics, B., & Kass, D. A. (2003). Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: Implications for systolic and diastolic reserve limitations. Circulation, 107(5), 714–720. https://doi.org/10.1161/01.CIR.0000048123.22359.A0.
Borlaug, B. A., Lam, C. S. P., Roger, V. L., Rodeheffer, R. J., & Redfield, M. M. (2009). Contractility and ventricular systolic stiffening in hypertensive heart disease insights into the pathogenesis of heart failure with preserved ejection fraction. Journal of the American College of Cardiology, 54(5), 410–418. https://doi.org/10.1016/j.jacc.2009.05.013.
Dabiri, Y., Sack, K. L., Shaul, S., Sengupta, P. P., & Guccione, J. M. (2018). Relationship of transmural variations in myofiber contractility to left ventricular ejection fraction: Implications for modeling heart failure phenotype with preserved ejection fraction. Frontiers in Physiology. https://doi.org/10.3389/fphys.2018.01003.
Genet, M., Lee, L. C., Baillargeon, B., Guccione, J. M., & Kuhl, E. (2016). Modeling pathologies of diastolic and systolic heart failure. Annals of Biomedical Engineering, 44(1), 112–127. https://doi.org/10.1007/s10439-015-1351-2.
Adeniran, I., MacIver, D. H., Hancox, J. C., & Zhang, H. (2015). Abnormal calcium homeostasis in heart failure with preserved ejection fraction is related to both reduced contractile function and incomplete relaxation: An electromechanically detailed biophysical modeling study. Frontiers in Physiology. https://doi.org/10.3389/fphys.2015.00078.
MacIver, D. H., & Townsend, M. (2008). A novel mechanism of heart failure with normal ejection fraction. Heart. https://doi.org/10.1136/hrt.2006.114082.
Shavik, S. M., Wall, S. T., Sundnes, J., Burkhoff, D., & Lee, L. C. (2017). Organ-level validation of a cross-bridge cycling descriptor in a left ventricular finite element model: effects of ventricular loading on myocardial strains. Physics Reports, 5(21), e13392. https://doi.org/10.14814/phy2.13392.
Shavik, S.-M., Zhong, L., Zhao, X., & Lee, L. C. (2019). In-silico assessment of the effects of right ventricular assist device on pulmonary arterial hypertension using an image based biventricular modeling framework. Mechanics Research Communications, 97, 101–111.
Guccione, J. M., Waldman, L. K., & McCulloch, A. D. (1993). Mechanics of active contraction in cardiac muscle : Part II—cylindrical models of the systolic left ventricle. Journal of Biomechanical Engineering, 115(February), 82–90.
Guccione, J. M., Mcculloch, A. D., & Waldman, L. K. (1991). Passive material properties of intact ventricular myocardium determined from a cylindrical model. Journal of Biomechanical Engineering, 113(1), 42–55.
Logg, A., Wells, G. N., & Mardel, K. A. (2012). Automated solution of differential equations by the finite element method., 84. https://doi.org/10.1007/978-3-642-23099-8.
Maurer, M. S., King, D. L., El-Khoury Rumbarger, L., Packer, M., & Burkhoff, D. (2005). Left heart failure with a normal ejection fraction: Identification of different pathophysiologic mechanisms. Journal of Cardiac Failure, 11(3), 177–187. https://doi.org/10.1016/j.cardfail.2004.10.006.
Shah, A. M. (2013). Ventricular remodeling in heart failure with preserved ejection fraction. Current Heart Failure Reports, 10(4), 341–349. https://doi.org/10.1007/s11897-013-0166-4.
Maurer, M. S., Burkhoff, D., Fried, L. P., Gottdiener, J., King, D. L., & Kitzman, D. W. (2007). Ventricular structure and function in hypertensive participants with heart failure and a normal ejection fraction. The Cardiovascular Health Study. Journal of the American College of Cardiology. https://doi.org/10.1016/j.jacc.2006.10.061.
Prasad, A., Hastings, J. L., Shibata, S., et al. (2010). Characterization of static and dynamic left ventricular diastolic function in patients with heart failure with a preserved ejection fraction. Circulation. Heart Failure, 3(5), 617–626. https://doi.org/10.1161/CIRCHEARTFAILURE.109.867044.
Zile, M. R., Baicu, C. F., Ikonomidis, J. S., et al. (2015). Myocardial stiffness in patients with heart failure and a preserved ejection fraction contributions of collagen and titin. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.114.013215.
Shavik, S. M., Jiang, Z., Baek, S., & Lee, L. C. (2018). High spatial resolution multi-organ finite element modeling of ventricular-arterial coupling. Frontiers in Physiology, 9(MAR). https://doi.org/10.3389/fphys.2018.00119.
Shavik, S. M., Tossas-Betancourt, C., Figueroa, C. A., Baek, S., & Lee, L. C. (2020). Multiscale modeling framework of ventricular-arterial bi-directional interactions in the cardiopulmonary circulation. Frontiers in Physiology, 11, 2. https://doi.org/10.3389/fphys.2020.00002.
Streeter, D. D., Spotnitz, H. M., Patel, D. P., Ross, J., & Sonnenblick, E. H. (1969). Fiber orientation in the canine left ventricle during diastole and systole. Circulation Research, 24(3), 339–347. https://doi.org/10.1161/01.RES.24.3.339.
He, K.-L., Burkhoff, D., Leng, W.-X., et al. (2009). Comparison of ventricular structure and function in Chinese patients with heart failure and ejection fractions >55% versus 40% to 55% versus. The American Journal of Cardiology, 103(6), 845–851. https://doi.org/10.1016/j.amjcard.2008.11.050.
Mascherbauer, J., Zotter-Tufaro, C., Duca, F., et al. (2017). Wedge pressure rather than left ventricular end-diastolic pressure predicts outcome in heart failure with preserved ejection fraction. JACC Hear Fail. https://doi.org/10.1016/j.jchf.2017.08.005.
Borlaug, B. A., Jaber, W. A., Ommen, S. R., Lam, C. S. P., Redfield, M. M., & Nishimura, R. A. (2011). Diastolic relaxation and compliance reserve during dynamic exercise in heart failure with preserved ejection fraction. Heart. https://doi.org/10.1136/hrt.2010.212787.
Lam, C. S. P., Donal, E., Kraigher-Krainer, E., & Vasan, R. S. (2011). Epidemiology and clinical course of heart failure with preserved ejection fraction. European Journal of Heart Failure, 13(1), 18–28. https://doi.org/10.1093/eurjhf/hfq121.
Westermann, D., Kasner, M., Steendijk, P., et al. (2008). Role of left ventricular stiffness in heart failure with normal ejection fraction. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.107.716886.
Gorcsan, J., & Tanaka, H. (2011). Echocardiographic assessment of myocardial strain. Journal of the American College of Cardiology, 58(14), 1401–1413. https://doi.org/10.1016/j.jacc.2011.06.038.
Smiseth, O. A., Torp, H., Opdahl, A., Haugaa, K. H., & Urheim, S. (2015). Myocardial strain imaging: how useful is it in clinical decision making? European Heart Journal, 37(15), 1196–1207. https://doi.org/10.1093/eurheartj/ehv529.
Hoit, B. D. (2011). Strain and strain rate echocardiography and coronary artery disease. Circulation. Cardiovascular Imaging, 4(2), 179–190. https://doi.org/10.1161/CIRCIMAGING.110.959817.
Butler, J., Hamo, C. E., Udelson, J. E., et al. (2016). Exploring new endpoints for patients with heart failure with preserved ejection fraction. Circulation. Heart Failure. https://doi.org/10.1161/CIRCHEARTFAILURE.116.003358.
Luo, C., Ramachandran, D., Ware, D. L., Ma, T. S., & Clark, J. W. (2011). Modeling left ventricular diastolic dysfunction: classification and key indicators. Theoretical Biology & Medical Modelling. https://doi.org/10.1186/1742-4682-8-14.
Donaldson, C., Palmer, B. M., Zile, M., et al. (2012). Myosin cross-bridge dynamics in patients with hypertension and concentric left ventricular remodeling. Circulation. Heart Failure, 5(6), 803–811. https://doi.org/10.1161/CIRCHEARTFAILURE.112.968925.
Borbély, A., Van Der Velden, J., Papp, Z., et al. (2005). Cardiomyocyte stiffness in diastolic heart failure. Circulation, 111(6), 774–781. https://doi.org/10.1161/01.CIR.0000155257.33485.6D.
Tanacli, R., Hashemi, D., Neye, M., et al. (2020). Multilayer myocardial strain improves the diagnosis of heart failure with preserved ejection fraction. ESC Hear Fail. https://doi.org/10.1002/ehf2.12826.
Xu, L., Pagano, J. J., Haykowksy, M. J., et al. (2020). Layer-specific strain in patients with heart failure using cardiovascular magnetic resonance: not all layers are the same. Journal of Cardiovascular Magnetic Resonance. https://doi.org/10.1186/s12968-020-00680-6.
Smith, S. P., Secomb, T. W., Hong, B. D., & Moulton, M. J. (2016). Time-dependent regional myocardial strains in patients with heart failure with a preserved ejection fraction. BioMed Research International. https://doi.org/10.1155/2016/8957307.
Gotschy, A., Von Deuster, C., Van Gorkum, R. J. H., et al. (2019). Characterizing cardiac involvement in amyloidosis using cardiovascular magnetic resonance diffusion tensor imaging. Journal of Cardiovascular Magnetic Resonance. https://doi.org/10.1186/s12968-019-0563-2.
Pearlman, E. S., Weber, K. T., Janicki, J. S., Pietra, G. G., & Fishman, A. P. (1982). Muscle fiber orientation and connective tissue content in the hypertrophied human heart. Laboratory Investigation.
Ennis, D. B., Nguyen, T. C., Riboh, J. C., et al. (2008). Myofiber angle distributions in the ovine left ventricle do not conform to computationally optimized predictions. Journal of Biomechanics. https://doi.org/10.1016/j.jbiomech.2008.08.007.
Triposkiadis, F., Butler, J., Abboud, F. M., et al. (2019). The continuous heart failure spectrum: Moving beyond an ejection fraction classification. European Heart Journal. https://doi.org/10.1093/eurheartj/ehz158.
Bers, D. M. (2002). Cardiac excitation-contraction coupling. Nature. https://doi.org/10.1038/415198a.
Kelshiker, M., Mayet, J., Unsworth, B., & Okonko, D. (2014). Basal septal hypertrophy. Current Cardiology Reviews. https://doi.org/10.2174/1573403X09666131202125424.
Weiss, H. R., Neubauer, J. A., Lipp, J. A., & Sinha, A. K. (1978). Quantitative determination of regional oxygen consumption in the dog heart. Circulatory Shock, 42(3), 394–401. https://doi.org/10.1161/01.res.42.3.394.
Duncker, D. J., Ishibashi, Y., & Bache, R. J. (1998). Effect of treadmill exercise on transmural distribution of blood flow in hypertrophied left ventricle. American Journal of Physiology. Heart and Circulatory Physiology, 275(4 44-4), 1274–1282. https://doi.org/10.1152/ajpheart.1998.275.4.h1274.
Tan, Y. T., Wenzelburger, F., Lee, E., et al. (2009). The pathophysiology of heart failure with normal ejection fraction. Exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion. Journal of the American College of Cardiology. https://doi.org/10.1016/j.jacc.2009.03.037.
Santos, A. B. S., Roca, G. Q., Claggett, B., et al. (2016). Prognostic relevance of left atrial dysfunction in heart failure with preserved ejection fraction. Circulation. Heart Failure. https://doi.org/10.1161/CIRCHEARTFAILURE.115.002763.
Bianco, C. M., Farjo, P. D., Ghaffar, Y. A., & Sengupta, P. P. (2020). Myocardial mechanics in patients with normal LVEF and diastolic dysfunction. JACC: Cardiovascular Imaging. https://doi.org/10.1016/j.jcmg.2018.12.035.
Park, J. J., Park, J. B., Park, J. H., & Cho, G. Y. (2018). Global longitudinal strain to predict mortality in patients with acute heart failure. Journal of the American College of Cardiology. https://doi.org/10.1016/j.jacc.2018.02.064.
Punnoose, L., Burkhoff, D., Rich, S., & Horn, E. M. (2012). Right ventricular assist device in end-stage pulmonary arterial hypertension: insights from a computational model of the cardiovascular system. Progress in Cardiovascular Diseases, 55(2), 234–243.e2. https://doi.org/10.1016/j.pcad.2012.07.008.
Pezzuto, S., & Ambrosi, D. (2014). Active contraction of the cardiac ventricle and distortion of the microstructural architecture. International Journal of Numerical Methods in Biomedical Engineering, 30(12), 1578–1596. https://doi.org/10.1002/cnm.2690.
Pezzuto, S., Ambrosi, D., & Quarteroni, A. (2014). An orthotropic active-strain model for the myocardium mechanics and its numerical approximation. European Journal of Mechanics - A/Solids, 48(1), 83–96. https://doi.org/10.1016/j.euromechsol.2014.03.006.
Funding
This study was funded by the American Heart Association (AHA) grant 17SDG33370110 and the National Institutes of Health (NIH) R01 HL134841.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All the authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Associate Editor Ana Barac oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
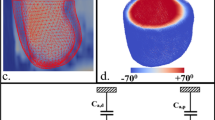
Closed Loop Systemic Circulatory Model
The LV FE model was coupled to a closed loop lumped-parameter circulatory model that describes the systemic circulation (Fig. 1), which is similar to our previous work [27]. The modeling framework consists of five compartments of the systemic circulation namely, LV, LA, proximal artery, distal artery, and vein. The total mass of blood needs to be conserved in the circulatory model, which requires that the rate of volume change in each storage compartment of the circulatory system to the inflow and outflow rates by the following relations,
where VLA, VLV, Va, p, Va, d, and Vven are volumes of LV, LA, proximal artery, distal artery, and vein, respectively, and qven, qmv, qao, qa, p, and qa, d are flow rates at different segments. Flowrate at different segments of the circulatory model depends on their resistance to flow (Rao, Ra, p, Ra, d, Rven, and Rmv) and the pressure difference between the connecting storage compartments (i.e., pressure gradient). The flow rates are given by
Pressure in each storage compartment is a function of its volume. A simplified pressure–volume relationship
was prescribed for the proximal artery, distal artery, and veins, where Vap, 0, Vad, 0, and Vven, 0 are constant resting volumes of the proximal artery, distal artery, and veins. Ca, p, Ca, d, and Cven are the total compliance of the proximal artery, distal artery, and venous system. On the other hand, pressure in the left atrium PLA(t) was prescribed to be a function of its volume VLA(t) by the following equations that describe its contraction using a time-varying elastance function [67]
where
and,
In Eqs. (5a–b), Ees, LA is the end-systolic elastance of the left atrium, V0, LA is the volume axis intercept of the end-systolic pressure–volume relationship (ESPVR), and both ALA and BLA are parameters of the end-diastolic pressure–volume relationship (EDPVR) of the left atrium. The driving function e(t) is given in Eq. (5c) in which tmax is the point of maximal chamber elastance and τ is the time constant of relaxation. The values of Ees, LA, V0, LA, ALA, BLA, tmax, and τLA are listed in Table 3.
Finally, pressure in the LV depends on its corresponding volume through nonclosed form function
The functional relationship between pressure and volume in the LV was obtained using the FE method as described in the next section. Parameter values associated with the closed loop circulatory model are tabulated in Table 4.
Finite Element Formulation of the LV
The weak form associated with finite element formulation of the LV was derived based on the minimization of the following Lagrangian functional [28, 37],
where, u is the displacement field, Pcav is the Lagrange multiplier to constrain the LV cavity volume Vcav(u) to a prescribed value V [68], p is a Lagrange multiplier to enforce incompressibility of the tissue (i.e., Jacobian of the deformation gradient tensor J = 1), and both c1 and c2 are Lagrange multipliers to constrain rigid body translation (i.e., zero mean translation) and rotation (i.e., zero mean rotation) [[69]]. The LV cavity volume Vcav is a function of the displacement u and is defined by
where Ωinner is the volume enclosed by the inner surface Γinner and the basal surface at z = 0, and n is the outward unit normal vector.
Pressure–volume relationship of the LV required in the lumped parameter circulatory model (i.e., Eqs. (6)) was defined by the solution obtained from minimizing the functional [27]. Taking the first variation of the functional in Eq. (7) leads to the following expression:
In Eq. (9), P is the first Piola Kirchhoff stress tensor, F is the deformation gradient tensor, δu, δp, δPcav, δc1, δc2 are the variation of the displacement field, Lagrange multipliers for enforcing incompressibility and volume constraint, zero mean translation and rotation, respectively. The Euler-Lagrange problem then becomes finding u ∈ H1(Ω0), p ∈ L2(Ω0), Pcav ∈ ℝ, c1 ∈ ℝ3, c2 ∈ ℝ3 that satisfies
and u(x, y, 0).n|base = 0 (for constraining the basal deformation to be in-plane) ∀δu(Ω0), δp ∈ L2(Ω0), δPcav ∈ ℝ, δc1 ∈ ℝ3, δc2 ∈ ℝ3.
Constitutive Law of the LV
An active stress formulation was used to describe the LV’s mechanical behavior in the cardiac cycle. In this formulation, the stress tensor P can be decomposed additively into a passive component Pp and an active component Pa (i.e., P = Pa + Pp). The passive stress tensor was defined by Pp = dW/dF, where W is a strain energy function of a Fung-type transversely isotropic hyperelastic material [30] given by
where,
In Eq. (11), Eij with (i, j) ∈ (f, s, n) are components of the Green–Lagrange strain tensor E with f, s, n denoting the myocardial fiber, sheet, and sheet normal directions, respectively. Material parameters of the passive constitutive model are denoted by C, bff, bxx, and bfx.
The active stress Pa was calculated along the local fiber direction using a modified time varying elastance model,
In the above equation, ef and \( {\mathbf{e}}_{f_0} \) are, respectively, the local vectors defining the muscle fiber direction in the current and reference configuration, Tref is the reference tension and Ca0 denotes the peak intracellular calcium concentration. The length dependent calcium sensitivity ECa50 and the variable Ct are given by [29]
In Eq. (13), B is a constant, (Ca0)max is the maximum peak intracellular calcium concentration and l0 is the sarcomere length at which no active tension develops. In Eq. (14), t0 is the time taken to reach the peak tension, tt is the time at which isovolumic relaxation of LV starts and τ is the time constant of the isovolumic relaxation. Parameter values associated with the LV model are tabulated in Table 5.
Parameters for each simulation cases are tabulated in Table 6.
Rights and permissions
About this article
Cite this article
Shavik, S.M., Wall, S., Sundnes, J. et al. Computational Modeling Studies of the Roles of Left Ventricular Geometry, Afterload, and Muscle Contractility on Myocardial Strains in Heart Failure with Preserved Ejection Fraction. J. of Cardiovasc. Trans. Res. 14, 1131–1145 (2021). https://doi.org/10.1007/s12265-021-10130-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-021-10130-y