Abstract
To determine whether the presence of ischemic heart disease (IHD) per se, or rather the co-presence of heart failure (HF), is the primum movens for less effective stem cell products in autologous stem cell therapy, we assessed numbers and function of bone marrow (BM)-derived progenitor cells in patients with coronary artery disease (n = 17), HF due to ischemic cardiomyopathy (n = 8), non-ischemic HF (n = 7), and control subjects (n = 11). Myeloid and erythroid differentiation capacity of BM-derived mononuclear cells was impaired in patients with underlying IHD but not with non-ischemic HF. Migration capacity decreased with increasing IHD severity. Hence, IHD, with or without associated cardiomyopathy, is an important determinant of progenitor cell function. No depletion of hematopoietic and endothelial progenitor cells (EPC) within the BM was observed, while circulating EPC numbers were increased in the presence of IHD, suggesting active recruitment. The observed myelosuppression was not driven by inflammation and thus other mechanisms are at play.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than a decade ago, the use of autologous bone marrow (BM)-derived stem cell transplantation was introduced as promising therapy to regenerate infarcted myocardium [1]. Convincing animal data set the stage for thoughtful clinical trials, testing this therapy as a “proof-of-concept.” Particularly, the total non-selected BM-derived mononuclear cell (MNC) fractions, but also mesenchymal stem cells, hematopoietic, and endothelial progenitor cells, were studied. Despite the heterogeneity in terms of stem/progenitor cell type, as well as dosing and route of administration, several meta-analyses in the field confirmed its safety and beneficial impact on left ventricular ejection fraction (LVEF), infarct size, and myocardial perfusion [2, 3]. These benefits were most likely mediated by paracrine actions of injected cells in ischemic tissue, i.e., stimulation of angiogenesis, inhibition of apoptosis of endothelial cells and cardiomyocytes, activation of cardiac stem cells, and recruitment of additional progenitor cells [4].
Despite the initial success of autologous stem cell therapy in the setting of acute myocardial infarction, the outcomes in patients with chronic ischemic heart disease (IHD) and ischemic cardiomyopathy were rather disappointing [5, 6]. Clinical trials reported a mild cardiac improvement in LVEF of ±3 % in patients with IHD, irrespective of reduced LVEF at baseline, compared to the placebo group 3–6 months after intracoronary BM-MNC administration [7, 8].
For patients with dilated cardiomyopathy, results were conflicting: the INTRACELL trial did not find any significant increase in LVEF 3 months after intramyocardial injection of BM-MNC compared to the control group [9]. In contrast, the REGENERATE-DCM trial reported a 5 % increase in LVEF 3 months after intracoronary administration of BM cells in patients with non-ischemic heart failure (HF) compared to baseline [10]. Hence, researchers were drawn back to the bench to investigate why results have proved inferior to what was anticipated from clinical studies.
At present, there is an emerging evidence base for a general myelosuppression in patients with chronic IHD, affecting both the functionality and the number of stem/progenitor cells in the BM. For example, in search for an explanation of HF-associated anemia, several groups reported a reduced proliferation and differentiation capacity of BM-derived progenitor cells in vitro in ischemic but not in dilated cardiomyopathy [11–14]. Jakob et al. demonstrated the in vivo clinical impact of this functional deficit: progenitor cells obtained from patients with ischemic cardiomyopathy showed a reduced capacity to promote cardiac function and neovascularization after myocardial injection in a hindlimb ischemia mice model when compared to progenitor cells acquired from healthy subjects [15]. Also in patients with isolated coronary artery disease (CAD), and thus without concomitant HF, intrinsic impairment of hematopoietic stem cell differentiation was observed [16].
Taken together, results from clinical trials suggest that the BM compartment in ischemic HF, and also in isolated CAD, might be dysfunctional. So far, the extent and severity of BM suppression have not been compared between these various underlying etiologies. We hypothesize that the extent of BM dysfunction will be more prominent in the presence of HF, since the existence of low-grade systemic inflammation in the HF syndrome may aggravate myelosuppression [17, 18].
In this regard, we performed a systematic evaluation of progenitor cell numbers and functionality in a broad range of cardiovascular diseases: CAD, HF due to ischemic cardiomyopathy, HF due to non-ischemic cardiomyopathy, and compared this with a healthy control group. Moreover, inflammation was explored as a potential mechanism of BM dysfunction.
Methods
Detailed methods are available in online supplementary material.
Study Population
Thirty-two patients undergoing elective cardiac surgery via median sternotomy (coronary artery bypass grafting, mitral valve surgery, or implantation of ventricular assist device) were stratified into groups according to the presence of significant IHD and/or HF. Hence, there was a first group of patients with IHD without HF (i.e., CAD group), a second group with HF due to IHD (i.e., ischemic cardiomyopathy or ICM group), and a third group with HF due to other reasons than IHD (i.e., non-ischemic HF group). Eleven subjects without significant past history of cardiovascular disease served as controls. The study complied with the Helsinki Declaration and was approved by the local ethics committee, and written informed consent was obtained from all subjects.
Sampling and Isolation of BM- and PB-MNC
In patients, BM (2 × 10 ml) was aspirated by sternal puncture under general anesthesia; arterial peripheral blood (PB, 12 ml) was sampled simultaneously via arterial catheter. In control subjects, BM was aspirated at the time of bone prelevation of the iliac crest prior to jaw reconstruction; venous PB was sampled by venipuncture. BM- and PB-MNC were isolated by density gradient centrifugation immediately after sampling.
Clinical and Biochemical Assessment
All patients underwent coronary angiography and standard transthoracic echocardiography pre-operatively to determine the complexity of IHD (Syntax score) and LVEF, respectively. The Syntax score, an angiographic tool to quantify the complexity of coronary artery lesions, was calculated using the online Syntax score calculator [19]. Physical capacity was evaluated by the 6-min walk test. The Framingham risk score representing the 10-year risk for cardiovascular disease was calculated for each patient [20]. CRP, hemoglobin, creatinine, leukocyte, total cholesterol, HDL, and LDL circulating levels were measured pre-operatively.
Assessment of BM Purity
The percentage of bone matrix vesicle-bound bone alkaline phosphatase (ALP) of total ALP activity, as a marker for the purity of BM aspirates, was quantified in BM serum as described previously [21]. BM aspirates in which the percentage of bone matrix vesicle-bound ALP was less than 15 % were excluded from the study for quality reasons.
Transwell Migration Assay of BM-MNC
In vitro migratory capacity of BM-MNC towards stromal cell-derived factor-1α (SDF-1α, 100 ng/ml, R&D Systems Europe Ltd., UK) and vascular endothelial growth factor (VEGF, 50 ng/ml, R&D Systems Europe Ltd.) was evaluated after 4 h using a modified Boyden chamber.
Colony-Forming Unit Assays
Isolated BM-MNC were aliquoted in duplicate in Methocult H4535 Enriched without EPO medium (Stem Cell Technologies, France) for induction of differentiation into the myeloid lineage (granulocyte/macrophage colony-forming units, GM-CFU), as well as in Methocult H4434 Classic medium (Stem Cell Technologies) for induction of differentiation into the erythroid lineage (erythroid burst-forming units, BFU-E). After incubation for 14 days, the number of GM-CFU and BFU-E was counted.
Paracrine Activity of BM-MNC
Isolated BM-MNC were seeded on gelatin-coated 24-well plates (5 × 106 cells/well). After incubation for 24 h, supernatant was collected, in which VEGF levels were measured using a human VEGF ELISA kit (R&D Systems Europe Ltd.).
Flow Cytometry for Hematopoietic and Endothelial Progenitor Cell Enumeration
Multiparametric flow cytometry was applied for the assessment of the cellular composition of the BM-MNC fraction, as well as for the specific enumeration of hematopoietic (HPC, CD45dimCD34+SSClow, ISHAGE gating strategy [22]) and endothelial (EPC, CD45dimCD34+KDR+, EPC-gating protocol standardized by our laboratory [23]) progenitor cells in both BM- and PB-MNC samples using APC-H7-labeled CD45 (BD), PE-Cy7-labeled CD34 (BD), and APC-labeled KDR (R&D Systems) antibodies. HPC and EPC numbers were expressed as relative numbers among CD45+ events. Early and late apoptosis was assessed by 7-AAD (BD) and FITC-labeled Annexin V staining (BD).
Inflammatory and Angiogenic Cytokine Levels
Levels of the inflammatory cytokines tumor necrosis factor alpha (TNFα), interferon gamma (IFNγ), and interleukin 6 (IL-6) and the angiogenic cytokines VEGF and basic fibroblast growth factor (bFGF) were measured in PB and BM plasma using Meso Scale Discovery multiplex platforms (Meso Scale Diagnostics, Maryland, USA).
Molecular Expression of Inflammatory and Angiogenic Receptors
Expression of TNFR1 and TNFR2 (TNFα receptors), IFNGR1 (IFNγ receptor 1), IL6-R (IL-6 receptor), CXCR4 (SDF-1α receptor), and VEGFR2 (VEGF receptor 2) in BM-MNC was normalized to GAPDH and calculated by real-time qPCR using the ΔΔCT method.
Statistical Analysis
Results are expressed as median (interquartile range (IQR)). IBM SPSS Statistics version 22.0 was used for statistical analysis. Normality of the variables was tested with Shapiro-Wilk and by visual Q–Q plot inspection. Logarithmic transformation of skewed data was done to obtain a normal distribution. Comparison between different groups was performed using ANOVA (normally distributed data), Kruskal-Wallis (skewed data), or chi-square test (nominal data), as appropriate. To evaluate the specific influence of either IHD or HF, a two-way ANOVA was performed for each parameter with IHD, HF, and the interaction between IHD and HF as independent factors. All models were adjusted for age. When the interaction between IHD and HF was not significant, it was removed from the model. Post hoc pairwise comparison was obtained by Mann–Whitney U and adjusted with the Bonferroni-Holm correction for multiple testing. Correlations were evaluated by the Pearson or Spearman test, as appropriate. A p value of <0.05 was considered statistically significant.
Results
Patient Characteristics
After exclusion of impure BM aspirates, i.e., samples that were contaminated with PB (n = 12), 43 subjects were included in the analysis. Figure 1 shows the stratification into groups based on the presence of IHD and/or HF.
Demographic and clinical characteristics of the different cohorts are depicted in Table 1. Groups were similar with respect to age and gender. Syntax scores were similar between the ICM and CAD groups, indicating a comparable IHD complexity. Patients with ICM showed significantly lower LVEF compared to patients with non-ischemic HF (p = 0.015), but New York Heart Association (NYHA) class was not different.
Furthermore, three control subjects received ACE inhibitors, beta-blockers, and/or statins as treatment for arterial hypertension or hypercholesterolemia, respectively.
Functional Analysis of BM-MNC
Table 2 shows the results for the various functional tests that were performed in BM-MNC in the four groups. The results of the two-way ANOVA model with IHD and HF are shown separately in Table 3. For all parameters, the interaction between IHD and HF was not significant and could be removed from the model.
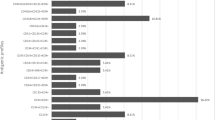
This analysis revealed a significant decrease in myeloid (GM-CFU; p = 0.009) and erythroid (BFU-E; p = 0.033) differentiation capacity of BM-MNC in the presence of IHD. This is illustrated in Fig. 2a, b. The presence of HF did not affect the differentiation capacity of BM-MNC; however, within HF patients, a significant positive correlation between GM-CFU numbers and LVEF was observed (Fig. 2c).
Functional assessment of BM-MNC of patients with IHD and HF. a In vitro myeloid (GM-CFU numbers) and b erythroid (BFU-E numbers) differentiation capacities of BM-MNC were decreased in subjects with IHD (i.e., CAD and ICM group, n = 17 + 8) compared to subjects without IHD (i.e., non-ischemic HF group and control subjects, n = 7 + 11). c In HF patients, GM-CFU numbers decrease with decreasing LVEF. d In IHD patients, migratory capacity of BM-MNC decreases with increasing IHD complexity, i.e., Syntax score. *p < 0.05 (ANOVA). e For the total cohort, age was negatively related with GM-CFU numbers and f BFU-E numbers
Additionally, whereas migratory capacity of BM-MNC did not differ between groups, it strongly correlated with IHD complexity, as assessed by the Syntax score (Fig. 2d). VEGF production of isolated BM-MNC was measured in a subset of the study population (Table 2), but no differences in VEGF production after 24-h incubation were detected between groups.
For the total cohort, a significant negative relation between age and GM-CFU (r = −0.416; p = 0.014; Fig. 2e) and BFU-E (r = −0.332; p = 0.042; Fig. 2f) was observed.
To exclude the possibility that the observed differences in myeloid and erythroid differentiation capacity are related to differences in cellular composition of the BM-MNC sample, a multiparametric flow cytometric analysis of BM-MNC was performed. In exception of higher monocyte percentages in IHD patients, BM from subjects with and subjects without IHD were comparable in cellular composition, including the ratio of lymphoblasts versus CD117+ myeloblasts (p = 0.347) or versus CD33+ myeloblasts (p = 0.347) present in the BM-MNC pool (Supplementary Table 1).
Numerical Analysis of Progenitor Cells in BM and PB
In the BM compartment, HPC and EPC numbers were comparable between the four groups (Table 2) and were not influenced by the presence of IHD and/or HF (Table 3). The percentage of BM-MNC in early and late apoptosis was significantly lower in subjects with IHD compared to subjects without IHD (Table 3).
In PB, EPC numbers were significantly elevated in the presence of IHD (p < 0.001; Fig. 3a), as well as in the presence of HF (p = 0.042, Fig. 3a). Moreover, an inverse correlation between circulating EPC numbers and LVEF was found in all patients with HF (Fig. 3b).
Enumeration of circulating hematopoietic (HPC) and endothelial (EPC) progenitor cells in patients with IHD and HF. a Circulating EPC numbers were increased in subjects with IHD (i.e., CAD and ICM group, n = 13 + 5) compared to subjects without IHD (i.e., non-ischemic HF group and control subjects, n = 7 + 11). b Circulating EPC negatively correlated with LVEF in patients with HF. c Circulating HPC numbers were elevated in subjects with HF (ICM and non-ischemic HF group, n = 5 + 7) compared to subjects without HF (CAD group and control subjects, n = 13 + 11). *p < 0.05 (ANOVA)
The presence of HF also affected circulating HPC numbers with higher numbers of HPC in subjects with HF compared to subjects without HF (p = 0.010, Table 3 and Fig. 3c).
Early and late apoptotic BM-MNC percentages were more prominent in subjects without IHD than with IHD (p = 0.051 and p = 0.037; Table 3). Yet, the degree of early and late apoptosis of freshly isolated MNC both in BM and PB was overall minimal (±<1 %).
Inflammatory and Angiogenic Cytokine Profile in BM and PB
To explore the mechanisms responsible for the aforementioned functional and numerical differences, levels of inflammatory cytokines and pro-angiogenic growth factors were studied in a subpopulation of 25 subjects.
In this entire subpopulation, levels of inflammatory cytokines were lower in BM compared to PB (IFNγ, TNFα, and IL-6), whereas levels of angiogenic growth factors (VEGF and bFGF) were higher in BM compared to PB (Supplementary Table 2).
The comparison between the four study groups is shown in Table 4. Only IL-6 levels were significantly altered: pairwise comparison showed a significant elevation of IL-6 in PB (p = 0.015), as well as in BM (p = 0.013) in patients with ICM compared to control subjects. The increases in IL-6 levels in BM and PB in patients with non-ischemic HF were not significant (PB IL-6, p = 0.059 and BM IL-6, p = 0.113); however, both BM and PB IL-6 concentrations correlated negatively with LVEF (BM IL-6, r = −0.556, p = 0.025; PB IL-6, r = −0.708, p = 0.002) and 6-MWT (BM IL-6, r = −0.886, p = 0.019; PB IL-6, r = −0.886, p = 0.019). Moreover, TNFα and IFNγ levels in BM were increased in patients with CAD compared to control subjects, but this was not significant.
Neither IL-6, TNFα, IFNγ, nor VEGF and bFGF levels in BM and PB correlated with any functional parameter or progenitor cell number in the study population.
Cytokine Receptor Expression on BM-MNC
Expression of cytokine receptors (TNFR1 and 2, IFNGR1, IL-6R) and receptors involved in the mobilization of BM-MNC into the circulation (VEGFR2, CXCR4) were analyzed to evaluate the sensitivity of the BM-MNC to the aforementioned cytokines and to gain more insight in the leading factor for mobilization.
Expression levels of these receptors on BM-MNC did not show any significant up- or downregulation between groups and thus appeared to be unaffected by either the presence of IHD and/or HF (Supplementary Table 3).
An increase in TNFα levels in BM was associated with an upregulation of TNFR2 expression (BM, r = 0.536, p = 0.007) in the study population. In turn, TNFR2 expression was negatively related to both GM-CFU (r = −0.428, p = 0.015) and BFU-E (r = −0.629, p = 0.005) numbers. Moreover, the ratio of TNFR1 to TNFR2 expression on BM-MNC, which gives an indication for cell survival (low ratio) or apoptosis (high ratio), did not differ between groups. In patients with HF, no increase in TNFα was observed, but a negative correlation with LVEF and TNFR1 expression on BM-MNC (r = −0.642, p = 0.010) was documented. Circulating EPC numbers were correlated with CXCR4 expression on BM-MNC (r = 0.364, p = 0.034).
Discussion
The present study is the first to provide a comprehensive analysis of the numbers and function of BM-derived progenitor cells in the setting of IHD and HF. Several interesting findings emerge from this study:
-
1.
Both myeloid and erythroid differentiation capacities of BM-MNC are impaired in the presence of IHD. Moreover, BM-MNC show attenuated migratory capacity with increasing complexity of angiographic lesions.
-
2.
We did not observe a depletion of progenitor cells in the BM compartment, neither in IHD nor in HF. These data suggest that the impairment of progenitor cells in the BM in IHD is restricted to a functional limitation and not to numerical values.
-
3.
The decline in functionality of BM-MNC in IHD is not driven by low-grade systemic inflammation.
-
4.
EPC mobilization from the BM into the circulation in IHD patients appears to involve CXCR4-mediated signaling.
Functional Impairment of BM-Derived Progenitor Cells in IHD
Several studies previously reported reduced in vitro GM-CFU and BFU-E capacity of isolated BM-MNC in the setting of ICM (LVEF < 45–40 %, NYHA II–IV) compared to healthy subjects [11, 12, 14]. Liguori et al. also observed this functional impairment in patients with CAD without the clinical presence of HF (LVEF >45 %, NYHA I) [16]. In this study, we confirmed the reduced myeloid/erythroid differentiation capacity of BM-MNC in CAD but distinguished the effect of IHD versus HF. Surprisingly, we identified only IHD, but not HF, as an important determinant of BM-MNC differentiation capacity. This finding is in line with the work of Kissel et al. who observed lower GM-CFU numbers in ICM patients (previous MI, LVEF 32 ± 11 %) but not in age-matched patients with dilated cardiomyopathy (LVEF 27 ± 9 %) [12].
Heeschen et al. also documented a reduced migratory response towards SDF-1α and VEGF of BM-MNC in 18 patients with ICM (previous MI, LVEF 38 ± 11 %) [14]. In our study, however, migratory capacity of BM-MNC was not influenced by the presence of IHD nor by HF. This discrepancy could be explained by the differences in study population: the ICM patients in the study of Heeschen et al. were 17 % diabetic and compared to significantly younger healthy subjects [14]. Both diabetes and age are known influencing determinants of the progenitor cell function (see infra) [24, 25]. Therefore, we assigned diabetes as exclusion criterion in our study and corrected for the confounding age effect in our analyses.
In the present study, we demonstrated a significant inverse relation between the migratory capacity of BM-MNC and the complexity of IHD, as assessed by the Syntax score. The observation that severity of IHD is an important determinant of progenitor cell function has been suggested earlier by Bozdag-Turan et al.: CD34+/CD45+ and CD133+/CD45+ progenitor cells isolated from peripheral blood showed a reduced erythroid-myeloid differentiation capacity and migratory response towards VEGF/SDF-1α in patients with IHD, which all decreased further with increasing number of diseased coronary arteries [26].
In conclusion, this study extends previous observations and shows that, in the setting of IHD, myeloid and erythroid differentiation capacities of progenitor cells are already impaired when still residing in the BM compartment. This impairment in functionality worsens further with increasing complexity of CAD but is not observed in non-ischemic HF. Our findings identify IHD rather that the HF syndrome itself as primum movens for the observed functional impairment of BM cells. We acknowledge that these results do not support our initial hypothesis: since HF is regarded as a multi-system disorder that also accounts for several peripheral abnormalities such as endothelial dysfunction, skeletal muscle changes, and ventilatory inefficiency [27], we also anticipated an associated BM dysfunction. Yet, our results suggest otherwise and are in accordance with the findings from Kissel et al. [12] and Liguori et al. [16], as discussed above. In this regard, our focus in the quest to reveal the underlying mechanisms for this functional BM deficit in this patient group should also shift towards ischemia-induced pathways.
Increased EPC Recruitment into the Circulation in IHD
The fact that we did not observe a depletion of HPC and EPC in the BM compartment, neither in IHD nor in HF, is in line with the findings from Kissel et al. [12] and Heeschen et al. [14], who did not find any differences in ICM compared to healthy subjects either. However, while we used the ISHAGE characterization (CD45dimCD34+SSClow) for HPC enumeration in BM, both groups applied CD34+CD45+ BM-MNC as HPC phenotype characterization and CD34+CD133+ BM-MNC for immature HPC. This is in contrast with the findings from Liguori et al. [16], who reported reduced HPC numbers in the BM of patients with CAD.
Whereas we observed a functional impairment of BM-derived progenitor cells in IHD, we also observed elevated circulating EPC numbers in these patients. This finding implies an active, possibly compensatory, recruitment of EPC from the BM into the circulation in the setting of ischemia, in order to obtain local neovascularization of ischemic tissue. In our study, higher numbers of circulating EPC correlated with higher CXCR4 expression on BM-MNC, suggesting that EPC recruitment into the circulation is mediated, at least partly, by SDF-1α.
In literature, conflicting results in circulating EPC numbers in the setting of IHD and HF have been published. Vasa et al. [28] showed a decrease in CD34+KDR+ cells in the circulation of CAD patients (stable CAD, acute coronary syndrome, or MI) compared to healthy subjects, while Valgimigli et al. [29] demonstrated increased CD34+CD133+KDR+ numbers in PB of patients with congestive HF (from different etiologies), especially in the early phase of HF (NYHA I). These data emphasize that not only the heterogeneity in EPC phenotypes but also the differences in severity of HF can lead to variations in study outcome.
Underlying Mechanisms for BM-Derived Progenitor Cell Dysfunction in IHD
Multiple mechanisms could underlie the observed dysfunction of BM-derived progenitor cells in IHD. Identification of these targets could help to restore progenitor cell functions and improve outcome after autologous stem cell therapy.
Since TNFα has been identified as a cell-extrinsic suppressor of normal HPC activity in vivo [18], we explored increased inflammation as a potential trigger of BM dysfunction. Interestingly, the inflammatory cytokine levels (TNFα, IFNγ, and IL-6) were lower in BM compared to PB, suggesting that BM can be regarded as a separate compartment and is protected from systemic increases in circulating cytokines. As expected, IL-6 levels were increased in both circulation and BM of patients with ICM; however, these IL-6 elevations were not statistically significant in patients with non-ischemic HF, which might be attributed to a less depressed LVEF in this patient cohort.
Neither the levels of TNFα and IFNγ in the BM compartment nor their systemic levels differed between groups. A possible hypothesis for the lack of these differences in inflammatory markers could potentially be ascribed to the inherent immunosuppressive nature of the BM-derived progenitor cells. Not only MSC but also early myeloid progenitor cells have recently been identified as immunosuppressors by the induction of T cell proliferation and regulatory T cell development in vitro [30]. The underlying mechanisms for these immunomodulatory properties are not yet fully elucidated, but MSC-mediated immunosuppression appeared to be even induced by pro-inflammatory cytokines through the role play of chemokines and NO, suggesting a compensatory mechanism [31].
TNFR2 is known to act as life receptor stimulating proliferation and cell survival, particularly in lymphocytes [32]. In contrast, we documented a negative relation between TNFR2 and both myeloid and erythroid differentiation capacity of BM-MNC. Yet, data by Schling et al. clearly demonstrate that there is no general principle for the regulated expression of TNFα and its receptors during the conversion of precursors into a more mature cell phenotype [33]. In this regard, experimental studies with primary cultures from WT and TNFR2−/− mice have demonstrated accelerated differentiation from bone marrow precursor cells into dendritic cells and osteoclasts [34, 35].
Based on these findings, as well as on the missing correlations between the inflammatory markers and the progenitor cell functionality in our study population, it is rather unlikely that inflammation is a major underlying mechanism for the observed BM dysfunction in IHD. In hematological disorders, immunosuppressive therapy has even been shown to beneficially affect the BM function. For example, in patients with aplastic anemia, immunosuppressive therapy with antithymocyte globulin and cyclosporine A results in hematologic recovery of the BM, despite the initial defect in progenitor cell numbers [36]. Hence, we should not ignore the suppressing role of inflammation on the progenitor cell function, but our data suggest that in the setting of IHD other more determining mechanisms are at play, whether or not stimulated by inflammation.
Since the intrinsic cellular dysfunction in BM was not observed in the setting of HF, future experiments could focus on ischemia-related pathways as underlying mechanism for BM dysfunction. For example, diabetes-induced microangiopathy in BM is responsible for a reduced perfusion and nutrition, as well as increased oxidative stress and reduced nitric oxide bioavailability, thereby hampering the progenitor cell function and HPC/EPC mobilization in ischemia models in vivo [37]. The suppressing effect of microvascular disease on BM function could be further extrapolated to IHD, although, the extent of microvascular disease in the BM niche in IHD has to be further explored.
Accelerated senescence of BM-derived progenitor cells could also be a potential underlying mechanism since IHD has been associated with telomere shortening of BM-MNC [38].
Implications for Autologous Stem Cell Therapy
Impaired progenitor cell function compromises the outcome of autologous stem cell therapy. The TOPCARE-CHD study demonstrated the clinical relevance of this impairment: administration of progenitor cells with a reduced function in vitro is inferior to administration of BM-MNC with a preserved function on patient survival and LVEF improvement [8]. A detailed analysis performed by Cogle et al. on the stem cell product that was administered in patients with acute and chronic IHD and left ventricular dysfunction showed a decrement in LVEF with decreasing percentages of CD34+ of the administered BM-MNC [13]. Based on our results, it appears that the poor outcome of autologous stem cell therapy in IHD might be a consequence of their reduced ability to differentiate.
In order to identify suitable therapeutic targets to improve efficacy of autologous stem cell therapy, we should first collect more insight in the underlying mechanisms of this observed progenitor cell dysfunction in IHD patients. Secondly, these specific pathways could be targeted to reverse the functional outcome. In this regard, modulation of cellular microRNA is particularly promising and proven successful in augmenting the progenitor cell function by means of paracrine activity, cell survival, and cardiomyogenic differentiation capacity, with direct beneficial impact on cardiac and/or vascular regeneration [39].
Additional Determinants of the Progenitor Cell Function
Not only the presence of IHD but also specific demographic characteristics of the study population are well-known relevant determinants on the BM-derived progenitor cell function.
For example, evidence has been collected for age-dependent deterioration of the proliferative capacity of BM-derived progenitor cells and in general the hematopoietic compartment [24]. In healthy subjects and/or CAD patients, age has been associated with impaired in vivo neovascularization, in vitro migration, and myeloid differentiation capacity of BM-MNC [14, 40]. This age effect was also observed in our study population: a negative relation was found with both GM-CFU and BFU-E numbers; however, this bias was limited since our study cohorts did not differ with respect to age. Additionally, in the regression model, analyses were adjusted for age.
Moreover, also medication appears to have its influence on the progenitor cell function and numbers. Statins have shown to stimulate BM-derived EPC survival, differentiation and function, as well as mobilization into the circulation [41]. In addition, non-selective beta-blockers appear to increase HPC growth and proliferation in the BM, although they play a suppressing role on the HPC mobilization [42]. In contrast, ACE inhibitors stimulate CD34+ cell recruitment into the circulation and towards the place of injury [43].
Additionally, concomitant chronic kidney disease is a well-known cause of anemia in HF patients and therefore assigned as exclusion criterion in our study [44]. Also patients with diabetes were withdrawn: type I and II diabetes have not only been associated with a reduced number of EPC but also with a reduced VEGF-/SDF-1α-induced migration capacity and proliferation [24]. Moreover, in the setting of cardiovascular disease, the co-presence of diabetes impairs CD34+ mobilization from the BM [25].
Limitations
Differences in BM-derived progenitor cell function between various underlying etiologies for cardiovascular diseases were evident in our study; yet, our results need to be further confirmed in larger trials.
Conclusions
The differentiation capacity of BM-derived progenitor cells is reduced in patients with IHD, which may hamper the clinical efficacy of autologous stem cell therapy. This functional impairment worsens with increasing complexity of coronary lesions but is not observed in the setting of non-ischemic cardiomyopathy. These findings suggest that IHD is an important determinant of progenitor cell function in the BM compartment. The observed myelosuppression in IHD is not driven by low-grade systemic inflammation, suggesting that other mechanisms are at play. Future studies should aim to elucidate the exact mechanisms for reduced BM-progenitor cell function in IHD in order to increase the success rate of BM cell therapy in this patient population.
Abbreviations
- BFU-E:
-
Erythroid burst-forming units
- BM:
-
Bone marrow
- CAD:
-
Coronary artery disease
- EPC:
-
Endothelial progenitor cell
- GM-CFU:
-
Granulocyte-macrophage colony-forming units
- HF:
-
Heart failure
- HPC:
-
Hematopoietic progenitor cell
- ICM:
-
Ischemic cardiomyopathy
- IHD:
-
Ischemic heart disease
- MNC:
-
Mononuclear cells
- LVEF:
-
Left ventricular ejection fraction
- PB:
-
Peripheral blood
References
Orlic, D., Kajstura, J., Chimenti, S., Jakoniuk, I., et al. (2001). Bone marrow cells regenerate infarcted myocardium. Nature, 410(6829), 701–705.
Lipinski, M. J., Biondi-Zoccai, G. G., Abbate, A., Khianey, R., et al. (2007). Impact of intracoronary cell therapy on left ventricular function in the setting of acute myocardial infarction: a collaborative systematic review and meta-analysis of controlled clinical trials. Journal of the American College of Cardiology, 50(18), 1761–1767.
Delewi, R., Hirsch, A., Tijssen, J. G., Schachinger, V., et al. (2014). Impact of intracoronary bone marrow cell therapy on left ventricular function in the setting of ST-segment elevation myocardial infarction: a collaborative meta-analysis. European Heart Journal, 35(15), 989–998.
Tongers, J., Losordo, D. W., & Landmesser, U. (2011). Stem and progenitor cell-based therapy in ischaemic heart disease: promise, uncertainties, and challenges. European Heart Journal, 32(10), 1197–1206.
Fisher, S. A., Doree, C., Mathur, A., & Martin-Rendon, E. (2015). Meta-analysis of cell therapy trials for patients with heart failure—an update. Circulation Research.
Afzal, M. R., Samanta, A., Shah, Z. I., Jeevanantham, V., et al. (2015). Adult bone marrow cell therapy for ischemic heart disease: evidence and insights from randomized controlled trials. Circulation Research, 117(6), 558–575.
Perin, E. C., Willerson, J. T., Pepine, C. J., Henry, T. D., et al. (2012). Effect of transendocardial delivery of autologous bone marrow mononuclear cells on functional capacity, left ventricular function, and perfusion in chronic heart failure: the FOCUS-CCTRN trial. JAMA, 307(16), 1717–1726.
Assmus, B., Fischer-Rasokat, U., Honold, J., Seeger, F. H., et al. (2007). Transcoronary transplantation of functionally competent BMCs is associated with a decrease in natriuretic peptide serum levels and improved survival of patients with chronic postinfarction heart failure: results of the TOPCARE-CHD Registry. Circulation Research, 100(8), 1234–1241.
Sant’Anna, R. T., Fracasso, J., Valle, F. H., Castro, I., et al. (2014). Direct intramyocardial transthoracic transplantation of bone marrow mononuclear cells for non-ischemic dilated cardiomyopathy: INTRACELL, a prospective randomized controlled trial. Revista Brasileira de Cirurgia Cardiovascular, 29(3), 437–447.
Hamshere, S., Arnous, S., Choudhury, T., Choudry, F., et al. (2015). Randomized trial of combination cytokine and adult autologous bone marrow progenitor cell administration in patients with non-ischaemic dilated cardiomyopathy: the REGENERATE-DCM clinical trial. European Heart Journal.
Westenbrink, B. D., Voors, A. A., de Boer, R. A., Schuringa, J. J., et al. (2010). Bone marrow dysfunction in chronic heart failure patients. European Journal of Heart Failure, 12(7), 676–684.
Kissel, C. K., Lehmann, R., Assmus, B., Aicher, A., et al. (2007). Selective functional exhaustion of hematopoietic progenitor cells in the bone marrow of patients with postinfarction heart failure. Journal of the American College of Cardiology, 49(24), 2341–2349.
Cogle, C. R., Wise, E., Meacham, A. M., Zierold, C., et al. (2014). Detailed analysis of bone marrow from patients with ischemic heart disease and left ventricular dysfunction: BM CD34, CD11b, and clonogenic capacity as biomarkers for clinical outcomes. Circulation Research, 115(10), 867–874.
Heeschen, C., Lehmann, R., Honold, J., Assmus, B., et al. (2004). Profoundly reduced neovascularization capacity of bone marrow mononuclear cells derived from patients with chronic ischemic heart disease. Circulation, 109(13), 1615–1622.
Jakob, P., Doerries, C., Briand, S., Mocharla, P., et al. (2012). Loss of angiomiR-126 and 130a in angiogenic early outgrowth cells from patients with chronic heart failure: role for impaired in vivo neovascularization and cardiac repair capacity. Circulation, 126(25), 2962–2975.
Liguori, A., Fiorito, C., Balestrieri, M. L., Crimi, E., et al. (2008). Functional impairment of hematopoietic progenitor cells in patients with coronary heart disease. European Journal of Haematology, 80(3), 258–264.
Lin, C. P., Lin, F. Y., Huang, P. H., Chen, Y. L., et al. (2013). Endothelial progenitor cell dysfunction in cardiovascular diseases: role of reactive oxygen species and inflammation. BioMed Research International, 2013, 845037.
Pronk, C. J., Veiby, O. P., Bryder, D., & Jacobsen, S. E. (2011). Tumor necrosis factor restricts hematopoietic stem cell activity in mice: involvement of two distinct receptors. The Journal of Experimental Medicine, 208(8), 1563–1570.
Sianos, G., Morel, M. A., Kappetein, A. P., Morice, M. C., et al. (2005). The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention, 1(2), 219–227.
D’Agostino, R. B., Sr., Vasan, R. S., Pencina, M. J., Wolf, P. A., et al. (2008). General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation, 117(6), 743–753.
Nollet, E., Van Craenenbroeck, E. M., Martinet, W., Rodrigus, I., et al. (2015). Bone matrix vesicle-bound alkaline phosphatase for the assessment of peripheral blood admixture to human bone marrow aspirates. Clinica Chimica Acta, 446, 253–260.
Gajkowska, A., Oldak, T., Jastrzewska, M., Machaj, E. K., et al. (2006). Flow cytometric enumeration of CD34+ hematopoietic stem and progenitor cells in leukapheresis product and bone marrow for clinical transplantation: a comparison of three methods. Folia Histochemica et Cytobiologica, 44(1), 53–60.
Van Craenenbroeck, E. M., Van Craenenbroeck, A. H., van Ierssel, S., Bruyndonckx, L., et al. (2013). Quantification of circulating CD34+/KDR+/CD45dim endothelial progenitor cells: analytical considerations. International Journal of Cardiology, 167(5), 1688–1695.
Dimmeler, S., & Leri, A. (2008). Aging and disease as modifiers of efficacy of cell therapy. Circulation Research, 102(11), 1319–1330.
Fadini, G. P., & Avogaro, A. (2013). Diabetes impairs mobilization of stem cells for the treatment of cardiovascular disease: a meta-regression analysis. International Journal of Cardiology, 168(2), 892–897.
Bozdag-Turan, I., Turan, R. G., Paranskaya, L., Arsoy, N. S., et al. (2012). Correlation between the functional impairment of bone marrow-derived circulating progenitor cells and the extend of coronary artery disease. Journal of Translational Medicine, 10, 143.
Coats, A. J. (2001). Heart failure: what causes the symptoms of heart failure? Heart, 86(5), 574–578.
Vasa, M., Fichtlscherer, S., Aicher, A., Adler, K., et al. (2001). Number and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery disease. Circulation Research, 89(1), E1–E7.
Valgimigli, M., Rigolin, G. M., Fucili, A., Porta, M. D., et al. (2004). CD34+ and endothelial progenitor cells in patients with various degrees of congestive heart failure. Circulation, 110(10), 1209–1212.
Pu, S., Qin, B., He, H., Zhan, J., et al. (2016). Identification of early myeloid progenitors as immunosuppressive cells. Scientific Reports, 6, 23115.
Ren, G., Zhang, L., Zhao, X., Xu, G., et al. (2008). Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell, 2(2), 141–150.
Chen, X., & Oppenheim, J. J. (2011). Contrasting effects of TNF and anti-TNF on the activation of effector T cells and regulatory T cells in autoimmunity. FEBS Letters, 585(23), 3611–3618.
Schling, P., Rudolph, C., Heimerl, S., Fruth, S., et al. (2006). Expression of tumor necrosis factor alpha and its receptors during cellular differentiation. Cytokine, 33(5), 239–245.
Polz, J., Remke, A., Weber, S., Schmidt, D., et al. (2014). Myeloid suppressor cells require membrane TNFR2 expression for suppressive activity. Immunity, Inflammation and Disease, 2(2), 121–130.
Abu-Amer, Y., Erdmann, J., Alexopoulou, L., Kollias, G., et al. (2000). Tumor necrosis factor receptors types 1 and 2 differentially regulate osteoclastogenesis. The Journal of Biological Chemistry, 275(35), 27307–27310.
Maciejewski, J. P., Kim, S., Sloand, E., Selleri, C., et al. (2000). Sustained long-term hematologic recovery despite a marked quantitative defect in the stem cell compartment of patients with aplastic anemia after immunosuppressive therapy. American Journal of Hematology, 65(2), 123–131.
Mangialardi, G., Katare, R., Oikawa, A., Meloni, M., et al. (2013). Diabetes causes bone marrow endothelial barrier dysfunction by activation of the RhoA-Rho-associated kinase signaling pathway. Arteriosclerosis, Thrombosis, and Vascular Biology, 33(3), 555–564.
Spyridopoulos, I., Erben, Y., Brummendorf, T. H., Haendeler, J., et al. (2008). Telomere gap between granulocytes and lymphocytes is a determinant for hematopoetic progenitor cell impairment in patients with previous myocardial infarction. Arteriosclerosis, Thrombosis, and Vascular Biology, 28(5), 968–974.
Nollet, E., Hoymans, V. Y., Van Craenenbroeck, A. H., Vrints, C. J., et al. (2016). Improving stem cell therapy in cardiovascular diseases: the potential role of microRNA. The American Journal of Physiology - Heart and Circulatory Physiology, ajpheart 00239 02016.
Schundeln, M. M., Walde, G., Basu, O., Havers, W., et al. (2014). Quantification of nucleated cells, CD34-positive cells and CFU-GM colonies in single bone marrow samples and bone marrow harvests derived from healthy children. Pediatric Hematology and Oncology, 31(4), 340–348.
Llevadot, J., Murasawa, S., Kureishi, Y., Uchida, S., et al. (2001). HMG-CoA reductase inhibitor mobilizes bone marrow-derived endothelial progenitor cells. The Journal of Clinical Investigation, 108(3), 399–405.
Beiermeister, K. A., Keck, B. M., Sifri, Z. C., ElHassan, I. O., et al. (2010). Hematopoietic progenitor cell mobilization is mediated through beta-2 and beta-3 receptors after injury. The Journal of Trauma, 69(2), 338–343.
Cangiano, E., Marchesini, J., Campo, G., Francolini, G., et al. (2011). ACE inhibition modulates endothelial apoptosis and renewal via endothelial progenitor cells in patients with acute coronary syndromes. American Journal of Cardiovascular Drugs, 11(3), 189–198.
Babitt, J. L., & Lin, H. Y. (2012). Mechanisms of anemia in CKD. Journal of the American Society of Nephrology, 23(10), 1631–1634.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study complied with the Helsinki Declaration and was approved by the local ethics committee. Informed consent was obtained from all subjects.
Funding
The work was supported by a research grant from the Fund for Scientific Research (FWO-Flanders, G060321N). EN is supported by a research grant from the University of Antwerp. EVC is supported by FWO-Flanders as senior clinical investigator.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Associate Editor Lorrie Kirshenbaum oversaw the review of this article
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Detailed Methods
(PDF 99 kb)
Supplementary Tables
(PDF 79.7 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nollet, E., Hoymans, V.Y., Rodrigus, I.R. et al. Bone Marrow-Derived Progenitor Cells Are Functionally Impaired in Ischemic Heart Disease. J. of Cardiovasc. Trans. Res. 9, 266–278 (2016). https://doi.org/10.1007/s12265-016-9707-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-016-9707-z