Abstract
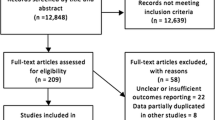
Long-term outcomes after open cholecystectomy are largely unknown. We aimed to investigate long-term mortality rate and incidence of intestinal obstruction after open cholecystectomy. Reporting of this systematic review and meta-analysis was according to the PRISMA 2020 guideline. A protocol was registered at PROSPERO (CRD42020178906). We searched the databases PubMed, Embase, and Cochrane CENTRAL in February 2022 for studies on long-term complications with n > 40 and follow-up ≥ 6 months. Outcomes included mortality and intestinal obstruction. Meta-analyses were conducted, and results were presented in forest plots. Risk of bias was assessed with the Newcastle–Ottawa Scale or Cochrane risk-of-bias tool 1. We included 21 studies. Long-term mortality after open cholecystectomy was reported in 17 studies including 125,222 patients, and it ranged from 0–35%. Follow-up ranged from six months to ten years. Meta-analysis estimated a long-term mortality rate of 9.2% (95% CI 6.8–11.6). One study with 90 patients reported on mini-laparotomy and none died during the 12 months follow-up. Three studies with 66,257 patients reported on intestinal obstruction after open cholecystectomy with an incidence ranging from 0.5% to 2.6%. Follow-up ranged from 36 to 67 months. Meta-analysis estimated a long-term rate of intestinal obstruction of 2.0% (95% CI 1.0–3.0). After a follow-up of six months to ten years, long-term mortality was 9.2%, and long-term incidence of intestinal obstruction was 2% up to 67 months after open cholecystectomy.



Similar content being viewed by others
Data Availability
Data extracted from the included studies can be shared upon request.
References
Lammert F, Acalovschi M, Ercolani G et al (2016) EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol 65:146–181
Talseth A, Lydersen S, Skjedlestad FE et al (2014) Trends in cholecystectomy rates in a defined population during and after the period of transition from open to laparoscopic surgery. Scand J Gastroenterol 49:92–98
Silverstein A, Costas-Chavarri A, Gakwaya MR et al (2017) Laparoscopic versus open cholecystectomy: a cost–effectiveness analysis at Rwanda Military Hospital. World J Surg 41:1225–1233
Keus F, Gooszen HG, Van Laarhoven CJHM (2009) Systematic review: open, small-incision or laparoscopic cholecystectomy for symptomatic cholecystolithiasis. Aliment Pharmacol Ther 29:359–578
Coccolini F, Catena F, Pisano M et al (2015) Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg 18:196–204
Jensen SA-MS, Fonnes S, Gram-Hanssen A et al (2022) Long-term mortality and intestinal obstruction after laparoscopic cholecystectomy: a systematic review and meta-analysis. Int J Surg 105:106841
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Jensen SA-MS, Fonnes S, Gram-Hanssen A, et al. Long-term complications after cholecystectomy including incisional hernia, intestinal bowel obstruction, and death: systematic reviews. PROSPERO. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=178906 (last accessed Oktober 19, 2023).
Greenhalgh T, Peacock R (2005) Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 331:1064–1065
Ouzzani M, Hammady H, Fedorowicz Z et al (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5:210
Higgins J, Savović J, Page M et al (2023) Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins J, Thomas J, Chandler J, et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane. Available from www.training.cochrane.org/handbook
Wells G, Shea B, O’Connell D et al (2011) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (last accessed Oktober 19, 2023)
Furuya-Kanamori L, Barendregt JJ, Doi SAR (2018) A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc 16:195–203
Doi SA (2018) Rendering the Doi plot properly in meta-analysis. Int J Evid Based Healthc 16:242–243
Wallace BC, Schmid CH, Lau J et al (2009) Meta-Analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol 9:80
Migliavaca CB, Stein C, Colpani V et al (2022) Meta-analysis of prevalence: I2 statistic and how to deal with heterogeneity. Res Synth Methods 13:363–367
Guyatt GH, Oxman AD, Vist GE et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926
Akl E, Mustafa R, Santesso N, et al (2003) GRADE Handbook. https://gdt.gradepro.org/app/handbook/handbook.html#h.svwngs6pm0f2 (last accessed October 19, 2023)
Deeks JJ, Higgins JPT, Altman DG (2023) Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023) Cochrane. Available from www.training.cochrane.org/handbook
Hammarström LE, Holmin T, Stridbeck H et al (1995) Long-term follow-up of a prospective randomized study of endoscopic versus surgical treatment of bile duct calculi in patients with gallbladder in situ. Br J Surg 82:1516–1521
Zitser YG, Simchen E, Ferderber N et al (1997) A trend for reduced 15-day wound infection and 6 months’ mortality in laparoscopic relative to open cholecystectomy: the Israeli study of surgical infections. Clin Perform Qual Health Care 5:116–122
Kelly TR (1974) Gallstone pancreatitis. Arch Surg 109:294–297
Ros E, Zambon D (1987) Postcholecystectomy symptoms. A prospective study of gallstone patients before and two years after surgery. Gut 28:1500–1504
Kong J, Shahait A, Girten K et al (2021) Recent trends in cholecystectomy in US veterans. Surg Endosc 35:5558–5566
Catena F, Melotti RM, Louis D et al (2017) Cholecystectomy in Emilia-Romagna region (Italy): a retrospective cohort study based on a large administrative database. Ann Ital Chir 88:215–221
Sinha S, Hofman D, Stoker DL et al (2013) Epidemiological study of provision of cholecystectomy in England from 2000 to 2009: retrospective analysis of hospital episode statistics. Surg Endosc 27:162–175
Rana HN, Hasan F, Tahir M et al (2011) Mini cholecystectomy through a 5cm subcostal incision experience at NSSSH Lahore. PJMHS 5:610–612
Rosenmüller M, Haapamäki MM, Nordin P et al (2007) Cholecystectomy in Sweden 2000–2003: a nationwide study on procedures, patient characteristics, and mortality. BMC Gastroenterol 7:35
Andersen TF, Brønnum-Hansen H, Jørgensen T et al (1995) Survival until 6 years after cholecystectomy: female population of Denmark, 1977–1983. World J Surg 19:609–615
Rogers AL, Farha GJ, Beamer RL et al (1985) Incidence and associated mortality of retained common bile duct stones. Am J Surg 150:690–693
Frey CF (1969) The operative treatment of pancreatitis. Arch Surg 98:406–417
Gilliland TM, Traverso LW (1990) Modern standards for comparison of cholecystectomy with alternative treatments for symptomatic cholelithiasis with emphasis on long term relief of symptoms. Surg Gynecol Obstet 170:39–44
Mühe E (1992) Long-term follow-up after laparoscopic cholecystectomy. Endoscopy 24:754–758
De la Serna S, Ruano A, Pérez-Jiménez A et al (2019) Safety and feasibility of cholecystectomy in octogenarians. Analysis of a single center series of 316 patients. HPB 21:1570–1576
Konsten J, Gouma DJ, von Meyenfeldt MF et al (1993) Long-term follow-up after open cholecystectomy. Br J Surg 80:100–102
Khuri SF, Henderson WG, DePalma RG et al (2005) Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 242:326–343
Linos DA, Adson MA (1983) Gallstone pancreatitis. Int Surg 68:153–156
Angenete E, Jacobsson A, Gellerstedt M et al (2012) Effect of laparoscopy on the risk of small-bowel obstruction: a population-based register study. Arch Surg 147:359–365
Udelsman BV, Chang DC, Parina R et al (2020) Population level analysis of adhesive small bowel obstruction. Ann Surg 271:898–905
Zbar RIS, Crede WB, Mckhann CF et al (1993) The postoperative incidence of small bowel obstruction following standard, open appendectomy and cholecystectomy: a six-year retrospective cohort study at Yale-New Haven Hospital. Conn Med 57:123–127
Jensen SA-MS, Fonnes S, Gram-Hanssen A et al (2021) Low long-term incidence of incisional hernia after cholecystectomy: a systematic review with meta-analysis. Surgery 169:1268–1277
Ellis H, Moran BJ, Thompson JN et al (1999) Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet 353:1476–1480
Barmparas G, Branco BC, Schnüriger B et al (2010) The incidence and risk factors of post-laparotomy adhesive small bowel obstruction. J Gastrointest Surg 14:1619–1628
Maclean AR, Cohen Z, Macrae HM et al (2002) Risk of small bowel obstruction after the ileal pouch-anal anastomosis. Ann Surg 235:200–206
Benlice C, Stocchi L, Costedio M et al (2015) Laparoscopic IPAA is not associated with decreased rates of incisional hernia and small-bowel obstruction when compared with open technique: long-term follow-up of a case-matched study. Dis Colon Rectum 58:314–320
Acknowledgements
We thank Kristoffer Andresen for his contribution to the conceptualization of the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All listed authors meet the ICMJE authorship criteria.
SASJ: Conceptualization; acquisition, analysis, and interpretation of the data; drafting the original draft; final approval; and agreed to be accountable for all aspects of the work.
SF: Conceptualization; interpretation of the data; critical revision of manuscript; final approval; and agreed to be accountable for all aspects of the work.
AG: Conceptualization; interpretation of the data; critical revision of manuscript; final approval; and agreed to be accountable for all aspects of the work.
JR: Conceptualization; interpretation of the data; critical revision of manuscript; final approval; and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethical Approval
Not relevant.
Conflicts of Interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jensen, S.AM.S., Fonnes, S., Gram-Hanssen, A. et al. Long-term Mortality and Intestinal Obstruction after Open Cholecystectomy: A Systematic Review and Meta-analysis. Indian J Surg (2024). https://doi.org/10.1007/s12262-024-04054-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12262-024-04054-5