Abstract
Spigelian hernia (SH) represents less than 1% of all hernias and about 0,1% of abdominal wall hernias. Although it is a very rare hernia, it has a considerably high risk of strangulation. The aim of this work is to propose the open approach based on local anesthesia on a Day Surgery regimen as a safe treatment for Spigelian Hernia surgery. We report a series of 17 clinical cases (9 men and 8 women, between 40 and 80 years old) who underwent SH open repair on a Day Surgery basis between 2004 and 2021 in our University Hospital. In our single-center case series, no early postoperative complications occurred, except for a bulky seroma of about 800 cc. No prosthesis or surgical wound infections occurred and no recurrences were observed in the early postoperative period. Looking at our experience and the literature, Spigelian hernia repair under local anesthesia on a Day Surgery regimen, using a pre-peritoneal polypropylene mesh, could be proposed as a safe and “real minimally invasive” approach in elective settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spigelian Hernia (SH), also known as “semilunar hernia” or “spontaneous lateral ventral hernia” [1], is an infrequent ventral hernia, representing about 0,1% of all abdominal wall hernias [1]. It can be considered a multifactorial pathology whose main associated risk factors are advanced age [2], constitutional factors [3], chronic increase in intra-abdominal pressure [4], diabetes [5] or connective tissue diseases [2]. There is no consensus about the optimal surgical approach: an open approach is generally preferred, although nowadays many authors are experimenting laparoscopic [6] and robotic surgery [7] for the treatment of SH. The aim of this work is to propose an open approach under local anesthesia on a Day Surgery regimen as a safe “real minimally invasive” treatment for Spigelian Hernia surgery.
Patients and Methods
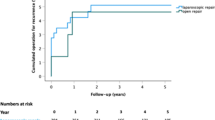
Here we report a series of 17 clinical cases (9 men and 8 women, between 40 and 80 years old) who underwent SH open repair on a Day Surgery basis between 2004 and 2021 in our University Hospital. Patients’ clinical features and instrumental exams are summarized in Table 1. All recruited patients gave their informed consent to use anonymized clinical data. Since 2001 this consent is already part of the surgical informed consent of our Clinic. This is a retrospective observational study, as a retrospective evaluation of a prospectively recorded data of our database starting from 2004 has been used. The Institutional Ethics Committee confirmed that no ethical approval was required. Among our patients, one mentioned a recent laparotomy for emergency surgery (urgent bilateral adnexectomy due to an hemoperitoneum) and a recurrent suprapubic incisional hernia; another patient mentioned previous cholecystectomy and prostatectomy. Two giant hernias with loss of abdominal domain were observed in two cases (12 × 10 cm and 10 × 9 cm respectively), and other two partially reducible hernias. Diagnosis was made based on anamnesis, clinical examination (Fig. 1a) and ultrasound; only in one case, additional CT and MR exams were needed to confirm the diagnosis (Fig. 1b). Surgical features, types of hospitalization and types of access to surgery are depicted in Table 2. Our surgical management of Spigelian hernia repair is conducted using both Day Surgery and local anesthesia selection criteria like the ones already published for incisional hernia repair [8], and a local anesthesia solution like the one already published for other abdominal wall hernias [9]. We borrowed the local anesthesia approach from the already described technique for incisional hernia repair [9]. Specifically, we used an infiltration of soft tissues until the obliquus externus fascia and an open troncular anesthesiologic block of ileo-inguinal and ileo-hypogastric nerves, with an additional perisaccular local anesthesia infiltration during the second part of the surgery, after opening the obliquus externus fascia until the hernia defect in the preperitoneal space along the Spigelian line. Our surgical technique contemplates opening the aponeurosis of the external oblique muscle in its pararectal side, isolating the hernial sac and placing a pre-peritoneal polypropylene prosthesis fixed by polypropylene stiches. Both mesh and plug were employed in 12 operations: along with the mesh, in 4 cases a double plug was used in order to repair the hernia and in one case 3 plugs were needed, based on a larger defect size. A mesh without any plug was used in 5 cases (29,4%). A double-layered polypropylene mesh was used for hernia repair in one case. Long-term follow-up was conducted by clinical and ultrasound examination and lasted between 12 and 180 months, with an average of 89 months.
Results
All the patients showed regular postoperative course: no early postoperative complications occurred, except for a bulky seroma of about 800 cc (Grade IIIa complication in Clavien-Dindo classification [10]) in one case (0,05%); it was drained two times on an outpatient basis and healed in 3 months. No prosthesis or surgical wound infections occurred. No recurrences were observed in the early postoperative period. All the patients were able to get back to their daily activities the day after discharge. No discomfort in the surgical site was mentioned by any of the patients. No differences between the outcomes of surgical SH repair only with a mesh and SH repair with mesh and plugs were detected in our follow-up.
Discussion
Spigelian hernia was named after Adriaan Van Den Spieghel, a Belgian anatomist and botanist [11] who described the anatomical limits of the semilunar line for the first time in 1645 [12]. Nevertheless, it was only in 1764 that Joseph T. Klinkosch [12] described this hernia as a clinical entity associated with this anatomical region [13] and gave it a definitive nosologic and topographical location by calling it "Spigelian hernia" [14]. Spigelian hernia can be subcutaneous [15] or intraparietal (the majority) [16]. It can also be secondary to trauma or previous surgery: in fact, up to 50% of Spigelian hernias occur in patients with a positive anamnesis for previous operations of the anterior abdominal wall [17]. Typically, it is a small-sized hernia [18], whose diagnosis is difficult due to the lack of specific clinical manifestations [19]. Surgical treatment is very often necessary due to its high risk of strangulation [20]. Even though it is considered a very rare hernia, it has a decidedly high risk of strangulation that reaches approximately 20–30% [20]. Its incidence seems to be slightly higher in women (1,18:1) [21], especially in the fifth and sixth decade of life [22]. It is generally a left-sided unilateral hernia [1] located along the semilunar fascia, a connective tissue area between the rectus abdominis muscle medially and the semilunar line laterally [3, 23]. Hernia content is very often made up of preperitoneal fat or peritoneal sac but, occasionally, various visceral organs can herniate as well [24]. Currently, surgical repair techniques for SH can be basically classified into two broad categories: open and minimally invasive repairs. As already stated, there is no consensus about which one is the best approach; it can depend on the experience of the surgeon [25], the clinical conditions of the patient or the characteristics of the hernia. Anyhow, following EHS and AHS Guidelines recommendations, we adopted open prosthetic repair [25]. Minimally invasive surgery is also accepted from the above-mentioned guidelines, but it is generally reserved to non-palpable lumps [25]; on the contrary, some Authors reserve it for selected cases with large hernial defects or when the aponeurotic tissues are noticeably weakened or atrophic [4]. Nowadays, robotic approach only counts a fair number of SH repair, so there are still limited data on its effectiveness and safety [2]. Open surgery contemplates the traditional herniorrhaphy used until the last years of the past century, such as the Mayo-Judd technique [26], first described by Mayo in 1901 and modified by Judd in 1912 [27], and the prosthetic hernia repair that has now almost completely replaced direct herniorraphy [25]. Prosthetic hernia repair is based on the placement of a prostheses with or without stitches fixation. Prosthetic hernia repair has a decidedly lower risk of recurrence and postoperative pain if compared to direct suture repair [28]. Most surgeons prefer open to laparoscopic surgery mainly because of its lower learning curve and its lower rate of intraoperative complications (e.g., vascular and visceral injuries) [29]. In addition, while minimally invasive surgery can only be performed under general anesthesia, open surgery makes it possible to use local or loco-regional (spinal or epidural) anesthesia, reducing hospitalization rate and guaranteeing an early mobilization, especially when local anesthesia is used. Nowadays, many surgeons perform hernia surgery -especially inguinal hernia repair- in a Day Surgery Regimen. The advantages are clear: not only the patient can come back earlier to a familiar environment, that means an early physical and psychological recovery, but also socio-health costs and waiting lists are reduced. This made hernia surgery under local anesthesia become an accepted Gold Standard of care [30]. In our experience, thanks to a standardized mixture of local anesthetics, we can treat every hernia in Day Surgery, included Spigelian hernia, achieving excellent results in terms of recurrence rate and intra-operative and early post-operative morbidity [9]. We use an extraperitoneal approach (Fig. 2), not opening abdominal cavity except for a restricted number of cases, for example when loss of viability of the intestinal loop involved is suspected. For all these reasons we call this method a “real minimally invasive” surgical method: the patient does not have all the problems related to general anesthesia and to pneumoperitoneum, so it is also easier to operate patients with cardiac or pulmonal comorbidities. Moreover, we do not open the peritoneum and we do not manipulate the bowels; the patient has only one scar, less pain and can be already discharged after three hours. In our single-center case series of SH repair from 2004 to 2021, Spigelian hernia repair was only performed with an open approach. Only 3 cases out of 17 were conducted under general anesthesia: those three patients came from the Emergency department of our hospital with a complicated SH hernia; given that the risk of opening the peritoneal sac and of bowel resection was considerably high, we decided not to perform surgery under local anesthesia in agreement with the team of anesthetists. Patients were discharged on the first post-operative day because bowel viability was maintained, so no bowel resection was needed. We also examined a series of small-scale studies conducted from 2001 to 2021 involving patients with Spigelian hernia operated on a Day Surgery regimen (Table 3). Overall, given the rarity of this hernia, the number of cases of Spigelian hernia treated on a one-day surgery regimen is still rather limited in recent years. In the examined literature, most of the patients (~ 31%) were discharged on the same day, especially those who underwent open surgery under local anesthesia. Only a few cases operated with a minimally invasive approach (laparoscopic or robotic) under general or spinal anesthesia, were discharged on the same day [7, 31], but most of them were instead discharged on the first postoperative day or after few days. Looking at the examined literature, comparing the number of recurrences and complications between open and minimally invasive SH repair, it is possible to state that there are no significative differences regarding the former, while postoperative mild and moderate complications appear to be more frequent with minimally invasive approaches. The limit of our Paper is that it is impossible to conduct a different group-treatment Trial, being it a single-center study and given the rarity of Spigelian Hernia. Therefore, our comparison was only based on different techniques of data in literature.
Conclusion
Looking at our experience and the literature, Spigelian hernia repair in elective settings could be easily conducted with both open and minimally invasive approaches. Anyway, our technique under local anesthesia on a Day Surgery regimen, using a pre-peritoneal polypropylene mesh, could be proposed as a valid and safe approach, except for a few cases treated in emergency conditions. Therefore, it seems to be the preferable surgical option and it could be considered as a “real minimally invasive” surgical method.
References
Cesaro E, Rocco C, Rosano N et al (2021) “Bulb-like” sign: Small bowel closed loop obstruction in incarcerated Spigelian hernia. Radiol Case Rep 16(3):520–523
Huttinger R, Sugumar K, Baltazar-Ford KS (2021) Spigelian Hernia. In: StatPearls [Internet]. Treasure island (FL): StatPearls Publishing
Patri G, Nostro IP, Maria A (2017) Ernie ventro-laterali della parete addominale-Revisione
Pinna A, Cossu ML, Paliogiannis P, Ginesu GC, Fancellu A, Porcu A (2016) Spigelian hernia. Ann Ital Chir 87(4):306–311
Duke B, Grozenski A, Kiel J (2021) Spigelian hernia secondary to blunt trauma. Curr Sports Med Rep 20(3):137–139
Takayama Y, Okada S, Nakatani K, Matsumoto R, Suganuma T, Rikiyama T (2021) The advantage of laparoscopic surgery in the treatment of Spigelian hernia: A report of two cases. Int J Surg Case Rep 82:105903
Jamshidian M, Stanek S, Sferra J, Jamil T (2018) Robotic repair of symptomatic Spigelian hernia: a series of three cases and surgical technique review. J Robot Surg 12:557–560
Donati M, Gandolfo L, Privitera A, Brancato G, Donati A (2008) Day hospital for incisional hernia repair: selection criteria. Acta Chir Belg 108(2):198–202
Donati M, Brancato G, Donati A (2010) Open incisional hernia repair under local anesthesia. Acta Chir Belg 110(1):45–50
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205
Ghosh SH, Sharma S, Biswas S, Chakraborty S (2014) Adriaan van den Spiegel (1578–1625): Anatomist, physician, and botanist. Clin Anat 27:952–957
Cinar H, Polat AK, Caglayan K, Ozbalci GS, Topgul HK, Polat C (2013) Spigelian hernia. Our experience and review of the literature. Ann Ital Chir 84:649–653
Vos DI, Scheltinga MRM (2004) Incidence and outcome of surgical repair of spigelian hernia. Br J Surg 91:640–644
Angelici AM, Nasti AG, Petrucciani N, Leonetti G, Palumbo P (2006) Spigelian hernia: a case report and review of the literature. G Chir 27(11/12):433–435
Azar SF, Jamadar DA, Wasnik AP, O’Rourke RW, Caoili EM, Gandikota G (2021) Clin Imaging 74:131–138
George C, Tauro LF, Dsouza C, Hegde BR, Kamath A, Rent E (2009) Spigelian hernia. J Clin Diagn Res 3:1437–1440
Foster D, Nagarajan S, Panait L (2015) Richter-type Spigelian hernia: A case report and review of the literature. Int J Surg Case Rep 6:160–162
Di Furia M, Romano L, Salvatorelli A et al (2019) Giant Spigelian Hernia presenting as small bowel obstruction: case report and review of literature. Int J Surg Case Rep 63:118–121
Taha A, Algethami NA, AlQurashi R, Alnemari AK (2021) Outcome of Orchidopexy in Spigelian Herni -undescended testis syndrome. Cureus 13(3):e13714
Rayman S, Yuori M, Jacob R et al (2021) Transabdominal Preperitoneal (TAPP) for the treatment of Spigelian hernias. JSLS 25(2):e2021.00024
Zachariah SK, Priya J (2011) Laparoscopic diagnosis of incarcerated “Spigelian Hernia”: report of a case and review of the literature. Case Rep Surg: 491802
Spinelli C, Strambi S, Pucci V, Liserre J, Spinelli G, Palombo C (2014) Spigelian hernia in a 14-Year-old girl: a case report and review of the literature. European J Pediatr Surg Rep 2(1):58–62
Halyk L, Pillay Y (2018) Laparoscopic herniorrhaphy of bilateral inguinal herniae and an incidental Spigelian hernia with intra corporeal suturing of the Spigelian hernia neck: A case report. Int J Surg Case Rep 49:58–63
Gurung R, Azna Ali A, Yee Lee F, Mra A, Hayati F (2021) A rare discovery of Spigelian-cryptorchidism syndrome in adult. Urol Case Rep 38:101687
Henriksen NA, Kaufmann R, on behalf of the European Hernia Society and the Americas Hernia Society et al (2020) EHS and AHS guidelines for treatment of primary ventral hernias in rare locations or special circumstances. BJS Open 4(2):342–353
Mayo WJ (1901) An operation of the radical cure of umbilical hernia. Ann Surg 34:276–280
Guhan VA (2016) Comparative study on various approaches in the surgical management of ventral hernia. Doctoral dissertation, Madras Medical College, Chennai
Scaini A, Olmi S, Croce E. Ernia di Spigelio. [PDF on Internet] Available from: http://www.doctor33.it/cont/download-center-files/15957/cap-ernia-spigelio-x19407allp1.pdf
Moreno-Egea A, Carrasco L, Girela E, Martin JG, Aguayo JL, Canteras M (2002) Open vs laparoscopic spigelian hernia repair: a prospective randomized trial. Arch Surg 137(11):1266–1268
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–165
Barnes TG, McFaul C, Abdelrazeq AS (2014) Laparoscopic transabdominal preperitoneal repair of Spigelian hernia—closure of the fascial defect is not necessary. J Laparoendosc Adv Surg Tech 24(2):66–71
Law TT, Ng KK, Ng L, Wong KY (2018) Elective laparoscopic totally extraperitoneal repair for Spigelian hernia: A case series of four patients. Asian J Endosc Surg 11(3):244–247
Zaragoza C, Peiró F, Bebek K et al (2001) Spiegelian hernia: ambulatory surgical treatment. Ambul Surg 9(3):127–129
Moreno-Egea A, Flores B, Girela E, Martín J, Aguayo J, Canteras M (2002) Spigelian hernia: bibliographical study and presentation of a series of 28 patients. Hernia 6(4):167–170
Campanelli G, Pettinari D, Nicolosi FM, Avesani EC (2005) Spigelian hernia. Hernia 9(1):3–5
Palanivelu C, MalladiVijaykumar KVJ, Rajan PS, Maheshkumaar GS, Rajapandian S (2006) Laparoscopic transabdominal preperitoneal repair of spigelian hernia. JSLS: J Soc Laparoendosc Surg 10(2):193
Zuvela M, Milicevic M, Galun D, Djuric-Stefanovic A, Bulajic P, Palibrk I (2013) Spigelian hernia as a day-case procedure. Hernia 17(4):483–486
Campanella AM, Licheri S, Barbarossa M et al (2015) Abdominal Wall Hernia-Spigelian hernia, anatomy, incidence, repair. Hernia 19:S215
Fernández-Moreno MC, Marti-Cunat E, Pou G, Ortega J (2018) Intraperitoneal Onlay mesh technique for Spigelian hernia in an outpatient and short-stay surgery unit: what’s new in intraperitoneal meshes? J Laparoendosc Adv Surg Tech 28(6):700–704
Donovan K, Denham M, Kuchta K et al (2021) Laparoscopic totally extraperitoneal and transabdominal preperitoneal approaches are equally effective for spigelian hernia repair. Surg Endosc 35(4):1827–1833
Zuvela M, Galun D, Bogdanovic A, Bidzic N, Zivanovic M (2021) Management of epigastric, umbilical, spigelian and small incisional hernia as day case procedure: results of long-term follow-up after open preperitoneal flat mesh technique. Hernia 25(4):1095–1101
Cui TYS, Law TT, Ng L, Wong KY (2021) Spigelian hernia: Our total extraperitoneal approach and a systematic review of the literature. Asian J Endoscopic Surg
Funding
Open access funding provided by Università degli Studi di Catania within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Conceptualization: Marcello Donati;
Methodology: Michela Zanatta;
Formal analysis and investigation: Michela Zanatta and Federica Marano;
Writing—original draft preparation: Michela Zanatta;
Writing—review and editing: Marcello Donati and Giovanna Brancato;
Funding acquisition: NA;
Resources: Michela Zanatta, Marcello Donati and Giovanna Brancato;
Supervision: Marcello Donati.
Corresponding author
Ethics declarations
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zanatta, M., Brancato, G., Marano, F. et al. Day Surgery for Spigelian Hernia Repair Under Local Anesthesia: A “Real Minimally Invasive” Surgical Approach. Indian J Surg 86, 408–413 (2024). https://doi.org/10.1007/s12262-023-03872-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-023-03872-3