Abstract
An aesthetically and functionally pleasing phalloplasty is most commonly performed by a free radial forearm flap. However, the problem with donor site morbidity on the forearm remains unsolved. The aim of this study was to evaluate if the use of a dermal template such as MatriDerm® on the donor site significantly decreases the incidence of complications based on the Clavien–Dindo classification, such as wound healing disorders and reoperation rate, and if it could shortens the duration of hospital stay. A case series analysis was conducted at our institution. A total of 21 patients divided into two groups undergoing the phallic construction after the Gottlieb and Levine design in a single center underwent the donor site defect coverage either by MatriDerm® and split-thickness skin graft from the thigh or by full-thickness skin graft from the groin area. The use of MatriDerm® and split-thickness skin graft showed to have a statistically significant impact on the rate of complications (p = 0.008). Complications that were treated conservatively as well as that require surgical revision were significantly lower in the MatriDerm® group than in the full-thickness skin graft group (p = 0.002). Complications occurred not only at the forearm but also at the groin, where the full-thickness skin graft was harvested. The large dimension of the free radial forearm flap used for phalloplasty resulted in a significant donor site morbidity, leading to wound healing disorders, reoperations, and extended length of hospital stay. Therefore, we consider the use of dermal templates such as MatriDerm® as worth the additional effort and costs in this patient collective.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
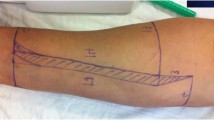
In most microsurgical centers, the free radial forearm flap represents the most common technique for penile reconstruction or transgender phalloplasty [1,2,3,4,5,6,7,8,9,10]. Previously, two different surgical techniques have been described: the first designed by Chang [11], published in 1984, and the second designed by Gottlieb and Levine [12], published in 1993. For both the techniques, the creation of a phallus required the harvesting of a large flap. Defect coverage of the donor site is most likely done by the use of split-thickness skin grafts [4, 13] or full-thickness skin grafts [4, 13,14,15]. Plastic surgeons know about the nuisance of wound healing disorders consisting in exposed tendons, reoperations, and extended duration of hospital stay [7, 16]. In the literature, the proposed solutions for optimizing the donor site after free radial forearm flap harvest include the use of endogenous tissue such as pedicled or free flaps that are either associated with great surgical effort [8] or simply too small to cover the entire donor site [4, 5, 9, 13, 17]. The solution proposed by several researchers are the use of dermal templates, such as Integra® or MatriDerm® [7, 17,18,19]. Initially, the dermal templates secure wound healing of the grafted skin on the bradytrophic tissue was employed in burn surgery, which minimizes the complications [20]. The dermal templates replace the dermis, where the application of an epidermal layer is needed and can be performed in a single-stage or two-stage procedure [7]. In our institution until 1993, the phalloplasty was done by adopting the design of Gottlieb and Levine [14]. There was an average donor site of 11 cm in width and 12 cm in length. The donor site reaches distally up to 2 to 3 cm from the palmar flexion crease (Fig. 1). Thus making the techniques applicable for minimizing the donor site like embedding of the exposed tendon into the adjacent muscle belly is impossible. At our institution, we used to perform the donor site defect coverage by full-thickness skin graft from the groin area. There are various reasons why the donor site defect coverage is done by full-thickness skin graft instead of split-thickness skin graft. The scar in the groin area is well hidden, and there is a request from patients to hide the donor site on the radial forearm by tattoo, which we considered safe after 1 year of surgery. In the split-thickness skin graft, the ink tends to smear and the artwork gets blurred. Due to the issues described above, we decided to switch to MatriDerm® and split-thickness skin graft from the thigh. Eventually, our institution compared the operative outcome on 21 patients with donor site coverage by a full-thickness skin graft from the groin area and the same number of consecutive patients with donor site defect coverage by single layered MatriDerm® dermal substitute plus split-thickness skin grafts from the thigh.
Patients and Methods
At our institution, a case series analysis of all patients having received defect coverage after harvesting the free radial forearm flap for the creation of a phallus by single-layered MatriDerm® and split-thickness skin grafts from the thigh (group A) between May 2016 and February 2018 was conducted. These 21 patients were compared to the same number of directly preceding patients receiving the defect coverage by full-thickness skin graft from the groin area (group B). All patients included in the study received a phalloplasty using Gottlieb and Levine’s technique [12, 14]. All patients were operated in an interdisciplinary two-team approach consisting of plastic surgeons and urologists. The short-term outcome of the donor site was analyzed with a special focus on wound healing disorders, reoperation rate, and duration of hospitalization (Fig. 2). The complications were classified by the Clavien–Dindo classification [21]. Ethics approval for the study was obtained from the ethical committee of the Hessian Medical Association. The methods of the study adhered to the CARE guidelines.
Statistical analysis was performed using the software SPSS (version 23.0) and R (version 3.3.2). Fisher’s exact test (χ2) test was used to detect the association between variables. The significance of the differences was tested with t test. A p value lower 0.05 was defined as statistically significant. A p value between 0.05 and 0.1 was defined to indicate a tendency towards a higher risk for complications.
Operative Technique
The phalloplasty procedure consists of a standardized procedure, as published previously [14]. The following description is about performing the defect coverage on the radial forearm. Preoperatively, Allen’s test was routinely performed in all patients to ensure adequate perfusion of the hand by the remaining ulnar artery. Elevation of the free radial forearm flap from the non-dominant forearm was performed as described previously by Gottlieb and Levine in 1993 [12, 14]. We adopted a careful dissection technique preserving the paratendon to provide a well-vascularized recipient bed for the skin graft or the dermal template to minimize the donor site morbidity. Defect coverage was either done by a full-thickness skin graft, harvested from the groin area, fatty gauze, following installation of the vacuum-assisted closure-therapy (VAC®) system; or by single-layered MatriDerm® plus split-thickness skin graft (0.2–0.3 mm thickness) from the thigh, fatty gauze, followed by the installation of a VAC® system. Installation of the VAC® system for graft fixation was performed identically in both groups. All patients were restrained from splint for 7 days after the operation. The VAC® system was removed from the bedside on the sixth postoperative day. Daily dressing was done for several days subsequently, until the skin graft showed not only adherence but stability as well. Once the skin graft was stable, the patients were instructed to perform scar massage and to apply a moisturizing ointment on a daily base. Patients were advised to wear a compression sleeve for 3 months postoperatively.
MatriDerm®
MatriDerm® (Skin and Health Care AG, Billerbeck, Germany) is a structurally intact matrix of bovine type I collagen with elastin which is used for dermal regeneration. The matrix serves as a support structure for the in growth of cells and vessels. Its elastin component improves the stability and elasticity of the regenerating tissue. As the healing process advances, fibroblast lays down the extracellular matrix, and the MatriDerm® resorbes it [20].
Results
A total of 42 patients undergoing phalloplasty by Gottlieb and Levine were included on accrual in the study. Thereof, 21 patients received donor site defect coverage by MatriDerm® and split-thickness skin graft (group A). The control group underwent full-thickness skin graft in the groin area (group B). Those 21 patients in group B preceded the patients from group A chronologically. In group A, the mean age of the patients was 33.4 years (range 18–51 years) with a mean BMI of 24.36 kg/m2 (range 19.1–32.04 kg/m2) and a mean duration of hospital stay of 20 days. Seven patients were active smokers at the time of surgery (33.3%). In group B, the mean age of the patients was 28.9 years (range 18–54 years) with a mean BMI of 25.8 kg/m2 (range 16.23–34.37 kg/m2) and a duration of hospital stay of 22 days. Eleven patients were active smokers at the time of surgery (52.4%). The patient groups did not differ statistically in terms of age (p=0.18) or proportion of smokers (p=0.49).
Complications were classified according to the Clavien–Dindo classification [21]. As defined by the authors, there is a graduation from zero to five [21]. Grade zero is assigned for the absence of complications. The definition of grade 1 is any deviation from the normal without any actions needed. Grade 2 is a complication that requires conservative medical therapy. A grade 3 complication requires surgical intervention. In our patient cohort, if there was no life-threating event, then it is defined as grade 4, and if the patient dies, it is grade 5 (Table 1). As Fig. 3 shows, group B is shown as an aesthetically unpleasant scar in the groin area, due to high tension on the scar.
Fisher’s exact test revealed a statistically significant difference between groups A and B for complications on the forearm based on the Clavien–Dindo classification compared to non-complication (0) and any (1–5) (p = 0.008) and between the non-complication as well as complications that can be treated conservatively and complications that require surgery (0–2 vs. 3–5; p=0.002). Especially in patients with low BMI, harvesting such large free radial forearm flaps from the forearm, as well as large full-thickness grafts from the groin, (partial) primary closure is under tension, often leading to subsequent wound dehiscence leaving behind an unpleasant scar (Fig. 3).
The average duration of hospital stay was 20 days in group A versus 22 days in group B (p=0.09). Statistical analysis showed no significant difference with respect to duration of hospital stay between groups A and B (p= 0.98). Power analysis revealed a needed sampling size of 51 patients per group to show a statistically significant difference. In both groups, we did not witness any neuroma of the superficial branch of the radial nerve.
Discussion
In most microsurgical centers, phalloplasty is most likely performed using the free radial forearm flap [1,2,3,4,5,6, 8,9,10, 14, 18, 22]. The donor site morbidity accompanied by a stigmatizing scar on the (non-dominant) forearm problem remains unsolved [4, 7,8,9, 14, 17]. The aim of this study was to investigate whether the use of the cost-intensive dermal layer reduced short-term complications and if reoperations would decrease or even become unnecessary and if the duration of hospital stay could be reduced. Our sample size allowed to clearly identify risk factors when performing donor site defect coverage of the radial forearm by full-thickness skin graft from the groin area. The use of a dermal template, such as MatriDerm®, allowed us to propose a solution for patients presenting to surgery with those identified risk factors.
The Clavien–Dindo classification allows a uniform description of complications if applied correctly, even a comparison between multiple centers. This study clearly showed that concerning short-term results, MatriDerm® had a significant impact on reducing wound healing disorders, accompanied by intensive dressing changes or even reoperations. From a physician’s point of view, any reoperation may represent a certain risk for the survival of the newly created phalloplasty, due to blood pressure alterations during anesthesia. In addition, reoperations present a high cost factor for the institution. Wound healing disorders as shown in Fig. 4 may be tedious for patients. In our center, we decided that the lower complication rate on the forearm by the use of MatriDerm® is worth the additional costs. The standard length of hospital stay after the creation of a phallus equaled 21 nights. In our patient collective, the average stay in group A was 20 days (range 16–36 days) and in group B was 22 days (range 15–49 days). The statistical outliers were due to wound healing disorders on the forearm.
Considering that the major part of our patients undergoing phalloplasty are transgender men, we respect the distress the patients undergo before presenting for surgery, or even before being diagnosed correctly [23].Whenever possible unfavourable preoperative conditions such as smoking and low or high BMI are improved in an interdisciplinary team approach. We aim to achieve a result within acceptable margins and try not to deny access to sex reassignment surgery.
For a long time, we witnessed an aesthetically appealing result on the radial forearm in both groups (Fig. 5). However, to integrate our patients as soon as possible into social and professional life, we focus on short-term and midterm results. Especially in skinny patients, the tension on the donor site is high, and wound healing disorders occur more likely; the use MatriDerm® and split-thickness skin graft for donor site defect coverage shows excellent functional and aesthetic outcomes as described by others [18]. Even though the scar in the groin area, respectively on the thigh, is stigmatizing in our patients, we witnessed a certain acceptance, since the scar can be effectively hidden in swimming trunks and shorts.
To our experience, some patients conceal the stigmatizing scar on the radial forearm by artfully designed tattoos. Unfortunately, there is a lack in literature about the possibilities and limitations of tattooing on skin grafts. To our knowledge, when using ink on split-thickness skin graft alone, the artwork will end up blurred since the ink tends to run away, and when tattooing on full-thickness skin graft or MatriDerm® and split-thickness skin graft, this problem does not occur.
Conclusion
The use of a dermal template such as MatriDerm® significantly reduced the complication rate at the forearm donor site in patients undergoing free radial forearm phalloplasty and may yield aesthetic outcomes compared to the use of full-thickness skin graft alone, or even better in some cases. However, the visible donor site at the thigh after split-thickness skin harvest has to be considered as well and in the end weighed against the donor site after full-thickness skin graft harvest in the groin. Especially in skinny patients, this second donor site may be a problem and be unsightly.
References
Baumeister S, Sohn M, Domke C, Exner K (2011) Phalloplasty in female-to-male transsexuals: experience from 259 cases. Handchir Mikrochir Plast Chir 43:215–221
Holzbach T, Giunta RE, Machens H-G, Müller D (2011) Phalloplasty with pedicled anterolateral thigh flap (“ALT-Flap”)]. Handchir Mikrochir Plast Chir 43:227–231
Scholten MM, Grundentaler R, Bull S, Küntscher MV (2013) Variety of the radial forearm phalloplasty with respect to urethral construction - a review. Handchir Mikrochir Plast Chir 45:211–216
Selvaggi G, Monstrey S, Hoebeke P et al (2006) Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast Reconstr Surg 118:1171–1177
Monstrey S, Hoebeke P, Selvaggi G et al (2009) Penile reconstruction: is the radial forearm flap really the standard technique? Plast Reconstr Surg 124:510–518
Monstrey SJ, Ceulemans P, Hoebeke P (2011) Sex reassignment surgery in the female-to-male transsexual. Semin Plast Surg 25:229–244
Wirthmann A, Finke JC, Giovanoli P, Lindenblatt N (2014) Long-term follow-up of donor site morbidity after defect coverage with Integra following radial forearm flap elevation. Eur J Plast Surg 37:159–166
Rieger UM, Majenka P, Wirthmann A, Sohn M, Bozkurt A, Djedovic G (2016) Comparative study of the free microvascular groin flap: optimizing the donor site after free radial forearm flap phalloplasty. Urology 95:192–196
Van Caenegem E, Verhaeghe E, Taes Y et al (2013) Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. J Sex Med 10:1644–1651
Doornaert M, Hoebeke P, Ceulemans P, T’Sjoen G, Heylens G, Monstrey S (2011) Penile reconstruction with the radial forearm flap: an update. Handchir Mikrochir Plast Chir 43:208–214
Chang T-S, Hwang W-Y (1984) Forearm flap in one-stage reconstruction of the penis. Plast Reconstr Surg 74:251–258
Gottlieb LJ, Levine LA (1993) A new design for the radial forearm free-flap phallic construction. Plast Reconstr Surg 92:284
Sidebottom AJ, Stevens L, Moore M et al (2000) Repair of the radial free flap donor site with full or partial thickness skin grafts. A prospective randomised controlled trial. Int J Oral Maxillofac Surg 29:194–197
Wirthmann AE, Majenka P, Kaufmann MC et al (2018) Phalloplasty in female-to-male transsexuals by Gottlieb and Levine’s free radial forearm flap technique-a long-term single-center experience over more than two decades. J Reconstr Microsur 34:235–241
Avery CM, Pereira J, Brown AE (2001) Suprafascial dissection of the radial forearm flap and donor site morbidity. Int J Oral Maxillofac Surg 30:37–41
Avery CME (2010) Review of the radial free flap: is it still evolving, or is it facing extinction? Part one: soft-tissue radial flap. Br J Oral Maxillofac Surg 48:245–252
Sinha UK, Shih C, Chang K, Rice DH (2002) Use of AlloDerm for coverage of radial forearm free flap donor site. Laryngoscope 112:230–234
Watfa W, di Summa PG, Meuli J, Raffoul W, Bauquis O (2017) MatriDerm decreases donor site morbidity after radial forearm free flap harvest in transgender surgery. J Sex Med 14:1277–1284
Wax MK, Winslow CP, Andersen PE (2002) Use of allogenic dermis for radial forearm free flap donor site coverage. J Otolaryngol 31:341–345
Halim AS, Khoo TL, MohdYussof SJ (2010) Biologic and synthetic skin substitutes: an overview. Indian J Plast Surg 43:S23–S28
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Lumen N, Monstrey S, Selvaggi G, Ceulemans P, De Cuypere G, Van Laecke E, Hoebeke P (2008) Phalloplasty: a valuable treatment for males with penile insufficiency. Urology 71(2):272–276; discussion 276–277. https://doi.org/10.1016/j.urology.2007.08.066
Winter S, Diamond M, Green J et al (2016) Transgender people: health at the margins of society. Lancet 23:390–400
Funding
Open access funding provided by University of Zurich
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Burger, A., Kiehlmann, M., Gruenherz, L. et al. Donor Site Defect Coverage of the Forearm with Dermal Substitute After Harvesting Radial Forearm Free Flap for Phalloplasty: Is MatriDerm® Worth the Effort?. Indian J Surg 85, 1356–1361 (2023). https://doi.org/10.1007/s12262-023-03705-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-023-03705-3