Abstract
Pulmonary sequestration (PS) is a rare congenital pulmonary dysplasia which presents with recurrent chest infections and haemoptysis. Its diagnosis is difficult and suspected on contrast-enhanced chest CT. The definitive treatment of pulmonary sequestration is surgical resection or endoluminal occlusion of the abnormal feeding vessel. Here, we report an innovative technique in which per-operative indocyanine green guided excision of intra-lobar sequestrated lung parenchyma and ligation of abnormal feeding vessel. The first patient was a 44-year-old gentleman with recurrent bouts of cough for 2 years. Courses of antibiotics failed to resolve it. Fibreoptic bronchoscopy and routine blood tests did not show any abnormality. CECT chest showed multiloculated cystic solid and low density mass in the right lower lung. The area of the lesion received its blood supply from anomalous systemic artery originating from coeliac trunk. Intraoperative, indocyanine green was injected into the atypical vessel, and pulmonary sequestration turned green. A sequential atypical lung resection could be completely removed with parenchyma preservation. The second patient was a 53-year-old lady presenting with chest pain, cough and expectoration for 2 years not responding to general management and antibiotics. CECT showed a low-density mass in the right lower lung lobe, with a feeding arterial vessel arising from the abdominal aorta. This was diagnosed as PS and resected using per-operative indocyanine green with parenchymal preservation and ligation of feeding vessel. Both patients have been followed up for at least 1 year and are symptom free. The intraoperative use of indocyanine green could greatly facilitate the presentation of the extent of a lung sequestration and safe resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pulmonary sequestration (PS) is a rare congenital lung anomaly defined as an area of lung tissue with an anomalous systemic blood supply and various forms of venous drainage. This lung tissue does not communicate with the tracheobronchial tree and has histologically abnormal bronchial epithelium. PS most commonly present as recurrent pneumonia [1]. Thirty per cent of pulmonary sequestration is incidental findings [2]. The gold standard of treatment for PS is surgical resection via thoracotomy or video-assisted thoracic surgery (VATS) [3]. The technique of visualizing the demarcation line using indocyanine green contrast dye (ICG) during pulmonary resection has recently been developed, and it has a relatively high success rate.
Case Presentation
Patient 1
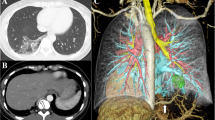
A 44-year-old male patient was admitted to our hospital due to cough and recurrent episodes of pneumonia during the last 2 years. CECT chest showed multiloculated cystic solid and low-density mass in the right lower lung (Fig. 1A, B). The area of the lesion received its blood supply from anomalous systemic artery originating from coeliac trunk (Fig. 1C). Muscle-sparing moderate anterolateral thoracotomy was performed. Intraoperatively, the boundary of the sequestration was not clear. The aberrant arterial supply was identified and ligated distally. Intraoperative, indocyanine green was injected into the atypical vessel (10 ml ICG (2.5 mg ICG)), and pulmonary sequestration turned green. A sequential atypical lung resection could be completely removed with parenchyma preservation (Fig. 3C, D). Postoperative course was uneventful, and the patient was discharged on postoperative day 8. Pathological findings of the resected specimen showed inflammatory lung tissue, with multiple cystic spaces willed with purulent secretions.
Patient 2
The second patient was a 53-year-old lady presenting with chest pain, cough and expectoration for 2 years not responding to general management and antibiotics. The patient had a history of smoking and pulmonal emphysema. CECT showed a low-density mass in the right lower lung lobe, with a feeding arterial vessel arising from the abdominal aorta (Fig. 2). As in the first case, atypical wedge resection was performed via a muscle-sparing anterolateral right thoracotomy. This was diagnosed as PS and resected using per-operative indocyanine green with parenchymal preservation and ligation of feeding vessel (Fig. 3). A sequential atypical lung resection could be completely removed with parenchyma preservation. The postoperative course was uneventful, and the patient was discharged on postoperative day 9. The postoperative chest radiograph demonstrates well-expanded lungs with interlobar effusion (Fig. 4C, D). Pathogenic analysis revealed an aberrant artery, a dilated bronchus, bronchitis and alveolitis with multiple cystic spaces. One-year after surgery, she is going well.
Discussion
This report shows in two cases of intralobar PS the safety and utility of ICG-guided pulmonary resection for intralobar pulmonary sequestration. PS is a very rare anomaly and accounts for 0.15 to 6.4% of all congenital lung malformations [4]. In most cases, PS has a single feeding artery; among the total blood supplied, 70% originates from the thoracic aorta and (6.9–31.6%) from abdominal aorta [5]. For the therapy of PS, there are various options such as surgical resection of PS combined with percutaneous endovascular embolization of the feeding systemic vessel. The gold standard of PS involves surgical resection especially for symptomatic patients, while asymptomatic patients are often treated with surgery to avoid infection, massive haemoptysis and damage to the lung parenchyma. In our cases, thoracoscopic surgery was not possible in adulthood because of severe adhesions after recurrent pneumonia and recurrent pleuritis. Sublobar resection is usually performed for small sequestration. Traditionally, the boundaries were identified intraoperatively with inflation/deflation of the target segment by clamping and unclamping the relevant bronchus.
Intraoperatively, the extent and delineation of PS was not clear, so ICG was used as part of an open-surgical procedure. A parenchyma-saving wedge resection was performed after thoracotomy and visualization of PS by injection of ICG into the aberrant vessel. PS could be visualized 3–8 min after injection. In contrast to methylene blue, ICG has been used as a contrast agent for intraoperative detection of PS because of its hepatic clearance and its limited systemic side effects [6]. Only few cases of pulmonary resection for intralobar pulmonary sequestration using ICG have been reported. In most cases, ICG is given intravenously and repeatedly [7,8,9]. In our cases, the ICG was injected directly into the aberrant artery. However, the incidence of anaphylactic shock due to ICG used for angiography at doses of 25 to 75 mg was reported to be 0.05%. Although the dose of ICG was quite low at 3 mg in the present cases, the demarcation line of target segment was clearly identified, so this dose of ICG was sufficient for identification of the segmental line. Using such a low dose of ICG is safe, as well, by helping avoid anaphylactic shock.
Conclusions
The intraoperative use of Indocyanine green can greatly facilitate the presentation of the extent of a lung sequestration and safe resection.
References
Hertzenberg C, Daon E, Kramer J (2012) Intralobar pulmonary sequestration in adults: three case reports. JThorac Dis 4(5):516–519
Alsumrain M, Ryu JH (2018) Pulmonary sequestration in adults: a retrospective review of resected and unresected cases. BMC Pulm Med. 18(1):97
Wei Y, Li F (2011) Pulmonary sequestration: a retrospective analysis of 2625 cases in China. Eur J Cardiothorac Surg 40(1):e39-42
Hakiri S, Fukui T, Chen-Yoshikawa TF. Combined surgical therapy for pulmonary sequestration and aberrant artery from the abdominal aorta. Gen Thorac Cardiovasc Surg. 2021 Jun;69(6):1031–1034.Alsumrain M, Ryu JH. Pulmonary sequestration in adults: a retrospective review of resected and unresected cases. BMC Pulm Med. 2018 Jun 05;18(1):97
Xie D, Xie H, You X, Chen C, Jiang G (2013) Pulmonary sequestration with aberrant arteries arising from the renal artery and the internal thoracic artery. Ann Thorac Surg 96(5):e131
van Manen L, Handgraaf HJM, Diana M, Dijkstra J, Ishizawa T, Vahrmeijer AL, Mieog JSD (2018) A practical guide for the use of indocyanine green and methylene blue in fluorescence-guided abdominal surgery. J Surg Oncol 118(2):283–300
Kasai Y, Tarumi S, Chang SS, Misaki N, Gotoh M, Go T, Yokomise H (2013) Clinical trial of new methods for identifying lung intersegmental borders using infrared thoracoscopy with indocyanine green: comparative analysis of 2- and 1-wavelength methods. Eur J Cardiothorac Surg 44(6):1103–1107
Motono N, Iwai S, Funasaki A, Sekimura A, Usuda K, Uramoto H (2019) Low-dose indocyanine green fluorescence-navigated segmentectomy: prospective analysis of 20 cases and review of previous reports. J Thorac Dis 11(3):702–707
Tarumi S, Misaki N, Kasai Y, Chang SS, Go T, Yokomise H (2014) Clinical trial of video-assisted thoracoscopic segmentectomy using infrared thoracoscopy with indocyanine green. Eur J Cardiothorac Surg 46(1):112–115
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ibrahim, A., Murtaja, A. & Oberhuber, A. Indocyanine Green to Visualize and Resect Pulmonary Sequestration in Adults. Indian J Surg 85 (Suppl 2), 540–544 (2023). https://doi.org/10.1007/s12262-022-03564-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03564-4