Abstract
The York Mason procedure was initially described for the management of recto-urinary fistulae. Although this procedure may be difficult to perform, success rates and long-term outcomes are encouraging. Adopting this technique for the management of a complex non-recto-urinary fistula in ano may be reasonable. In this manuscript, the York Mason technique was modified to repair a complex type 4 anterior fistula in ano without involvement of the urinary system with good results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The York Mason procedure is a technique employed to manage recto-urinary and recto-urethral fistulae [1]. The results of this technique for the management of this complex entity have been encouraging based on current literature [2]. In short, the York Mason procedure involves an open dissection of the posterior rectal wall to enable optimal exposure of the anterior anorectum for surgical repair of complex fistulae in this region, e.g., recto-urinary fistula. The procedure involves the division of the external sphincter ani, the internal sphincter ani, the levator ani muscles, and the posterior rectal wall to gain access to and repair recto-urinary fistulae [3].
Patients and Methods
A 47-year-old gentleman was referred to our coloproctology unit with a chronic anterior fistula following incision and drainage of an abscess at the penis root 3 years prior to referral. The surgical history with regard to the fistula included 23 procedures prior to referral. Previous procedures included seton placement, excision and closure, negative pressure wound therapy, LIFT, flap techniques, and fecal deviation via a loop ileostoma.
Work-up
A close to 2-cm-wide fistula tract was evident during examination under general anesthesia. At that time, curettage was performed, and a loose draining seton was inserted. Reconstructive surgery was scheduled 3 months later. Imaging with computed tomography (CT) and magnet resonance imaging (MRI) was obtained prior to surgery. No specific bowel preparation besides an enema was needed.
Surgical Procedure
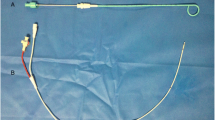
Single-shot antibiotics with intravenous (IV) cefuroxime and metronidazole were given prior to incision. The patient was placed in a prone jackknife position with the buttocks strapped apart. The rectal ampulla was irrigated with octenisept and rinsed with normal saline. The skin incision was made on the left gluteal region over a length of 15 cm from the anal verge. The subcutaneous tissue was dissected down to the musculature (Fig. 1a and b). Then, the external sphincter ani muscle was dissected, divided between claps, and ligated with 4/0 PDS sutures (Fig. 2a). Next, the internal sphincter ani muscles were separated, clapped divided, and sutured (Fig. 2b). Finally, the levator ani muscle was dissected, divided, and ligated (Fig. 3). A Lone Star retractor was used to optimize exposure. The posterior rectum was incised over a length of 5 cm, and a second retractor was used to improve the exposure of the anterior anorectum for free access to the fistula. The size of the fistula can be appreciated after replacing the draining seton (Fig. 4a) with sponge forceps (Fig. 4b). The fistula tract was debrided with excision of scary tissues and irrigated with normal saline (Fig. 5a). The fistula was then closed using two 3/0 barbed PDS sutures (Fig. 5b). The first suture line was placed at the level of the muscularis, while a mucosa flap was employed in the second suture line [4]. The rationale for this suture technique, according to the author, is to prevent direct contact of both suture lines, as this may increase the risk of failure or recurrence.
A two-layer closure technique was used to close the posterior rectum. First, the muscularis was closed using a 4/0 barbed PDS suture. The mucosa was then closed using a 5–0 PDS running suture. Pelvic floor reconstruction was performed by anastomosing the corresponding muscle groups using the sutures placed during muscle division. A suction drain was placed, followed by subcutaneous sutures and skin closure (Fig. 6). The suction drain was removed on postoperative day 2, and the patient was discharged on postoperative day 5.
Results
Rectal examination and MRT 12 weeks later confirmed a complete closure of the fistula. Flexible endoscopy confirmed a well-healed rectum. Ileostomy closure will be scheduled after pelvic floor training.
Discussion
The York Mason procedure is a complex reconstructive procedure initially described for the repair of recto-urinary fistulae. In the present scenario, the York Mason procedure was modified to manage a complex anterior fistula following incision and drainage of an abscess at the penis root. In the original technique described by Mason and Kilpatrick, the incision was made relatively close to the midline extending from the sacrococcygeal junction to the anal verge [3]. A personal preference is to carry the incision as far away from the midline as possible because this increases the patient’s comfort and reduces the risk of wound infection.
The complex nature of the anterior fistula, in this case, is primarily defined by the course of the fistula tract through a relevant portion of the sphincter apparatus. This was a high, type 2 transsphincteric fistula according to Park’s classification [5] and secondarily by the number of previously attempted (twenty-three) repairs. This is in accordance with the finding of relevant scary tissues along the fistula tract during surgery. Nonetheless, surgery and recovery were uneventful.
The major advantages of this technique include the optimal exposure of fistulae at a difficult-to-access site, good healing rates with a low risk of recurrence, and a small risk of continence disturbance [2, 6, 7]. Although the York Mason procedure was primarily used for closed recto-urinary fistulae, it can be modified to successfully manage complex anterior fistulae in ano without the involvement of the urinary structures.
References
Kilpatrick F, Mason AY (1969) Post-operative recto-prostatic fistula 1. Br J Urol 41(6):649–654
Renschler TD, Middleton RG (2003) 30 years of experience with York-Mason repair of recto-urinary fistulas. J Urol 170(4 Part 1):1222–1225
Mason AY, Kilpatrick F (1973) Rectoprostatic and rectourethral fistulae. SAGE Publications, In.
Boenicke L, Karsten E, Zirngibl H, Ambe P (2017) Advancement flap for treatment of complex cryptoglandular anal fistula: prediction of therapy success or failure using anamnestic and clinical parameters. World J Surg 41(9):2395–2400
Parks A, Gordon PH, Hardcastle J (1976) A classification of fistula-in-ano. Br J Surg 63(1):1–12
Hadley DA, Southwick A, Middleton RG (2012) York-Mason procedure for repair of recto-urinary fistulae: a 40-year experience. BJU Int 109(7):1095–1098
Falavolti C, Sergi F, Shehu E, Buscarini M (2013) York Mason procedure to repair iatrogenic rectourinary fistula: our experience. World J Surg 37(12):2950–2955
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ambe, P.C. Modified York Mason Procedure for the Closure of a Complex Anterior Fistula in Ano. Indian J Surg 85, 925–928 (2023). https://doi.org/10.1007/s12262-022-03552-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03552-8