Abstract
Choledocholithiasis means the presence of gallstone inside the common bile duct (CBD). Removing the bile duct stones can be done surgically using endoscopic catheters. In this study, we aim to assess the safety and efficacy of basket catheters compared to balloon catheters at bile duct stone clearance. We searched four databases for clinical trial and cohort studies that compare basket catheter and balloon catheter in bile duct stone extraction. We extracted data from the included studies. These data were pooled as mean difference (MD) or risk ratio (RR) with 95% confidence interval (CI) using Review Manager software (version 5.3) and OpenMetaAnalyst software for zero-event outcomes. In a total of 728 patients, we find that the balloon catheter was better than the basket catheter regarding incomplete bile duct stone clearance (RR = 0.91, 95% CI [0.85, 0.98], P = 0.01). Regarding the number of the extracted stones by both catchers, the analysis favored the balloon catheter over the basket for clearance when less than four stones (RR = 0.91, 95% CI [0.85, 0.99], P = 0.02) but no significant difference for more than four stones (RR = 0.77, 95% CI [0.48, 1.24], P = 0.29). There was no significant difference between the two groups. The analysis revealed that the balloon catheter is better than the basket catheter for choledocholithiasis regarding the complete clearance of the stone. However, there was no significant difference regarding the safety outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dr. Elliot-Smith, the great Egyptologist and anatomist, discovered an Egyptian mummy containing 30 gallstones, which has been presented in the Museum of the Royal College of Surgeons in London until the Second World War [1, 2]. Choledocholithiasis indicates the presence of gallstone inside the common bile duct (CBD), which carries bile from hepatic and cystic ducts to the small bowel [3]. The common hepatic duct (CHD) is the first section of the biliary tract, which extends from the cooperation of the right and left bile duct and connects the gallbladder by the short cystic duct [4,5,6]. Choledocholithiasis are formed due to the precipitation of bile components of bile salts, bilirubin, fat, cholesterol, and protein in the gallbladder or CBD [7]. According to the composition, choledocholithiasis is classified into cholesterol or pigmented stones, while according to the location, they are classified into extrahepatic or intrahepatic stones [3].
In the USA, about 6 million men and 14 million women have been diagnosed with gallbladder stones [8, 9]. These stones of CBD can be detected using ultrasound, computed tomography scans (CT), laboratory tests, and magnetic resonance cholangiopancreatography (MRCP). However, gallstones may be complicated with jaundice, cholangitis, biliary pancreatitis, biliary cirrhosis, lobar atrophy, liver abscess, or cholangiocarcinoma [3, 10].
Clinically, bile duct stones can be symptomatic and asymptomatic; however, to remove the symptomatic bile duct stones, the endoscopic retrograde cholangiopancreatography (ERCP) was recommended according to British guidelines [11, 12]. Either balloon or basket catheters can be used for stone retrieval, in which about 85–90% of stones can be easily extracted by both methods following endoscopic sphincterotomy (EST), while bout 10–15% could be hard to deal with [13, 14].
The traditional basket catheter is called a Dormia basket. It can capture and withdraw stones. The balloon catheter can capture small stones by obstructing the bile duct lumen after distention. That cannot prevent the moving of small stones to be impacted in the corner pocket at the lower end of the cystic bile duct during stone extraction. Hence, the traction power is better in the basket than in the balloon catheter [15].
According to the European Society of Gastrointestinal Endoscopy (ESGE) guidelines, the difference between balloon or basket catheter is slightly minimal, so endoscopists can use any, while according to the American guidelines, the balloon catheter is highly recommended for safety issues related to basket impaction [12, 16]. Although insufficient sphincterotomy or stone larger than appraised makes basket catheter crashes the papilla of Vater, the Japanese doctors still prefer the basket catheter over the balloon due to its durability and better traction [17, 18]. Therefore, due to this variety of preferences between the basket and balloon catheters, we aimed in this systematic review and meta-analysis to systematically compare both techniques in the light of the available evidence in the literature (Tables 1 and 2).
Materials and Method
We conducted this systematic review and meta-analysis using handbook guidelines of systematic reviews of interventions and the PRISMA checklist for systematic review and meta-analysis [19, 20].
Search Strategy
We searched four databases, PubMed, Scopus, Web of Science (WOS), and Cochrane Library, through July 2021 using the following terms, ((Basket catheter) AND (Balloon catheter)) AND (Choledocholithiasis), without any restrictions on time or language.
Study Selection
We included randomized control trials and retrospective cohort studies that compared basket catheter and balloon catheter for choledocholithiasis. We excluded other studies, which did not meet our inclusion criteria. We conducted two steps of screening: title/abstract screening and then full-text screening. Two independent reviewers performed the screening, and a third reviewer resolved the disagreements between the two reviewers.
Data Extraction
Two independent authors extracted the data from the included studies, and a third one resolved the disagreements. We extracted the characteristics of included studies, baseline characteristics of included patients, risk of bias domains, and study outcomes.
Study Outcomes
The primary outcomes are efficacy outcomes, including the following: (1) time to complete clearance by assigned catheter, (2) complete the clearance by assigned catheter, (3) clearance according to the number of stones, and safety outcomes which include the following: (1) pancreatitis, (2) bleeding, (3) perforation, and (4) cholangitis.
Risk of Bias Assessment
Two independent reviewers conducted risk of bias assessment according to the Cochrane risk of bias (ROB) assessment tool, which is adequately described in Chapter 8.5 of the Cochrane handbook of systematic reviews of interventions 5.1.0. [20]. Also, we used NIH Quality Assessment Tool for Observational Cohort Studies [21]. We did not use Egger’s and colleagues for randomized control trials due to the limited number of the included studies, which were less than ten [22].
Data Analysis
Continuous data were extracted and pooled as mean difference (MD) and with 95% confidence interval in a fixed-effect meta-analysis model, while dichotomous data were pooled as risk ratios (RR) with 95% confidence interval in a fixed-effect meta-analysis model. We used RevMan version 5.4 for windows and OpenMetaAnalyst for zero-event dichotomous data. Heterogeneity was assessed by the Chi-square test, and its extent was measured by the I-squared test. Resolvable heterogeneity was done using the random-effect model of meta-analysis.
Result
Literature Search
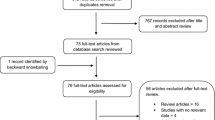
The initial search resulted in 381 articles from four databases. Of these 381 articles, we excluded 69 articles due to duplications, and the remaining 312 articles underwent title and abstract screening. We excluded 301, as they did not meet our criteria. The remaining 11 articles underwent full-text screening. Only four studies were finally included in the qualitative and quantitative analysis (Fig. 1).
Risk of Bias Assessment
We used the Cochrane risk of bias (ROB) assessment tool and the NIH assessment tool to assess the quality of the included clinical trials and retrospective cohort, respectively. The three included clinical trials were at low risk of bias (Fig. 2), while the cohort study was at a poor high risk of bias (Supplementary material).
Outcomes
Complete Clearance by Assigned Catheter
The analysis showed a significant difference between the balloon and assigned catheter. The balloon catheter clearance was better than basket catheter (RR = 0.91, 95% CI [0.85, 0.98], p = 0.01); the pooled studies were homogeneous (P = 0.46; I2 = 0%) [23]–[25] (Fig. 3a).
Time to Complete Clearance by Assigned Catheter
The analysis revealed no significant difference between the two groups favoring basket catheter (RR = 1.19, 95% CI [− 0.32, 2.7], p = 0.12); the pooled studies were heterogeneous (P < 0.0001; I2 = 94%), and the heterogeneity could not be resolved by sensitivity analysis due to the limited number of the studies in the subgroup [23, 24] (Fig. 3b).
Clearance According to the Number of Stones
Subgroup’s analysis was performed according to the number of stones. Our meta-analysis showed that in patients with ≥ 4 stones, balloon catheter clearance was significantly better than basket catheter (RR = 0.77, 95% CI [0.48, 1.42], P = 0.29); the pooled studies were homogeneous (P = 0.12; I2 = 60%). Likewise, in patients with < 4 stones, balloon catheter clearance was significantly better than basket catheter (RR = 0.91, 95% CI [0.85, 0.99], P = 0.02); pooled studies were homogeneous (p = 0.36; I2 = 0%). The overall effect estimate of these subgroups showed that balloon catheter clearance was better than basket catheter in stone clearance (RR = 0.91, 95% CI [0.83, 0.99], P = 0.02); the pooled studies were homogeneous (P = 0.31; I2 = 15%) [23, 24] (Fig. 4).
Pancreatitis
The overall effect estimate showed no significant difference between two groups favoring basket catheter (RR = 0.96, 95% CI [0.37, 2.46], P = 0.93); pooled studies were homogeneous (p = 0.82; I2 = 0%) [23, 24, 26] (Fig. 5a).
Bleeding
The analysis showed no significant difference between the two groups favoring basket catheter (RR = 0.7, 95% CI [0.2, 2.5], p = 0.59); pooled studies were homogeneous (p = 0.53; I2 = 0%) [23, 24, 26] (Fig. 5b).
Cholangitis and Perforation
There was no significant difference between two groups regarding cholangitis or perforation (RR = 1.156; CI [0.60, 3.47]; P = 0.9) [23, 24] (RR = 0.670, CI [0.083, 5.406]; P = 6.70), respectively [23, 24, 26] (Fig. 6a and b).
Discussion
In this systematic review and meta-analysis, we pooled data from three clinical trials and one cohort study with a total of 728 patients to compare the balloon catheter with basket catheter for bile duct stone extraction. From our analysis results, the balloon catheter showed a significant superiority to the basket catheter at complete stone clearance but with no significant difference between the two groups at the time for complete stones removal and safety including pancreatitis, bleeding, perforation, and cholangitis. A subgroup analysis was done according to the number of extracted stones, and balloon catheter was better than basket catheter.
By viewing the literature, Lauri et al. (1993) [27] reported that endoscopic extraction effectively treats patients with CBD stones. Stromberg et al. (2011) [28] conducted a comparison between the laparoscopic technique and ERCP and found the lowest mortality and morbidity rates with ERCP. Yasuda et al. (2013) [29] reviewed other new treatments of bile duct stones; they conclude that endoscopic sphincterotomy followed by using balloon or basket catheter is still the first line of treatment for bile duct stones. Furthermore, Misra et al. (2008) [30] found that using large-diameter (15-mm, 18-mm, or 20-mm maximum sizes) balloon dilation of the sphincterotomy site in patients who could not get bile duct stones out with endoscopic sphincterotomy and dormia basket or balloon catheter extraction was adequate, which support our study results.
However, Lin et al. (2004) [33] found that complete bile duct stone clearance is higher in endoscopic sphincterotomy than endoscopic balloon dilatation. Both techniques are safe and successful options to remove CBD stones. In patients with coagulopathy, endoscopic balloon dilatation is healthy and does not increase the risk of pancreatitis or hemorrhage.
The basket catheter has a bullet-shaped distal tip with an opening diameter of 22 mm for quick insertion in the CBD, besides distal and proximal portions containing four wires to be inserted into the CBD using the free-hand technique. This catheter has a contrast material injection lumen, which allows for visualization of any remaining stones during removal. To fit the anatomical condition of each case, each balloon can be easily modified to one of three sizes (8.5, 11.5, and 15 mm) [18, 31]. To perform balloon occlusion cholangiography (BOC), this catheter is inserted into the CBD using a wire-guided technique and has a contrast-injection hole above the balloon [23].
Endoscopic balloon dilation (EBD) of the biliary sphincter is an alternative to biliary sphincterotomy. The potential advantages of EBD over sphincterotomy are that it preserves the biliary sphincter and also reduces the risk of bleeding compared with a biliary sphincterotomy. However, a single multi-center study in 237 patients randomized to either endoscopic sphincterotomy or balloon dilation was stopped early due to increased rates of pancreatitis (15.4% vs 0.8%), with two deaths due to pancreatitis in the dilation group. EBD can be considered as an alternative to endoscopic sphincterotomy in patients at high risk for endoscopic sphincterotomy such as those with a bleeding disorder, altered anatomy (i.e., Billroth II), or difficult anatomy such as a periampullary diverticulum. In patients with large CBD stones with a prior sphincterotomy, EBD can also be used as an alternative to extending the sphincterotomy [32].
Our review has firstly compared between basket and balloon catheter for bile duct stones extraction. All included clinical trials were at low risk of bias and high level of evidence, while the included cohort study was at low quality. However, there are some limitations as the small number of included studies, and small total sample may cause possible publication bias, which we could not assess due to the small number of the included studies.
In conclusion, the balloon catheter is better than the basket catheter regarding the extraction of bile duct stone; it takes the upper hand regarding the complete clearance of the stones. However, there was no significant difference between the two groups regarding safety outcomes. Future studies with larger sample sizes are recommended to obtain a high level of evidence regarding bile duct stone extraction using the catheter.
Data Availability
All data and material are available upon reasonable request from the corresponding author.
References
Glenn F (1971) Biliary tract disease since antiquity. Bull New York Acad Med J Urban Heal 47(4):329–350
Ellis PH (2019) The story of gallstones and their treatment. J Perioper Pract 29(11):382–384. https://doi.org/10.1177/1750458919838450
McNicoll CF, Pastorino A, Farooq U, St Hill CR (2021) Choledocholithiasis. In: StatPearls [Internet]. StatPearls Publishing
Manohar R, and Lagasse E (2013) “Liver stem cells,” in Principles of Tissue Engineering: Fourth Edition, Elsevier Inc., pp. 935–950
Bergman S, Geisinger KR (2008) Alimentary Tract (Esophagus, Stomach, Small Intestine, Colon, Rectum, Anus, Biliary Tract). In: Comprehensive Cytopathology. Elsevier Inc., pp 373–408
Turner MA, Fulcher AS (2001) The cystic duct: normal anatomy and disease processes. Radiographics 21(1):3–22. https://doi.org/10.1148/radiographics.21.1.g01ja093
Lammert F et al (Dec. 2016) Gallstones. Nat Rev Dis Prim 2(1):16024. https://doi.org/10.1038/nrdp.2016.24
Costi R, Gnocchi A, Di Mario F, Sarli L (2014) Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. In: World Journal of Gastroenterology
Shabanzadeh DM (2018) New determinants for gallstone disease? Danish Med J 65:1–18
Park C-H (2018) The management of common bile duct stones. Korean J Gastroenterol 71:260. https://doi.org/10.4166/kjg.2018.71.5.260
Millat B, Borie F (2000) [Common bile duct stones and their complications]. In: La Revue du praticien
Williams EJ, Green J, Beckingham I et al (2008) Guidelines on the management of common bile duct stones (CBDS). Gut 57:1004–1021. https://doi.org/10.1136/gut.2007.121657
Seitz U, Bapaye A, Bohnacker S, Navarrete C, Maydeo A, Soehendra N (Nov. 1998) Advances in therapeutic endoscopic treatment of common bile duct stones. World J Surg 22(11):1133–1144. https://doi.org/10.1007/s002689900532
McHenry L, Lehman G (Apr. 2006) Difficult bile duct stones. Curr Treat Options Gastroenterol 9(2):123–132. https://doi.org/10.1007/s11938-006-0031-6
Ishiwatari H et al (2016) Balloon catheter versus basket catheter for endoscopic bile duct stone extraction: a multicenter randomized trial. Endoscopy 48(4):350–357. https://doi.org/10.1055/s-0035-1569573
Maple JT et al (Oct. 2011) The role of endoscopy in the management of choledocholithiasis. Gastrointest Endosc 74(4):731–744. https://doi.org/10.1016/j.gie.2011.04.012
Ekmektzoglou K, Apostolopoulos P, Dimopoulos K, et al Basket versus balloon extraction for choledocholithiasis: a single center prospective single-blind randomized study. Acta gastro-enterologica Belgica 83:577–584
Binmoeller KF, Schafer TW (Feb. 2001) Endoscopic management of bile duct stones. J Clin Gastroenterol 32(2):106–118. https://doi.org/10.1097/00004836-200102000-00004
Moher D et al (Jul. 2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Higgins JPT, Thomas J, Chandler J et al (2019) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons
National Heart and Blood Institute L (2014) Quality assessment tool for observational cohort and cross-sectional studies
Stuck AE et al (Feb. 1998) Bias in meta-analysis detected by a simple, graphical. BMJ 316(7129):469–469. https://doi.org/10.1136/bmj.316.7129.469
Ekmektzoglou K et al (2020) Basket versus balloon extraction for choledocholithiasis: a single center prospective single-blind randomized study. Acta Gastro-Enterol Belg 83(4):577–584
Ishiwatari H et al (2016) Balloon catheter versus basket catheter for endoscopic bile duct stone extraction: a multicenter randomized trial. Endoscopy 48(04):350–357. https://doi.org/10.1055/s-0035-1569573
Ozawa N et al (2017) Prospective randomized study of endoscopic biliary stone extraction using either a basket or a balloon catheter: the BasketBall study. J Gastroenterol 52(5):623–630. https://doi.org/10.1007/s00535-016-1257-2
Takeshita K, Asai S, Fujimoto N, Ichinona T, Akamine E (2020) Comparison of the effects of retrieval balloons and basket catheters for bile duct stone removal on the rate of post-ERCP pancreatitis. Hepatobiliary Pancreat Dis Int. https://doi.org/10.1016/j.hbpd.2020.04.004
Lauri A, Horton RC, Davidson BR, Burroughs AK, Dooley JS (1993) Endoscopic extraction of bile duct stones: management related to stone size. Gut 34(12):1718–1721. https://doi.org/10.1136/gut.34.12.1718
Strömberg C, Nilsson M (2011) Nationwide study of the treatment of common bile duct stones in Sweden between 1965 and 2009. Br J Surg 98(12):1766–1774. https://doi.org/10.1002/bjs.7690
Yasuda I, Itoi T (2013) Recent advances in endoscopic management of difficult bile duct stones. Dig Endosc 25(4):376–385. https://doi.org/10.1111/den.12118
Misra SP, Dwivedi M (Mar. 2008) Large-diameter balloon dilation after endoscopic sphincterotomy for removal of difficult bile duct stones. Endoscopy 40(3):209–213. https://doi.org/10.1055/s-2007-967040
Katanuma A, Maguchi H, Osanai M, Takahashi K (May 2010) Endoscopic treatment of difficult common bile duct stones. Dig Endosc 22:S90–S97. https://doi.org/10.1111/j.1443-1661.2010.00979.x
Canard JM, Lennon AM, Létard JC, et al (2011) Endoscopic retrograde cholangiopancreatography. In: Gastrointestinal Endoscopy in Practice. Elsevier, pp 370–465
Lin CK et al (Jan. 2004) Endoscopic balloon dilatation is a safe method in the management of common bile duct stones. Dig Liver Dis 36(1):68–72. https://doi.org/10.1016/j.dld.2003.09.014
Acknowledgements
We would like to thank our International Medical Research Association (IMedRA) colleagues for their ongoing efforts, encouragement, and support.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Each author contributed to the manuscript with major contributions according to ICMJE criteria. Two independent authors (Elsnhory A. B. and Montaser A. G.) did the screening, either title and abstract screening or full-text screening. The rest of the author did manual screening and screened the references of the finally included studies. Another two independent author evaluates the studies’ quality and risk of bias (Mandour O. A. and Kereet I. M.), and a third author (Rezk H. S.) supervised the quality assessment task and settle down any conflicts. Two independent authors did the extraction of the studies’ data (Elsnhory A. B., Mandour O. A.). The analysis was done by the first author (Elsnhory A. B.), and it was revised by the supervisor (Gbreel M. I.). All authors (Elsnhory A. B., Mandour O. A., Montaser A. G., kereet I. M., Rezk H. S., Ragab K. M., Rabea R. K., Gbreel M. I.) contributed in the manuscript writing with cross-revision by another author.
Corresponding author
Ethics declarations
Ethics Approval
Not needed.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsnhory, A.B., Mandour, O.A., Montaser, A.G. et al. A Systematic Review and Meta-analysis of Basket or Balloon Catheter for the Retrieval of Choledocholithiasis. Indian J Surg 85, 241–250 (2023). https://doi.org/10.1007/s12262-022-03435-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03435-y