Abstract
Locally advanced colon cancer is associated with poor prognosis. The aim of this report was to examine the association between the lymph node status and prognosis of locally advanced colon cancer. Perioperative and oncologic outcomes were studied in patients who had undergone colectomy for colon cancer between June 2004 and December 2018. Locally advanced colon cancer was defined as stage T4a/T4b cancer. The long-term oncologic results were investigated in patients with non-metastatic locally advanced colon cancer. Of 195 patients operated for locally advanced colon cancer, 83 (42.6%), 43 (22.1%), and 69 (35.3%) had pN0, pN1, and pN2 disease, respectively. Preoperative serum levels of CEA and CA 19-9, as well as incidence of distant metastases were significantly higher in patients with pN2 compared to those with pN0 and pN1. In non-metastatic setting, a trend towards higher incidence of recurrence was observed in node-positive patients. Nodal stage was a significant predictor for survival in the univariable analysis but non-significant after adjusting for confounders. Subgroup analyses among the patients with T4a and T4b cancer did not demonstrate any association between the nodal stage and survival. Preoperative CA 19-9 > 37 U/ml and adjuvant chemotherapy were the only prognostic factors in T4a and T4b colon cancer, respectively. Although a trend towards higher incidence of recurrence was observed in node-positive locally advanced colon cancer, nodal stage was not associated with survival. Adjuvant chemotherapy should be strongly considered in T4b stage colon cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colon cancer is one of the most common malignancies worldwide and the fourth most frequent cause of cancer-related death [1]. Despite the improvement in diagnostic modalities, 10–20% of patients are diagnosed with locally advanced colon cancer (LACC) known for its poor prognosis [2, 3]. Multidisciplinary treatment modalities are considered in patients with LACC although radical surgery remains the mainstay of its successful treatment [2].
Adequate lymphadenectomy is the crucial part of surgery in colon cancer as it results in both curative resection and correct lymph node staging [4]. Several studies reported positive lymph nodes to be associated with decreased survival in patients with LACC [5, 6]. Some reports though did not confirm these findings as other factors such as patient age, gender, CA 19-9, tumor location, disease stage, positive resection margins, and adjuvant chemotherapy were associated with survival [2, 7,8,9]. Yamanashi and co-workers suggest that lymph node ratio but not nodal stage is an independent predictor for survival although this report included also patients with rectal cancer [9]. At the same time, different definitions have been used for LACC. While some define T3-T4 stage colon cancer as locally advanced [10], others consider T4 stage solely [2, 8].
The impact of lymph node metastases and associated parameters (nodal stage, ratio) on survival in patients with LACC undergoing surgery remains unclear. The aim of this report was to examine the association between lymph node status and long-term outcomes following colectomy for LACC.
Patients and Methods
Patients with LACC who had undergone colectomy from June 2004 to December 2018 were included in the analysis. Data on patient demographics, clinical characteristics, perioperative and pathology work-up were obtained from a prospectively maintained database. The exclusion criteria were incomplete information on lymph node status and associated parameters. The groups were defined and classified according to the nodal stage set on pathology (pN0, pN1, and pN2) and compared in terms on perioperative, short-, and long-term oncologic outcomes. Prognostic factors for survival were analyzed.
Selection criteria for surgery and perioperative management have been described elsewhere [11]. Patient follow-up included clinical and instrumental (chest X-ray and abdominal ultrasound) examinations and measurement of serum tumor markers (CEA and CA 19-9) 3 and 6 months after surgery. These were followed by check-ups every 6 months for the first 5 years. Chest and abdominal computed tomography were performed 1 year after surgery and thereafter repeated annually.
LACC was defined as pT4 stage (pT4a and pT4b) colon cancer confirmed on pathology. Tumor and nodal stages were classified according to the criteria of the 8th edition of the American Joint Committee on Cancer [12]. Tumor size was defined as the largest dimension of the tumor measured microscopically at the pathology work-up. R0 was defined as no microscopic tumor in resected margins or lymph nodes. Colon cancer that were of histological type other than adenocarcinoma were excluded from the analysis. Recurrence was defined as radiological evidence of intra-abdominal soft tissue around the surgical site and/or distant metastases. Three main types of recurrence were specified—locoregional, distant metastases, and peritoneal carcinomatosis. Postoperative complications were defined and classified according to Clavien and Dindo [13]. Grade ≥ II complications were reported, and grade ≥ III complications were defined as severe. Mortality included cases of death within 30 days of surgery.
Normally and non-normally distributed continuous data were presented as means (± standard deviation) and medians (range), respectively. Numbers (percentages) were used to present categorical data. The Chi-square test or Fisher’s exact test was used to compare the categorical variables. The two-sample T-test was used to compare means, and the Mann-Whitney U test was used for medians. Two-tailed p value < 0.05 was considered statistically significant.
Median survival was estimated by using the Kaplan–Meier method. The log-rank test was applied to compare survival between the groups. Two-tailed p value <0.05 was statistically significant. Uni- and multivariable Cox regression analyses were used to identify the prognostic factors for survival. Variables significant at p value <0.1 were included in the multivariable backward logarithmic regression model. Two-tailed p value <0.05 was statistically significant.
Results
After applying the exclusion criteria, 195 patients were included in the analysis. Of those, 83 (42.6%), 43 (22.1%), and 69 (35.3%) were ultimately diagnosed with pN0, pN1, and pN2. The groups were comparable in terms of patient characteristics, clinical, and functional parameters (Table 1). The serum levels of CEA and CA 19-9 significantly increased together with an increase in the nodal stage—2.6 vs. 3.9 vs. 7.6 ng/ml (p = 0.005) and 5.5 vs. 8.6 vs. 17.6 (p = 0.003) for N0, N1, and N2, respectively. Operative time and estimated blood loss were similar, although the rate of red blood cell transfusion was significantly higher patients with N0 (22.9 vs. 4.7 vs. 7.2%, p = 0.003).
Postoperative results were similar between the groups. Pathology examination demonstrated significantly greater lymph node yield in patients with lymph node metastases compared to those without (Table 2). However, no differences were found between those with N1 and N2. Mean lymph node ratio was significantly higher in patients with N2 compared with N1 (0.58 vs. 0.14, p < 0.01). Distant metastases were more frequent in patients with N2 compared to those with N1 and N0 (52.2 vs. 20.9 vs. 15.7%, p < 0.01).
After excluding the patients with distant metastases (n = 58) and those who had died after surgery (n = 4), 133 were analyzed for long-term oncologic outcomes. No statistically significant differences were found in terms of utilizing adjuvant chemotherapy and recurrence (Table 3). Median follow-up was 36 (2–147) months. Median survival following colon resection for non-metastatic T4 stage cancer was 71 (38–104) months, while 3-, 5-, and 10-year survival rates were 64.1%, 51.9%, and 20.6%. Patients with T4a cancer had more than two times longer median survival compared to those with T4b—98 (88–108) vs. 37 (23–51), p = 0.009 (suppl. figure 1). Survival rates for non-metastatic T4a/T4b cancer at 3 and 5 years after surgery were 80.8/51.4% and 72.2/35.2%, respectively.
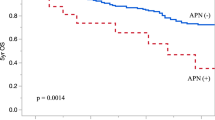
Significant differences in median survival were observed for patients with N0, N1, and N2 stages—93 vs. 48 vs. 24 months, p < 0.01 (Fig. 1). Obesity, elevated serum CA 19-9 level, adjuvant chemotherapy, T4 substage, and nodal stage were associated with survival in the univariable analysis (Table 4). In multivariable model, only elevated serum CA 19-9 correlated with survival—HR 6.1 (1.2–30.8), p = 0.03.
Subgroup analyses were performed for patients with T4a and T4b stage cancer. Survival in these patients stratified by nodal stage is presented in the supplementary figure 2. No significant correlation was found between the nodal stage and survival in T4a cancer. Elevated serum CA 19-9 was the only prognostic factor in these patients (data not shown). In T4b, nodal stage and adjuvant chemotherapy were significant prognostic factors in the univariable analysis (supplementary table 1). However, adjuvant chemotherapy was the only independent predictor for survival in the multivariable model.
Discussion
Our findings suggest that nodal stage has no prognostic impact in patients with LACC. Furthermore, parameters associated with the nodal status, such as number of harvested lymph nodes and lymph node ratio had no influence on survival. This is in contrast with Yamanashi and co-workers who distinguished lymph node ratio ≥ 0.06 as an independent predictor of overall and recurrence-free survival in T4 colon cancer [9]. One possible explanation could be that this study involved also patients with rectosigmoid cancer, while our report concerned exclusively those with colon cancer. Nevertheless, several reports focusing merely on T4 colon cancer suggest that presence of lymph nodes metastases and nodal stage are prognostic factors for survival (supplementary table 2). In this study, only preoperative CA 19-9 and adjuvant chemotherapy were significant predictors for survival in patients with T4a and T4b colon cancer, respectively. Aoki et al. have also reported association between CA 19-9 and survival in T4 colon cancer [7], while others have underscored the prognostic role of adjuvant chemotherapy [14,15,16]. Thus, in that vein, our findings seem to be in line with the literature.
Interestingly, most of these reports did not conduct subgroup analyses for patients with T4a and T4b cancer. As a result, prognostic factors were reported without differentiating for the subtypes of T4. In our view, such analysis is needed as T4a and T4b represent different stages of colon cancer requiring distinct treatment modalities. Therefore, current report has specifically focused on prognostic factors in T4a and T4b cancer.
A trend towards higher recurrence rate was observed in patients with positive lymph nodes. However, statistics were not calculated due to incomplete data. Klaver and co-workers suggest that N2 stage is associated with intraabdominal recurrence in patients with T4 colon cancer [15]. Furthermore, it has also been reported to result in peritoneal carcinomatosis [17]. Unfortunately, the quality of our data did not allow to investigate these correlations. Together with the retrospective design, incomplete data were the main limitations of this study. Another major drawback is that some specimens were inadequately examined for the lymph node yield, especially in the beginning of the study period. Since surgical technique and considerations on the extent of surgery have not changed throughout the study period, the quality of pathology examination has had a major influence on this parameter. Examination of at least 12 lymph nodes is recommended by the NCCN guidelines for colon cancer [18]. In our material, <12 lymph nodes were examined in nearly 40% of patients. Furthermore, the proportion of cases with positive lymph nodes was significantly higher when ≥12 lymph nodes were examined (66.7 vs. 45.2%, p = 0.01). Therefore, the risk of understaging in inadequately examined specimens remains considerable. At the same time, neither lymph node ratio nor detecting ≥12 lymph nodes were not associated with survival. This is in contrast with their prognostic role in stage I–III colon cancer [19].
Our study is among the largest single-center reports addressing prognostic factors in LACC (supplementary table 2), and presented 5-year survival rate of 51.9% is comparable with the literature data [20,21,22,23,24]. At the same time, most of these studies report both open and laparoscopic resections for LACC trying to address the oncologic adequacy of laparoscopic surgery in this setting. In our series, all procedures were performed via laparotomy. On one hand, it does not allow to understand the impact of surgical approach on the lymph node yield and disease prognosis. On the other hand, surgical approach and technique were uniform in all patients given that these were operated by one surgeon (AMS). This represents one of the strengths of our material.
Conclusions
This report found no association between the nodal stage and survival in non-metastatic locally advanced colon cancer. A trend towards higher incidence of distant metastases and peritoneal carcinomatosis was observed in patients with positive lymph nodes. Considering potential limitations of this study, standardized pathology examination should be in the focus of prospective registries aimed at examining the prognostic role of pathology findings in colon cancer.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386
Rosander E, Nordenvall C, Sjovall A, Hjern F, Holm T (2018) Management and outcome after multivisceral resections in patients with locally advanced primary colon cancer. Dis Colon Rectum 61(4):454–460
An MS, Yoo JH, Kim KH, Bae KB, Choi CS, Hwang JW, Kim J, Kim B, Kang M, Oh M, Hong K (2015) T4 stage and preoperative anemia as prognostic factors for the patients with colon cancer treated with adjuvant FOLFOX chemotherapy. World J Surg Oncol 13:64
Hashiguchi Y, Hase K, Ueno H, Mochizuki H, Shinto E, Yamamoto J (2011) Optimal margins and lymphadenectomy in colonic cancer surgery. Br J Surg 98(8):1171–1178
Yang ZF, Wu DQ, Wang JJ, Lv ZJ, Li Y (2018) Short- and long-term outcomes following laparoscopic vs open surgery for pathological T4 colorectal cancer: 10 years of experience in a single center. World J Gastroenterol 24(1):76–86
Kumamoto T, Toda S, Matoba S, Moriyama J, Hanaoka Y, Tomizawa K, Sawada T, Kuroyanagi H (2017) Short- and long-term outcomes of laparoscopic multivisceral resection for clinically suspected T4 colon cancer. World J Surg 41(8):2153–2159
Aoki T, Matsuda T, Hasegawa H, Yamashita K, Sumi Y, Ishida R, Yamamoto M, Kanaji S, Oshikiri T, Nakamura T, Suzuki S, Kakeji Y (2019) Outcomes of laparoscopic surgery for pathological T4 colon cancer. Int J Color Dis 34(7):1259–1265
Leon P, Iovino MG, Giudici F, Sciuto A, de Manzini N, Cuccurullo D, Corcione F (2018) Oncologic outcomes following laparoscopic colon cancer resection for T4 lesions: a case-control analysis of 7-years' experience. Surg Endosc 32(3):1133–1140
Yamanashi T, Nakamura T, Sato T, Naito M, Miura H, Tsutsui A, Shimazu M, Watanabe M (2018) Laparoscopic surgery for locally advanced T4 colon cancer: the long-term outcomes and prognostic factors. Surg Today 48(5):534–544
Leijssen LGJ, Dinaux AM, Amri R, Kunitake H, Bordeianou LG, Berger DL (2019) The impact of a multivisceral resection and adjuvant therapy in locally advanced colon cancer. J Gastrointest Surg 23(2):357–366
Sahakyan AM, Aleksanyan A, Batikyan H, Petrosyan H, Sahakyan M (2020) Standard and multivisceral colectomy in locally advanced colon cancer. Radiol Oncol 54(3):341–346
Weiser MR (2018) AJCC 8th edition: colorectal cancer. Ann Surg Oncol 25(6):1454–1455
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240(2):205–213
Teufel A, Gerken M, Hartl J, Itzel T, Fichtner-Feigl S, Stroszczynski C, Schlitt HJ, Hofstädter F, Klinkhammer-Schalke M (2015) Benefit of adjuvant chemotherapy in patients with T4 UICC II colon cancer. BMC Cancer 15:419
Klaver CEL, Wasmann K, Verstegen M, van der Bilt JDW, Nagtegaal ID, van Ramshorst B et al (2018) Postoperative abdominal infections after resection of T4 colon cancer increase the risk of intra-abdominal recurrence. Eur J Surg Oncol 44(12):1880–1888
Sebastian NT, Tan Y, Miller ED, Williams TM, Diaz DA (2020) Surgery with and without adjuvant radiotherapy is associated with similar survival in T4 colon cancer. Color Dis 22(7):779–789
van Santvoort HC, Braam HJ, Spekreijse KR, Koning NR, de Bruin PC, de Vries Reilingh TS, Boerma D, Smits AB, Wiezer MJ, van Ramshorst B (2014) Peritoneal carcinomatosis in t4 colorectal cancer: occurrence and risk factors. Ann Surg Oncol 21(5):1686–1691
Benson AB, Venook AP, Al-Hawary MM, Cederquist L, Chen Y-J, Ciombor KK, et al (2018) NCCN guidelines insights: colon cancer, Version 2.2018. 2018;16(4):359
Lykke J, Roikjaer O, Jess P (2013) The relation between lymph node status and survival in Stage I-III colon cancer: results from a prospective nationwide cohort study. Color Dis 15(5):559–565
Govindarajan A, Coburn NG, Kiss A, Rabeneck L, Smith AJ, Law CH (2006) Population-based assessment of the surgical management of locally advanced colorectal cancer. J Natl Cancer Inst 98(20):1474–1481
de'Angelis N, Vitali GC, Brunetti F, Wassmer CH, Gagniere C, Puppa G et al (2016) Laparoscopic vs. open surgery for T4 colon cancer: a propensity score analysis. Int J Color Dis 31(11):1785–1797
Takahashi R, Hasegawa S, Hirai K, Hisamori S, Hida K, Kawada K, Sakai Y (2017) Safety and feasibility of laparoscopic multivisceral resection for surgical T4b colon cancers: retrospective analyses. Asian J Endosc Surg 10(2):154–161
Lu J, Dong B, Yang Z, Song Y, Yang Y, Cao J, Li W (2019) Clinical efficacy of laparoscopic surgery for T4 colon cancer compared with open surgery: a single center’s experience. J Laparoendosc Adv Surg Tech A 29(3):333–339
Macari D, Kawak S, Raofi V, Wasvary H, Jaiyesimi I (2019) Recurrence pattern and outcomes in T4 colon cancer: a single institution analysis. J Surg Oncol 121:337–341. https://doi.org/10.1002/jso.25766
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Artur M. Sahakyan, Andranik Aleksanyan, and Mushegh A. Sahakyan. The first draft of the manuscript was written by Artur M. Sahakyan and Mushegh A. Sahakyan. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sahakyan, A.M., Aleksanyan, A., Batikyan, H. et al. Lymph Node Status and Long-Term Oncologic Outcomes After Colon Resection in Locally Advanced Colon Cancer. Indian J Surg 84, 79–85 (2022). https://doi.org/10.1007/s12262-021-02825-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-021-02825-y