Abstract
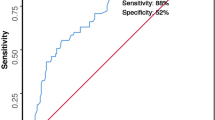
Perforated peptic ulcer represents the most frequent indication for emergency surgery for peptic ulcer disease. The mortality from perforated peptic ulcer remains up to 27%. We compare predictive score of mortality in perforated peptic ulcer (POMPP) scoring system with peptic ulcer perforation (PULP) score, Boey score, and American Society of Anesthesiologists (ASA) score to predict mortality. Hundred consecutive patients were operated for peptic perforation from May 2018 to May 2019 in our institute. For prediction of mortality, scoring was done by POMPP score, PULP score, Boey score, and ASA score. Comparative analysis of different score was done. Mean age was 40.7 years and male to female ratio was 32.3:1. Post-operative morbidity was 27% and mortality rate was 11%. Of the 10 patients of high POMPP score, 8 patients died (p value 0.000001) with accuracy of 80%. Receiver operating characteristic curve analysis showed that area under curve was 0.964 for POMPP score, 0.980 for PULP score, 0.960 for Boey score, and 0.906 for ASA score. The specificity of Boey score, POMPP score, and PULP score was 88.7%, 97.7%, and 100% respectively. Boey score had accuracy of 44.4% and PULP score had 100% accuracy in predicting mortality but it is complex with more number of components. POMPP score is based on objective data and its components are age and routinely measured values (blood urea nitrogen and serum albumin). It is simple and easily applicable scoring system for predicting mortality in peptic perforation peritonitis patients with accuracy of 80%.

Similar content being viewed by others
References
Wang YR, Richter JE, Dempsey DT (2010) Trends and outcomes of hospitalizations for peptic ulcer disease in the United States, 1993 to 2006. Ann Surg 251(1):51–58 [PubMed] [Google Scholar]
Lau JY, Sung J, Hill C, Henderson C, Howden CW, Metz DC (2011) Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality. Digestion 84(2):102–113 [PubMed] [Google Scholar]
Guzel H, Kahramanca S, Seker D, Ozgehan G, Tunc G, Kucukpinar T, Kargici H (2014) Peptic ulcer complications requiring surgery: what has changed in the last 50 years in Turkey? Turk J Gastroenterol 25(2):152–155 [PubMed] [Google Scholar]
Lohsiriwat V, Prapasrivorakul S, Lohsiriwat D (2009) Perforated peptic ulcer: clinical presentation, surgical outcomes, and the accuracy of the Boey scoring system in predicting postoperative morbidity and mortality. World J Surg 33:80–85. https://doi.org/10.1007/s00268-008-9796-1
Thorsen K, Søreide JA, Søreide K (2013) Scoring systems for outcome prediction in patients with perforated peptic ulcer. Scand J Trauma Resusc Emerg Med 21:25. https://doi.org/10.1186/1757-7241-21-25
Søreide K, Thorsen K, Harrison EM, Bingener J, Moller MH, Ohene-Yeboah M, Soreide JA (2015) Perforated peptic ulcer. Lancet 386(10000):1288–1298. https://doi.org/10.1016/S0140-6736(15)00276-7
Møller MH, Adamsen S, Thomsen RW, Moller AM (2011) Multicenter trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation. Br J Surg 98(6):802–810
Anand C, Shekhar H, Pratap V, Ali M (2018) Comparison of effectiveness of Boey score and PULP score in assessment of severity in peptic ulcer perforations: prospective study. IOSR J Dental Med Sci (IOSR-JDMS) 17(12):11–17
Gulzar JS, Paruthy SB, Arya SV (2016) Improving outcome in perforated peptic ulcer emergency surgery by Boey scoring. Int Surg J 3(4):2120–2128
So JBY, Yam A, Cheah WK, Kum CK, Goh PMY (2000) Risk factors related to operative mortality and morbidity in patients undergoing emergency gastrectomy. Br J Surg 87:1702–1707
Lunevicius R, Morkevicius M (2005) Systematic review comparing laparoscopic and open repair for perforated peptic ulcer. Br J Surg 92:1195–1207
Menekse E, Kocer B, Topcu R, Olmez A, Tez M, Kayaalp C (2015) A practical scoring system to predict mortality in patients with perforated peptic ulcer. World Journal of Emergency Surgery 10:7. https://doi.org/10.1186/s13017-015-0008-7
Kocer B, Surmeli S, Solak C, Unal B, Bozkurt B, Yildirim O, Dolapci M, Cengiz O (2007) Factors affecting mortality and morbidity in patients with peptic ulcer perforation. J Gastroenterol Hepatol 22:565–570
Lee FY, Leung KL, Lai BS, Ng SS, Dexter S, Lau WY (2001) Predicting mortality and morbidity of patients operated on for perforated peptic ulcers. Arch Surg 136:90–94
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20:250–278
Thorsen K, Søreide JA, Søreide K (2014) What is the best predictor of mortality in perforated peptic ulcer disease? A population-based, multivariable regression analysis including three clinical scoring systems. J Gastrointest Surg 18(7):1261–1268. https://doi.org/10.1007/s11605-014-2485-5
Kumar N, Sahu SK, Bedi KS (2017) Evaluation of mortality and morbidity in patients with secondary peritonitis using predictive score of mortality in perforated peptic ulcer. Int Surg J 4(8):2706–2709
Møller MH, Engebjerg MC, Adamsen S, Bendix J, Thomsen RW (2012) The peptic ulcer perforation (PULP) score: a predictor of mortality following peptic ulcer perforation. A cohort study. Acta Anaesthesiol Scand 56:655–662. https://doi.org/10.1111/j.1399-6576.2011.02609.x
Boey J, Wong J, Ong GB (1982) A prospective study of operative risk factors in perforated duodenal ulcers. Ann Surg 195:265–269
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved with ethical committee of our institute. Informed and written consent was taken from the patient.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gupta, S., Bansal, S., Rajpurohit, M. et al. Comparison of POMPP Scoring System with PULP Score, Boey Score, and ASA Scoring Systems to Predict Mortality in Peptic Perforation. Indian J Surg 83, 160–164 (2021). https://doi.org/10.1007/s12262-020-02351-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02351-3