Abstract
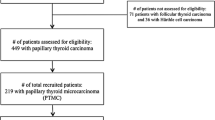
Despite the increased incidence of papillary thyroid microcarcinoma (PTMC), clinical importance is still controversial. Although risk factors for PTMCs have been identified previously, prognostic factors have not been established clearly. In this study, we aimed to review the presentation features and outcomes of the patients with PTMC. Our study included 144 patients that underwent thyroidectomy and were diagnosed with PTMC according to the postoperative pathology report. All data included age, gender, mode of diagnosis, preoperative ultrasonography and fine needle aspiration cytology (FNAC) results, tumor features (diameter, unilobar localization, multifocality, and stage), the presence of residual thyroid tissue, postoperative serum thyroglobulin (Tg) levels, and radioactive iodine (RAI) ablation were retrospectively reviewed. Only 29 patients (20%) with PTMC could be diagnosed preoperatively with FNAC which was performed in 67% of the patients. The diameter and the number of thyroid nodules were significantly related to the mode of diagnosis. The average size of the tumor diameter was 5 mm ± 2.87. An extrathyroidal extension (ETE) was observed in 10 patients (7%). Lymph node metastasis (LNM) was diagnosed in 6 patients (16%). There was a significant correlation between ETE and tumor diameter with LNM (p = 0.008 and p < 0.001, respectively). Residual tissue was noted in 110 patients (76%). The presence of residual thyroid tissue was significantly related to the extent of surgery, unilobar location, and multifocality. Mode of diagnosis (incidental or non-incidental), tumor diameter, the number of thyroid nodules, unilobar location, and multifocality seem to be related to unfavorable outcomes of patients with PTMC.

Similar content being viewed by others
References
Davies L, Welch HG (2014) Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg 140:317–322
Novosel T, Ritter HE, Gupta M, Harvey A, Mitchell J, Berber E, Siperstein A, Milas M (2009) Detection of circulating thyroid cancer cells in patients with thyroid microcarcinomas. Surgery 146:1081–1089
Du L, Wang Y, Sun X, Li H, Geng X, Ge M, Zhu Y (2018) Thyroid cancer: trends in incidence, mortality and clinical-pathological patterns in Zhejiang Province, Southeast China. BMC Cancer 18:291
Lombardi CP, Bellantone R, De Crea C, Paladino NC, Fadda G, Salvatori M, Raffaelli M (2010) Papillary thyroid microcarcinoma: extrathyroidal extension, lymph node metastases, and risk factors for recurrence in a high prevalence of goiter area. World J Surg 34:1214–1221
Grodski S, Delbridge L (2009) An update on papillary microcarcinoma. Curr Opin Oncol 21:1–4
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133
Zhao Q, Ming J, Liu C, Shi L, Xu X, Nie X, Huang T (2013) Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Ann Surg Oncol 20:746–752
Sakorafas GH, Giotakis J, Stafyla V (2005) Papillary thyroid microcarcinoma: a surgical perspective. Cancer Treat Rev 31:423–438
Lin JD, Huang BY, Chang HY (1998) Clinical experience in the diagnosis of 127 papillary thyroid microcarcinoma. Endocr Relat Cancer 5:239–245
Neuhold N, Schultheis A, Hermann M, Krotla G, Koperek O, Birner P (2011) Incidental papillary microcarcinoma of the thyroid--further evidence of a very low malignant potential: a retrospective clinicopathological study with up to 30 years of follow-up. Ann Surg Oncol 18:3430–3436
Slijepcevic N, Zivaljevic V, Marinkovic J, Sipetic S, Diklic A, Paunovic I (2015) Retrospective evaluation of the incidental finding of 403 papillary thyroid microcarcinomas in 2466 patients undergoing thyroid surgery for presumed benign thyroid disease. BMC Cancer 15:330
Noguchi S, Yamashita H, Uchino S, Watanabe S (2008) Papillary microcarcinoma. World J Surg 32:747–753
Wang TS, Goffredo P, Sosa JA, Roman SA (2014) Papillary thyroid microcarcinoma: an over-treated malignancy? World J Surg 38:2297–2303
Sugitani I (2018) Active surveillance for very low-risk papillary thyroid carcinoma: experience and perspectives from Japan. Ann Thyroid 3:26
Page C, Biet A, Boute P, Cuvelier P, Strunski V (2009) Aggressive papillary thyroid microcarcinoma. Eur Arch Otorhinolaryngol 266:1959–1963
Thomas RM, Habra MA, Perrier ND, Grubbs EG (2012) Well-differentiated carcinoma of the thyroid and neoplasms of the parathyroid glands. In: Feig BW, Ching CD (eds) The MD Anderson surgical oncology handbook, 5th edn. Lippincott Williams &Wilkins, Philadelphia, pp 550–587
Küçük NO, Tari P, Tokmak E, Aras G (2007) Treatment for microcarcinoma of the thyroid--clinical experience. Clin Nucl Med 32:279–281
Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, Matsuzuka F, Kuma K, Miyauchi A (2004) Papillary microcarcinoma of the thyroid: how should it be treated? World J Surg 28:1115–1121
Siddiqui S, White MG, Antic T, Grogan RH, Angelos P, Kaplan EL, Cipriani NA (2016) Clinical and pathologic predictors of lymph node metastasis and recurrence in papillary thyroid microcarcinoma. Thyroid 26:807–815
Pelizzo MR, Boschin IM, Toniato A, Pagetta C, Piotto A, Bernante P, Casara D, Pennelli G, Rubello D (2004) Natural history, diagnosis, treatment and outcome of papillary thyroid microcarcinoma (PTMC): a mono-institutional 12-year experience. Nucl Med Commun 25:547–552
Vlassopoulou V, Vryonidou A, Paschou SA, Ioannidis D, Koletti A, Klonaris N, Katsoulis K, Rontogianni D, Vasilopoulos C, Tsagarakis S, Tzavara I (2016) No considerable changes in papillary thyroid microcarcinoma characteristics over a 30-year time period. BMC Res Notes 9:252
Cheema Y, Olson S, Elson D, Chen H (2006) What is the biology and optimal treatment for papillary microcarcinoma of the thyroid? J Surg Res 134:160–162
Arora N, Turbendian HK, Kato MA, Moo TA, Zarnegar R, Fahey TJ 3rd (2009) Papillary thyroid carcinoma and microcarcinoma: is there a need to distinguish the two? Thyroid 19:473–477
Tzvetov G, Hirsch D, Shraga-Slutzky I, Weinstein R, Manistersky Y, Kalmanovich R, Lapidot M, Grozinsky-Glasberg S, Singer J, Sulkes J, Shimon I, Benbassat C (2009) Well-differentiated thyroid carcinoma: comparison of microscopic and macroscopic disease. Thyroid 19:487–494
Wada N, Duh QY, Sugino K, Iwasaki H, Kameyama K, Mimura T, Ito K, Takami H, Takanashi Y (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237:399–407
Zhang X, Zhang L, Xue S, Wang P, Chen G (2019) Predictive factors of lateral lymph node metastasis in solitary papillary thyroid microcarcinoma without gross extrathyroidal extension. Asian J Surg 42:563–570
Roti E, Rossi R, Trasforini G, Bertelli F, Ambrosio MR, Busutti L, Pearce EN, Braverman LE, Degli Uberti EC (2006) Clinical and histological characteristics of papillary thyroid microcarcinoma: results of a retrospective study in 243 patients. J Clin Endocrinol Metab 91:2171–2178
Lim DJ, Baek KH, Lee YS, Park WC, Kim MK, Kang MI, Jeon HM, Lee JM, Yun-Cha B, Lee KW, Son HY, Kang SK (2007) Clinical, histopathological, and molecular characteristics of papillary thyroid microcarcinoma. Thyroid 17:883–888
Chow SM, Law SC, Chan JK, Au SK, Yau S, Lau WH (2003) Papillary microcarcinoma of the thyroid-prognostic significance of lymph node metastasis and multifocality. Cancer 98:31–40
Cappelli C, Castellano M, Braga M, Gandossi E, Pirola I, De Martino E, Agosti B, Rosei EA (2007) Aggressiveness and outcome of papillary thyroid carcinoma (PTC) versus microcarcinoma (PMC): a mono-institutional experience. J Surg Oncol 95:555–560
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cayir, D., Kulah, B. & Bozkurt, M. Presentation and Outcomes of Papillary Thyroid Microcarcinomas. Indian J Surg 82, 533–539 (2020). https://doi.org/10.1007/s12262-019-02044-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-019-02044-6