Abstract
Asthma is a chronic inflammatory disease triggered by allergic reactions in the bronchia. These reactions lead to swelling of mucous membranes, hypersecretion of mucus, and bronchoconstriction, resulting in a restricted opening of the lung airway. Allergic pulmonary inflammation and airway hyperresponsiveness are induced when Th2 cytokines, such as interleukin (IL)-4 and IL-13, bind to their cognate receptors on lung epithelial cells. Specifically, IL-13 stimulates inflammation through a multi-subunit receptor, mainly the alpha chain of the IL-4 receptor (IL-4Rα), which also plays a role in IL-4 signaling. In this study, we employed a lung epithelial cell-targeting siRNA carrier composed of a rabies virus glycoprotein-derived small peptide coupled with cationic nona-arginine and trileucine before cysteine peptide (RVG9R3LC). This carrier was complexed with siRNA, enabling targeted delivery of therapeutic siRNA to IL-4Rα (siIL4Rα) expressed in lung epithelial cells within an asthma model in vivo. Our approach demonstrated efficient gene knockdown in cultured lung epithelial cells and in vivo. Furthermore, two administrations of therapeutic siIL4Rα protected the ovalbumin-sensitized and challenged asthma mouse model from airway inflammation and excessive mucus secretion. Our findings suggest that the peptide-siRNA carrier system presents a promising therapeutic approach for respiratory inflammation.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Asthma is a chronic inflammatory disease caused by allergic inflammatory reactions in the bronchia, leading to bronchoconstriction, swelling of mucous membranes, hypersecretion of mucus, and a restricted opening of the lung airway [1]. Asthma pathogenesis is associated with an imbalance in immune responses of the T-helper cells Th1 and Th2 [2, 3]. In asthma, the overproduction of Th2 cytokines, such as interleukin (IL)-4 and IL-13, plays a significant role in promoting allergic inflammation [4]. Patients with asthma exhibit elevated levels of IL-4 and IL-13 in both lung tissues and serum [5]. The convergence of IL-4 and IL-13 signaling pathways presents an opportunity to simultaneously inhibit the inflammatory actions caused by both IL-4 and IL-13 [6]. The type II interleukin-4 receptor alpha (IL-4Rα) serves as a crucial intermediary subunit for receptor binding by both IL-4 and IL-13, leading to the induction of a Th2 cytokine response [7]. Ligand binding to the IL-4Rα initiates the recruitment and phosphorylation of the STAT6 transcription factor, triggering various intracellular signaling cascades. Subsequently, phosphorylated STAT6 activates genes responsive to IL-4 and IL-13, contributing to Th2 responses, immunoglobulin E (IgE) switching, the development of airway hyperresponsiveness (AHR), and mucus production [8, 9].
The therapeutic potential of IL-4Rα inhibition becomes evident based on findings from IL-4Rα genetic ablation studies [10]. Genetic ablation of IL-4Rα or inhalation of IL-4Rα antisense oligonucleotides has shown to mitigate allergen-induced AHR, goblet cell metaplasia, and suppress airway eosinophilia and neutrophilia [11, 12]. Additionally, dupilumab, an FDA-approved humanized monoclonal antibody targeting IL-4Rα, has demonstrated significant improvement in lung function with reduced production of the total IgE in patients with severe asthma [13, 14]. These studies underscore the potential therapeutic value of targeting IL-4Rα signaling to ameliorate airway inflammation and mucus secretion in patients with allergic asthma.
The coronavirus disease 2019 (COVID-19) pandemic has underscored the urgent demand for a novel pulmonary drug delivery system that cater to millions of infected individuals worldwide. Beyond safeguarding against viral infection, the regulation of the inflammatory response has shown a high correlation with the prognosis and severity of COVID-19 infection [15, 16]. Numerous studies have reported various effective therapeutic gene delivery methods, demonstrating successful prevention of lung damage caused by respiratory diseases and minimization of after-effects resulting from abnormal gene functioning, thereby improving overall patient care [17, 18]. Currently, chemically modified dimeric siRNAs can be administered intranasally to effectively enter the lungs and achieve degradation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), including delta and omicron variants [19]. This technology can be adapted to address other pulmonary diseases, such as pulmonary fibrosis and respiratory viruses.
The delivery of genes to an intact airway epithelium encounters formidable challenges, including physical barriers, such as mucins and surfactants, and immunologic barriers, such as innate immune responses, which collectively impede gene penetration into cells [20, 21]. This predicament may result in the entrapment of the therapeutic gene in the mucus layer, rendering it susceptible to mucociliary clearance [22]. The presence of anionic molecules in mucus further hampers the efficacy of nucleic acid-based drugs (DNA and siRNA) by disrupting nucleic acid-carrier complexes [23]. Additionally, inhaled therapeutic genes are cleared by airway surface liquid and obstructed by glycocalyx, hindering their interaction with the intended receptors for endocytosis [24, 25]. The size of the delivery particles is a critical factor in this process. Small aerosol droplets (100–200 nm) are adept at targeting the alveolar region, whereas larger droplets (4 μm) are deposited in the tracheobronchial region [23]. To achieve optimal in vivo therapeutic effects and enhance siRNA deposition in the airway epithelium, it is crucial that the delivered nanoparticles should have a nanosize range. While liposomes have demonstrated efficacy in treating airway inflammation, specific delivery to the lung epithelium through cell surface receptors proves to be more efficient for siRNA than for liposomes [26,27,28].
Receptor-mediated gene delivery systems have been extensively investigated over the past few decades. Numerous studies have explored ligand-targeting receptors expressed in the lung epithelium to deliver therapeutic genes [29,30,31,32,33]. In our previous studies, we employed a rabies virus glycoprotein (RVG)-derived small peptide coupled with nona-arginine, a cationic cell-penetrating peptide, to deliver siRNA to distinct cell types expressing nicotinic acetylcholine receptors (nAchR) on their surface [34, 35]. Additionally, the terminal linking of a hydrophobic trileucine residue to the RVG9R3LC:siRNA complexes, hereafter referred to as RVG9R, enhances endosomal escape and leads to efficient siRNA translocation into the cytoplasm [36].
In this study, we observed widespread expression of nAchR in the lung epithelium, and intratracheal administration of RVG9R facilitated siRNA deposition in the lung. Furthermore, we assessed the therapeutic effectiveness of delivering siRNA targeting IL-4Rα specifically to lung epithelial cells, a component of both IL-4 and IL-13. Our findings confirm that peptide-mediated binding to nAchR expressed in the lung epithelial cells results in efficient siRNA delivery, inducing more pronounced silencing effects. Therefore, targeted delivery of siRNA to epithelial cells by RVG9R holds promise for RNA interference (RNAi) therapy in asthma.
2 Materials and methods
2.1 Peptides and siRNAs
RVG9R and RVM9R peptides were synthesized by Peptron, and their sequences are depicted [34, 36]. siRNA targeting murine IL-4Rα (5’-GGAGGAAGAAGAUGAGAUA-3’) and human CD4 (5’-GAUCAAGAGACUCCUCAGUTT-3’) were synthesized by ST Pharm. FITC-labeled siRNA (siFITC) or Cy5-labeled siRNA (siCy5) with the sequence 5’-CUUACGCUGAGUACUUCGAdTdT-3’ targeted the firefly luciferase mRNA [36].
2.2 Cell culture and transfection
The murine lung epithelial cell line (MLE-12) from ATCC was cultured in Dulbecco's modified Eagle medium supplemented with 10% fetal bovine serum, penicillin (100 IU/mL) and streptomycin (100 μg/mL). Peptide:siRNA complexes were formed at various molar ratios in 200 µL of serum-free Dulbecco's modified Eagle medium and incubated for 15 min before transfection in 12-well plates. For cellular uptake assays, 100 pmol siFITC was used. Lipofectamine 2000 (Invitrogen) served as the transfection control, following the manufacturer’s instructions.
2.3 Immunocytochemistry
To confirm the expression of nAchR or IL-4Rα, MLE-12 cells were grown on coverslips. Subsequently, the cells were blocked with phosphate-buffered saline (PBS) containing 1% bovine serum albumin and 0.05% Tween 20 for 2 h at 37 °C. Following the blocking step, the cells were stained with rabbit anti-nAchR α7 primary antibody (1:200, ab10096; Abcam) or rabbit anti-IL-4Rα primary antibody (1:200, ab203398; Abcam) overnight at 4 °C in a dark humidified chamber. The cells were then washed three times with PBS (0.05% Tween 20) and stained with a FITC conjugated anti-rabbit secondary antibody (1:200, ab97050; Abcam) for 2 h at 4 °C in the dark. Finally, nuclei were counterstained with Hoechst 33,342 and mounted using an aqueous mounting solution (Abcam). Fluorescent signals were captured using a confocal microscope (TSP-SP5; Leika).
2.4 Cytotoxicity assay
Cell viability was analyzed using the CCK-8 assay (Dojindo Laboratories), according to the manufacturer’s instructions, 24 h post-transfection with 100 pmol of siRNA at various peptide:siRNA molar ratios.
2.5 Biodistribution of Cy5-labeled siRNA
To examine the distribution of siRNA in the lung tissues, 200 pmol of siCy5 precomplexed with RVG9R at a 20:1 peptide:siRNA ratio was intratracheally administered using MicroSprayer (PennCentury) at a final volume of 100 µL with PBS. The lungs were excised at 0, 12, 24, 48, 60, and 72 h post inoculation, washed with cold PBS, and examined for fluorescence signals using Molecular Imaging System (Kodak). Additionally, 20 μm-thick frozen sections were prepared at each time point, with nuclei counterstained using Hoechst 33342. Fluorescent signals in the cells were captured using a confocal laser microscope (Leica).
2.6 Analysis of gene silencing
For quantitative PCR, total RNA was extracted from peptide:siRNA transfected cells (100 pmol siRNA) at a 20:1 peptide:siRNA ratio, using an RNAiso kit (Takara). Harvested total RNA was reverse transcribed using the iScript™ cDNA synthesis kit (Bio-Rad) and quantified using the SYBR Fast qPCR kit (Kapa Biosystems) on a 7500 Fast Real-Time PCR system (Applied Biosystems). Murine IL-4Rα, MUC5AC, TNFα, STAT6, IFN-γ and NF-kB mRNA levels were quantified with the appropriate primer sets and normalized to the murine GAPDH levels.
IL-4Rα: forward primer, 5’-TCCCATTTTGTCCACCGAATA-3’; reverse primer, 5’-GTTTCTAGGCCCAGCTTCCA-3’.
MUC5AC: forward primer, 5’-CCTACCTGCCGCTTCCTCT-3’; reverse primer, 5’-GGGCCTCTCCTACCTCCAAG-3’.
TNFα: forward primer, 5’-CAGGCGGTGCCTATGTCTC-3’; reverse primer, 5’-CGATCACCCCGAAGTTCAGTAG-3’.
STAT6: forward primer, 5’-CTCTGTGGGGCCTAATTTCCA-3’; reverse primer, 5’- CATCTGAACCGACCAGGAACT-3’.
IFN-γ: forward primer, 5’-ACAGCAAGGCGAAAAAGGATG-3’; reverse primer, 5’- TGGTGGACCACTCGGATGA-3’.
NF-kB: forward primer, 5’- CTGGGCACCAGTTCGATGG-3’; reverse primer, 5’- GACAGCATAAGGCACACACTT-3’.
2.7 Ovalbumin (OVA)-induced asthma model and treatment
Female BALB/c mice (20–25 g) were used to establish an OVA-induced asthma model. Mice were sensitized with intraperitoneal injection (i.p.) of OVA (100 µg, Sigma-Aldrich) and aluminum hydroxide (4 mg, Pierce) reconstituted in 20 µL PBS on day 0 and day 14. Intranasal challenge with OVA (1.5 mg) was performed on days 15–17 post-initial sensitization. For in vivo therapeutic effects, mice were intratracheally inoculated with 200 pmol of siRNA at a 20:1 peptide:siRNA ratio at a final volume of 100 µL with PBS. The sham group was sensitized and challenged with PBS without OVA and aluminum hydroxide. All the procedures were performed in accordance with the guidelines and protocols approved by the Institute of Animal Care and Use Committee of Hanyang University (2013-0144A).
2.8 Histology and immunohistochemistry
Paraffin-embedded lung tissue sections were deparaffinized and rehydrated before periodic acid-Schiff (PAS) staining using a standard protocol. Coverslips were applied to the PAS-stained sections, and a blind analysis was performed using light microscopy. For immunohistochemistry, the sections were heat-inactivated with prewarmed antigen retrieval buffer (10 mM sodium citrate, 0.05% Tween-20 (w/v), pH 6.0) for 25 min at 95 °C, followed by cooling at room temperature for 20 min. Subsequently, sections were blocked with Tris-buffered saline with Tween 20 (TBST) containing 1% bovine serum albumin and 10% goat serum for 1 h at 37 °C. Overnight incubation at 4 °C was conducted using a rabbit anti-nAchR α7 primary antibody (1:200, ab10096; Abcam, Cambridge, UK). The sections were washed with TBST and incubated for 2 h with a HRP conjugated goat anti-rabbit IgG secondary antibody (ab6721, 1:10,000; Abcam). The sections were developed using a 3,3' diaminobenzidine substrate (GE Healthcare) and counterstained with hematoxylin (Sigma-Aldrich).
2.9 Airway hyperresponsiveness
On day 18, AHR was measured 24 h after the last OVA challenge by inducing bronchoconstriction with increasing doses of methacholine. The enhanced pause (Penh) in unrestrained mice was estimated using a whole-body plethysmograph as a measure of AHR (All Medicus Co.). AHR was assessed in all the tested mice.
2.10 Serum immunoglobulin G assay
Serum collected from all tested groups was used to measure the total IgG level using an IgG mouse ELISA kit (Abcam), following the manufacturer’s instructions. The IgG concentration in the serum was determined by measuring the absorbance at 450 nm.
2.11 Bronchoalveolar lavage (BAL) fluid collection and cell number counting
BAL was collected from anesthetized mice by instilling and withdrawing cold saline through the trachea using a 24G catheter (BD Bioscience) connected to a 1 mL syringe. BAL was obtained by centrifugation at 1,000 × g at 4ºC. Differential cell counts of 500 cells from cytospin preparation were stained with Diff-Quik (Sysmex) and blindly counted by three individuals.
2.12 Statistical analysis
Statistical analysis of data in this study was conducted using the Mann–Whitney U-test to assess differences in mean values between any two groups and a one-way ANOVA to assess differences in mean values among more than two groups using the GraphPad Prism 5 software. A significance level of p < 0.05 was considered statistically significant.
3 Results
3.1 RVG9R demonstrates efficient delivery of siRNA to lung epithelial cells
In a previous study, we demonstrated effective delivery of siRNA into neuronal cells expressing nAchR using the RVG fusion peptide, RVG, and cationic cell penetrating nona-arginine (9R), along with trileucine-delivered siRNA [36]. In this study, we extended our investigation to specifically target siRNA delivery to lung cells. Initially, we assessed the expression of nAchR in cultured lung epithelial MLE-12 cells. Confocal microscopy revealed prevalent nAchR expression in lung epithelial cells (Fig. 1A). Subsequently, we investigated whether nAchR expressed by lung epithelial cells could facilitate siRNA delivery using RVG9R peptide. Flow cytometry data of the transfected siFITC revealed substantial fluorescence associated with cells when RVG9R was employed, as shown in the representative histograms, in contrast to the scrambled RVM9R peptide (Fig. 1B, upper panel). The percentage of transfected cells and mean fluorescence intensity significantly increased at the 20:1 peptide:siRNA ratio compared with the other ratios tested (Fig. 1B, lower panel). To ensure that the RVG9R:siRNA complexes did not compromise cell membrane integrity, cytotoxicity was assessed using the CCK-8 assay. The toxicity data indicated that the RVG9R:siRNA complexes were nontoxic to cultured lung epithelial cells at all tested ratios (Fig. 1C). Our findings suggest that RVG9R effectively delivers siRNA to cultured nAchR-expressing lung epithelial cells.
RVG9R enhances siRNA uptake in the lung epithelial cells. A Expression of nicotinic acetylcholine receptor (nAchR) in MLE-12 cells. Representative confocal laser microscopy images depicting nAchR expression (FITC, green) and Hoechst-stained nuclei (blue) and their colocalization (merge). Scale bar: 20 μm. B Cellular uptake of siRNA. Flow cytometry analysis of MLE-12 cells 24 h post exposure to various concentrations of peptide:siFITC complexes. Representative histograms (upper panel) and cumulative data for siFITC transfection efficiency presented as percent cells (lower panel, left) and mean fluorescence intensity (MFI; lower panel, right). C Cellular toxicity. Cytotoxicity assessed by CCK-8 viability assay 24 h post transfection of MLE-12 cells with peptide:siRNA complexes at the indicated molar ratio using 100 pmol of siRNA. Error bars represent the mean standard deviation of three independent experiments. Statistical significance is denoted as *p < 0.05, **p < 0.01, ***p < 0.001, and ns indicates not significant. LMN: Lipofectamine 2000, siFITC: siRNA labeled with FITC
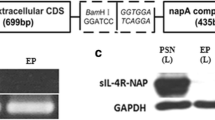
3.2 RVG9R successfully delivers functional siRNA to cultured lung epithelial cells
Prior to evaluating the functional silencing effect mediated by RVG9R:siRNA targeting IL-4Rα, we examined the expression of IL-4Rα in cultured lung epithelial cells. Confocal microscopy data demonstrated the presence of IL-4Rα on lung epithelial cells (Fig. 2A). For targeting the IL-4Rα gene, lung epithelial cells were transfected with 100 pmol of siRNA complexed with RVG9R, with siIL4Rα at a 20:1 peptide:siRNA molar ratio. Our results demonstrated maximum gene silencing of approximately 55% and 45% after 24 and 48 h, respectively. In contrast, the scrambled peptide and siRNA targeting the luciferase gene (negative control) did not exhibit any gene silencing effects (Fig. 2B). Therefore, our findings indicate that RVG9R effectively delivers siRNA specifically to cultured lung epithelial cells, resulting in a reduced mRNA expression level of IL-4Rα.
Effective delivery of functional siRNA to the lung epithelial cells using RVG9R. A Expression of interleukin-4 receptor alpha (IL-4Rα) in MLE-12 cells. Representative confocal laser microscopy images illustrating IL-4Rα expression (FITC, green) and Hoechst-stained nuclei (blue) and their co-localization (merge). Scale bar: 20 μm. B qPCR analysis of murine IL-4Rα mRNA levels in MLE-12 cells treated with peptide:siIL4Rα complexes at various hours post transfection with 100 pmol of siRNA at a 20:1 molar ratio. Relative gene expression is quantified against GAPDH mRNA level. Error bars represent the mean standard deviation of three independent experiments. Statistical significance is denoted as *p < 0.05, **p < 0.01, and ns indicates not significant. LMN: Lipofectamine 2000, siIL4Rα: siRNAs targeting IL-4 receptor α chain
3.3 RVG9R facilitates the delivery of functional siRNA to the lung in vivo
To utilize RVG9R as a carrier, we initially demonstrated the expression of nAchR in mouse lung tissues using immunohistochemistry. Microscopic data revealed prevalent expression of nAchR in the lung epithelial cells, suggesting the potential of RVG9R as an siRNA carrier in the lungs (Fig. 3A). Subsequently, we examined the distribution of fluorescence-labeled siRNA in mouse lungs at various time points (12, 24, 48, 60, and 72 h) following a single intratracheal dose of RVG9R:siRNA complexes (totaling 2.6 µg siRNA). This led to siRNA deposition in the lungs, with maximal delivery observed at 24 h, which persisted at detectable levels until 72 h (Fig. 3B). In contrast, siRNA delivered by the scrambled RVM9R peptide was cleared as early as 24 h. Confocal microscopy images of the lung cryosections at the 72-h time point confirmed the presence of Cy5-siRNA, consistent with our biodistribution data (Fig. 3C). Our data suggest that RVG9R targets lung epithelial cells and effectively delivers siRNA before degradation in the mucus. We then assessed the silencing efficiency of functional siRNA in the lung by targeting IL-4Rα expressed in the lung tissues [37]. To achieve maximal gene silencing, we administered 200 pmol (2.6 µg) of siRNA daily for two days, collecting samples at 12, 24, 48, and 72 h. Consistent with our gene delivery data, we achieved a maximal gene silencing effect at 24 and 48 h post inoculation (Fig. 3D). At 12 h, there was approximately 30% gene knockdown, compared to 55%, 51%, and 45% at 24 h, 48 h, and 72 h, respectively (Fig. 3D). These findings indicate that RVG9R can effectively deliver functional siRNA to the lungs, making it a promising carrier system for the treatment of lung-associated diseases.
Effective in vivo delivery of functional siRNA to the lung using RVG9R. A Expression of nicotinic acetylcholine receptor (nAchR) in mouse lung tissues. Representative images display 3,3' diaminobenzidine-stained nAchR in the epithelial cell layer and bronchiole (n = 3 per group). Scale bar: 100 μm. B Biodistribution of intratracheally inoculated peptide:siCy5 at 20:1 molar ratio with 200 pmol of siRNA (n = 6 per group). Examination of siCy5 presence in the lung. Representative lung images (left) and cumulative data (right) illustrating relative fluorescence intensity ± SD measured in arbitrary pixels from indicated test cohorts. C Confocal laser microscopic images of lung cryosections. Representative images showcasing the localization of siCy5 (red) and Hoechst-stained nuclei (blue). Scale bar: 100 μm. D qPCR analysis of murine IL-4Rα mRNA levels in mouse lung at indicated time points post inoculation with a total of 400 pmol of siRNA at 20:1 peptide:siIL4Rα molar ratio (n = 6 per group). Relative gene expression is quantified against GAPDH mRNA level. Error bars represent the mean standard deviation. Statistical significance is denoted as *p < 0.05, **p < 0.01, ***p < 0.001, and ns indicates not significant. siCy5: siRNA labeled with Cy5
3.4 RVG9R:siRNA administration does not elicit a lung inflammatory response
We further investigated whether the RVG9R:siRNA complex could elicit an inflammatory response in the lungs. Mice were treated once daily with RVG9R:siRNA for three days (2.6 µg). We performed qPCR to examine the expression of inflammation-related genes in the lung tissues 24 h after the last treatment. The analysis revealed that the RVG9R:siRNA complex did not trigger any inflammation-related genes, as evidenced by the lack of change in TNF-α, IFN-γ, STAT-6, and NF-kB gene levels compared with those of lipopolysaccharides-treated mice (Fig. 4). Our data highlight that the RVG9R:siRNA complex can be safely employed as a gene carrier system for asthma treatment, with minimal adverse inflammatory responses.
Absence of lung inflammatory response in RVG9R:siIL4Rα-treated mice. qPCR analysis of murine TNF-α, STAT6, IFN-γ, and NF-kB mRNA expression levels in mouse lungs inoculated with 200 pmol of peptide:siIL4Rα at 20:1 molar ratio (n = 6 per group). Relative gene expression is quantified against GAPDH mRNA levels. The error bars represent the mean standard deviation. Statistical significance is denoted as **p < 0.01, ***p < 0.001, and ns indicates not significant. LPS: lipopolysaccharides, siIL4Rα: siRNAs targeting IL-4 receptor α chain
3.5 RVG9R:siIL4Rα treatment diminishes airway hyperresponsiveness development and alleviates histological damage in asthma
To assess the therapeutic efficacy of RVG9R:siIL4α in an OVA-induced asthma model, BALB/c mice underwent sensitization and challenge with OVA to induce asthma [38]. The mice were subjected to OVA sensitization (i.p., OVA 12.5 µg + aluminum hydroxide 2.5 mg, day 0). The first treatment of 2.6 µg RVG9R:siIL4α was administered intratracheally using microsprayer on day 13, followed by the second OVA sensitization (i.p.) on day 14, with the same siRNA dose for the second treatment on day 15. Subsequently, OVA challenges (intranasal, 0.3 mg) were performed on day 16 and 17. The effects on AHR development and histological changes were examined on day 18 (Fig. 5A). Airway responsiveness to aerosolized methacholine was measured using barometric whole-body plethysmography in a conscious, spontaneous breathing state [39]. OVA sensitization and challenge increased airway reactivity, whereas RVG9R:siIL4α treatment group displayed reduced AHR compared with that of the OVA-sensitized and challenged group (OVA) or that of the control group (RVM9R:siIL4α or RVG9R:siLuci) (Fig. 5B). The impact of IL-4α silencing on mucus overproduction in OVA-sensitized and challenged mice were also observed. The Th2 cytokines, IL-4 and IL-13, induced excess mucus production in response to OVA. Specifically, IL-4 induced mucin gene expression, leading to mucus hypersecretion, whereas IL-13 activated mucus-secreting goblet cells in the airway epithelium [40, 41]. The mRNA expression of the mucin family MUC5AC gene was significantly elevated in the OVA-sensitized and OVA-challenged groups. In contrast, mice treated with RVG9R:siIL4α showed a significant reduction in MUC5AC expression in the lung, whereas non-targeted control siRNA had no effect (Fig. 5C). Histopathological changes and goblet cell hyperplasia were assessed using PAS staining [42]. In an OVA-induced asthma mouse model treated with PBS, noticeable goblet cell hyperplasia was observed as depicted through the presence of PAS-stained positive cells in the airways. In contrast, administration of RVG9R:siIL4α resulted in a reduction in the number of PAS-stained positive cells, indicating an attenuation of goblet cell hyperplasia (Fig. 5D). Our data indicate that treatment with RVG9R:siIL4α improves AHR development, reduces mucus overproduction, and attenuates goblet cell hyperplasia resulting from OVA sensitization and challenge in the asthma model.
Attenuation of airway hyperresponsiveness (AHR) development and histological changes by RVG9R:siIL4Rα in OVA-induced asthma model. A Methacholine-induced AHR in OVA-induced asthma model (n = 6 per group). B Enhanced pause (Penh) measured during inhalation indicating the dose of methacholine in the indicated animal groups. C qPCR analysis of murine Muc5AC mRNA level in the lungs of OVA-induced asthma model (n = 6 per group). Relative Muc5AC gene expression is quantified against GAPDH mRNA level. D Lung histology of OVA-induced asthma model (n = 6 per group). Representative microscopy images of alveoli and surrounding tissues after periodic acid-Schiff (PAS) staining. The scale bar represents 100 μm. In all cases, a total of 400 pmol of peptide:siRNA at 20:1 molar ratio was used. The error bars represent the mean standard deviation. Statistical significance is denoted as **p < 0.01, ***p < 0.001, and ns indicates not significant. siLuci: siRNAs targeting firefly luciferase, siIL4Rα: siRNAs targeting IL-4 receptor α chain, OVA: ovalbumin, MCh: methacholine
3.6 RVG9R:siIL4Rα treatment reduces inflammatory cells in BAL in an asthma mouse model
OVA sensitization and challenge induce OVA-specific serum IgE levels in a mouse model of asthma [43]. In our study, a significant increase in serum IgG levels was observed in OVA-sensitized and OVA-challenged mice compared with that of sham mice. However, mice treated with RVG9R:siIL4α exhibited a notable inhibition in serum IgG secretion (Fig. 6A). Subsequently, we investigated changes in the type and total number of inflammatory cells in the airways of OVA-sensitized and OVA-challenged mice. BAL analysis revealed a significant increase in the number of total infiltrated cells (80 ± 12 × 104 cells/mL) in OVA-sensitized mice compared with that in sham mice (21 ± 5 × 104 cells/mL). Neither the scrambled peptide nor the control siRNA reduced immune cell infiltration. In contrast, treatment with RVG9R:siIL4α resulted in a substantial decrease in the total number of infiltrated cells to 51 ± 7 × 104 cells/mL (Fig. 6B). The inflammatory cell types in BAL fluid of OVA-sensitized and challenged mice mainly consisted of macrophages (51 ± 8 × 104 cells/mL), followed by eosinophils (35 ± 13 × 104 cells/mL), with a modest increase in neutrophils (17 ± 4 × 104 cells/mL) and lymphocytes (1.2 ± 0.7 × 104 cells/mL) (Fig. 6C). In contrast to OVA-sensitized and challenged mice, RVG9R:siIL4α-treated group had significantly fewer macrophages, eosinophils, neutrophils, and lymphocytes (31 ± 7 × 104 cells/mL, 40 ± 3 × 104 cells/mL, 8 ± 2 × 104 cells/mL, and 0.5 ± 0.3 × 104 cells/mL, respectively) (Fig. 6C). Our data demonstrate that IL-4Rα silencing inhibits OVA-induced serum IgG secretion and reduces the number of inflammatory cells in BAL fluid, suggesting its potential therapeutic effect in asthma.
Reduction of pulmonary inflammation by RVG9R:siIL4Rα in OVA-induced asthma model. A Quantification of serum IgE in OVA-induced asthma model (n = 6 per group). Serum IgE level (ng/mL) quantified in each indicated animal group. B Total infiltrating cell count in OVA-induced asthma model (n = 6 per group). Lung lavage was performed, and differential cell count in BAL fluid was assessed. C–F Leukocytes infiltrating cell counts in OVA-induced asthma model (n = 6 per group). The macrophages (C), eosinophils (D), neutrophils (E), and lymphocytes (F) were counted in BAL fluid of indicated animal groups. In all cases, a total of 400 pmol of peptide:siRNA at 20:1 molar ratio was used. The error bars represent the mean standard deviation. Statistical significance is denoted as *p < 0.05, **p < 0.01, and ns indicates not significant. siLuci: siRNAs targeting firefly luciferase, siIL4Rα: siRNAs targeting IL-4 receptor α chain, OVA: ovalbumin, BAL: bronchoalveolar lavage
4 Discussion
Airway diseases, such as asthma, are commonly managed with symptomatic relief drugs, such as corticosteroids and beta 2 agonists, which provide temporary alleviation without a cure [44, 45]. This study explores RNAi targeting IL-4Rα, a shared receptor for IL-4 and IL-13 cytokines in asthma. IL-4Rα plays a crucial role in AHR development, as evidenced by our experimental data and previous studies [46,47,48]. Our approach, utilizing RVG9R:siIL4Rα to knock down IL-4Rα, effectively attenuated airway inflammation, AHR, goblet cell metaplasia, mucus secretion, and inflammatory immune cells in the OVA-induced asthma model.
Local pulmonary delivery of siRNA can be an effective approach to minimize systemic side effects and enhance lung retention time for treating diseases, such as asthma [49]. However, a lack of biocompatible lung cell-specific siRNA carriers limits the clinical efficacy of targeted gene delivery. RVG9R demonstrates promise as an siRNA carrier to the lungs, effectively addressing these challenges. Various targeted gene delivery approaches have been proposed for the treatment of chronic airway diseases, including ligand-based delivery and encapsulation within liposomes [50]. Although some methods have been successful, they lack cell specificity or require a targeting moiety [51,52,53,54]. In contrast, RVG9R:siRNA complex specifically recognizes cell surface receptors (nAchR) expressed in the lung epithelial cells, ensuring precise delivery to target cells. In addition to the targeted delivery system, the size of nanoparticles is crucial for achieving optimal siRNA delivery and therapeutic efficacy. Our previous study demonstrated that the RVG9R:siRNA complex falls within the nano-size range, measuring approximately 165 ± 8 nm, with an acceptable polydispersity index.
Comparing our approach to recent studies, such as the study by Hariharan et al. [19] on SARS-CoV-2, both employed lung delivery methods. However, our emphasis was on the specific delivery of siRNA to receptor-expressing cells in the lungs, exploiting nAChR enrichment in various lung epithelial cell types [55]. Studies using Clara cell-specific IL-4Rα knock-out transgenic mice highlighted protection from allergen-induced mucus production. However, our approach utilizing RVG9R for siRNA delivery to the lung epithelial cells broadens the spectrum, allowing target gene silencing in multiple cell types, resulting in attenuated hyperreactivity and mucin gene production [56].
Targeted siRNA delivery to the lung epithelium ensures specificity, precise testing of siRNA efficacy, and prevention of unwanted side effects. Additionally, RVG9R prevents inflammatory responses associated with cationic liposomes, demonstrating its safety [57]. By delivering siRNA through nAchR, our approach minimizes the need for repeated siRNA inoculation and demonstrates the absence of associated inflammation, positioning it as an effective and safe treatment strategy for asthma.
5 Conclusion
Our study highlights the efficacy of RVG9R in selective delivery of siRNA to the lung epithelium. This targeted delivery system proves highly effective in safeguarding the lung against OVA-induced airway inflammation and AHR development by specifically targeting IL-4Rα. The RVG9R:siRNA approach holds promise not only for addressing allergic responses, such as those induced by OVA, but also for potential applications in mitigating pulmonary damage stemming from infections, such as SARS-CoV-2. Furthermore, the versatility of this targeted approach extends its potential utility beyond allergic responses and encompasses a spectrum of inflammatory conditions. Chronic obstructive pulmonary disease, rhinitis, and pulmonary fibrosis, all associated with inflammation, are potential candidates for the therapeutic application of RVG9R-mediated siRNA delivery. Our findings open new avenues for exploring this approach in diverse pulmonary pathologies, offering a targeted and effective strategy for treating conditions characterized by inflammation.
Data availability
Raw data for this manuscript is available upon reasonable request to corresponding author.
References
Lambrecht BN, Hammad H (2015) The immunology of asthma. Nat Immunol 16:45–56. https://doi.org/10.1038/ni.3049
Wu Q, Tang Y, Hu X et al (2016) Regulation of Th1/Th2 balance through OX40/OX40L signalling by glycyrrhizic acid in a murine model of asthma. Respirology 21:102–111. https://doi.org/10.1111/resp.12655
Li S, Han F, Liu C et al (2023) Rapid screen of IL-5/IL-5Rα blocking antibodies in the HEK293-IL-5Rα-CSF2RB transfected cell line. Biotechnol Bioprocess Eng 28:612–622. https://doi.org/10.1007/s12257-022-0315-2
LaPorte SL, Juo ZS, Vaclavikova J et al (2008) Molecular and structural basis of cytokine receptor pleiotropy in the interleukin-4/13 system. Cell 132:259–272. https://doi.org/10.1016/j.cell.2007.12.030
Tavakkol Afshari J, Farid Hosseini R, Hosseini Farahabadi S et al (2007) Association of the expression of IL-4 and IL-13 genes, IL-4 and IgE serum levels with allergic asthma. Iran J Allergy Asthma Immunol 6:67–72
Munitz A, Brandt EB, Mingler M et al (2008) Distinct roles for IL-13 and IL-4 via IL-13 receptor alpha1 and the type II IL-4 receptor in asthma pathogenesis. Proc Natl Acad Sci USA 105:7240–7245. https://doi.org/10.1073/pnas.0802465105
Ramalingam TR, Pesce JT, Sheikh F et al (2008) Unique functions of the type II interleukin 4 receptor revealed in mice lacking the interleukin 13 receptor α1 chain. FASEB J 22(674):9. https://doi.org/10.1096/fasebj.22.1_supplement.674.9
Maes T, Joos GF, Brusselle GG (2012) Targeting interleukin-4 in asthma: Lost in translation? Am J Respir Cell Mol Biol 47:261–270. https://doi.org/10.1165/rcmb.2012-0080TR
Lee JY, Park W (2015) Anti-inflammatory effect of chrysin on RAW 264.7 mouse macrophages induced with polyinosinic-polycytidylic acid. Biotechnol Bioprocess Eng 20:1026–1034. https://doi.org/10.1007/s12257-015-0416-2
Hölscher C, Heitmann L, Owusu-Dabo E et al (2016) A mutation in IL4RA is associated with the degree of pathology in human TB patients. Mediators Inflamm 2016:4245028. https://doi.org/10.1155/2016/4245028
Karras JG, Crosby JR, Guha M et al (2007) Anti-inflammatory activity of inhaled IL-4 receptor-alpha antisense oligonucleotide in mice. Am J Respir Cell Mol Biol 36:276–285. https://doi.org/10.1165/rcmb.2005-0456OC
Ip S, Ms S, Av K et al (2022) The mixture of siRNAs targeted to IL-4 and IL-13 genes effectively reduces the airway hyperreactivity and allergic inflammation in a mouse model of asthma. Int Immunopharmacol 103:108432. https://doi.org/10.1016/j.intimp.2021.108432
Corren J, Castro M, Ford LB et al (2019) Dupilumab improves asthma outcomes irrespective of frequency of previous asthma exacerbation history. Ann Allergy Asthma Immunol 123:222-224.e1. https://doi.org/10.1016/j.anai.2019.04.028
Corren J, Hanania NA, Busse WW et al (2023) Efficacy of dupilumab in patients with uncontrolled, moderate-to-severe asthma with fungal sensitization. Clin Exp Allergy 53:1020–1030. https://doi.org/10.1111/cea.14389
Hojyo S, Uchida M, Tanaka K et al (2020) How COVID-19 induces cytokine storm with high mortality. Inflamm Regen 40:37. https://doi.org/10.1186/s41232-020-00146-3
Parasher A (2021) COVID-19: current understanding of its pathophysiology, clinical presentation and treatment. Postgrad Med J 97:312–320. https://doi.org/10.1136/postgradmedj-2020-138577
Baliga UK, Dean DA (2021) Pulmonary gene delivery-realities and possibilities. Exp Biol Med (Maywood) 246:260–274. https://doi.org/10.1177/1535370220965985
Lee W, Kim SJ (2022) Current updates on COVID-19 vaccines and therapeutics: as of June 2022. Biotechnol Bioprocess Eng 27:461–467. https://doi.org/10.1007/s12257-022-0188-4
Hariharan VN, Shin M, Chang CW et al (2023) Divalent siRNAs are bioavailable in the lung and efficiently block SARS-CoV-2 infection. Proc Natl Acad Sci USA 120:e2219523120. https://doi.org/10.1073/pnas.2219523120
Coyne CB, Kelly MM, Boucher RC et al (2000) Enhanced epithelial gene transfer by modulation of tight junctions with sodium caprate. Am J Respir Cell Mol Biol 23:602–609. https://doi.org/10.1165/ajrcmb.23.5.4164
Kim C, Ryu SH, Choi H et al (2022) The inhibitory functions of sparstolonin B against ambient fine particulate matter induced lung injury. Biotechnol Bioprocess Eng 27:949–960. https://doi.org/10.1007/s12257-022-0286-3
Duncan GA, Jung J, Hanes J et al (2016) The mucus barrier to inhaled gene therapy. Mol Ther 24:2043–2053. https://doi.org/10.1038/mt.2016.182
Alipour M, Suntres ZE, Halwani M et al (2009) Activity and interactions of liposomal antibiotics in presence of polyanions and sputum of patients with cystic fibrosis. PLoS ONE 4:e5724. https://doi.org/10.1371/journal.pone.0005724
Mall MA (2008) Role of cilia, mucus, and airway surface liquid in mucociliary dysfunction: lessons from mouse models. J Aerosol Med Pulm Drug Deliv 21:13–24. https://doi.org/10.1089/jamp.2007.0659
Stonebraker JR, Wagner D, Lefensty RW et al (2004) Glycocalyx restricts adenoviral vector access to apical receptors expressed on respiratory epithelium in vitro and in vivo: role for tethered mucins as barriers to lumenal infection. J Virol 78:13755–13768. https://doi.org/10.1128/JVI.78.24.13755-13768.2004
Chen X, Huang W, Wong BC et al (2012) Liposomes prolong the therapeutic effect of anti-asthmatic medication via pulmonary delivery. Int J Nanomed 7:1139–1148. https://doi.org/10.2147/IJN.S28011
Ng ZY, Wong JY, Panneerselvam J et al (2018) Assessing the potential of liposomes loaded with curcumin as a therapeutic intervention in asthma. Colloids Surf B Biointerfaces 172:51–59. https://doi.org/10.1016/j.colsurfb.2018.08.027
Di Gioia S, Conese M (2009) Polyethylenimine-mediated gene delivery to the lung and therapeutic applications. Drug Des Devel Ther 2:163–188. https://doi.org/10.2147/dddt.s2708
Writer MJ, Marshall B, Pilkington-Miksa MA et al (2004) Targeted gene delivery to human airway epithelial cells with synthetic vectors incorporating novel targeting peptides selected by phage display. J Drug Target 12:185–193. https://doi.org/10.1080/10611860410001724459
Manunta MD, McAnulty RJ, Tagalakis AD et al (2011) Nebulisation of receptor-targeted nanocomplexes for gene delivery to the airway epithelium. PLoS ONE 6:e26768. https://doi.org/10.1371/journal.pone.0026768
Hibbitts A, Lieggi N, McCabe O et al (2011) Screening of siRNA nanoparticles for delivery to airway epithelial cells using high-content analysis. Ther Deliv 2:987–999. https://doi.org/10.4155/tde.11.73
Tagalakis AD, Munye MM, Ivanova R et al (2018) Effective silencing of ENaC by siRNA delivered with epithelial-targeted nanocomplexes in human cystic fibrosis cells and in mouse lung. Thorax 73:847–856. https://doi.org/10.1136/thoraxjnl-2017-210670
Lee K, Willi JA, Cho N et al (2023) Cell-free biosynthesis of peptidomimetics. Biotechnol Bioprocess Eng 28:905–921. https://doi.org/10.1007/s12257-022-0268-5
Kumar P, Wu H, McBride JL et al (2007) Transvascular delivery of small interfering RNA to the central nervous system. Nature 448:39–43. https://doi.org/10.1038/nature05901
Beloor J, Ramakrishna S, Nam K et al (2015) Effective gene delivery into human stem cells with a cell-targeting peptide-modified bioreducible polymer. Small 11:2069–2079. https://doi.org/10.1002/smll.201402933
Ullah I, Chung K, Beloor J et al (2017) Trileucine residues in a ligand-CPP-based siRNA delivery platform improve endosomal escape of siRNA. J Drug Target 25:320–329. https://doi.org/10.1080/1061186X.2016.1258566
White SR, Martin LD, Stern R et al (2010) Expression of IL-4/IL-13 receptors in differentiating human airway epithelial cells. Am J Physiol Lung Cell Mol Physiol 299:L681–L693. https://doi.org/10.1152/ajplung.00422.2009
Nials AT, Uddin S (2008) Mouse models of allergic asthma: acute and chronic allergen challenge. Dis Model Mech 1:213–220. https://doi.org/10.1242/dmm.000323
Tomkinson A, Duez C, Cieslewicz G et al (2001) A murine IL-4 receptor antagonist that inhibits IL-4- and IL-13-induced responses prevents antigen-induced airway eosinophilia and airway hyperresponsiveness. J Immunol 166:5792–5800. https://doi.org/10.4049/jimmunol.166.9.5792
Cohn L, Homer RJ, MacLeod H et al (1999) Th2-induced airway mucus production is dependent on IL-4Ralpha, but not on eosinophils. J Immunol 162:6178–6183
Evans CM, Kim K, Tuvim MJ et al (2009) Mucus hypersecretion in asthma: causes and effects. Curr Opin Pulm Med 15:4–11. https://doi.org/10.1097/MCP.0b013e32831da8d3
Rogers DF (2002) Airway goblet cell hyperplasia in asthma: Hypersecretory and anti-inflammatory? Clin Exp Allergy 32:1124–1127. https://doi.org/10.1046/j.1365-2745.2002.01474.x
Reddy AT, Lakshmi SP, Reddy RC (2012) Murine model of allergen induced asthma. J Vis Exp 63:e3771. https://doi.org/10.3791/3771
Cazzola M, Matera MG (2007) Safety of long-acting beta2-agonists in the treatment of asthma. Ther Adv Respir Dis 1:35–46. https://doi.org/10.1177/1753465807081747
Reddel HK, Bacharier LB, Bateman ED et al (2022) Global initiative for asthma strategy 2021: executive summary and rationale for key changes. Am J Respir Crit Care Med 205:17–35. https://doi.org/10.1164/rccm.202109-2205PP
Corren J, Busse W, Meltzer EO et al (2010) A randomized, controlled, phase 2 study of AMG 317, an IL-4Ralpha antagonist, in patients with asthma. Am J Respir Crit Care Med 181:788–796. https://doi.org/10.1164/rccm.200909-1448OC
Wenzel S, Wilbraham D, Fuller R et al (2007) Effect of an interleukin-4 variant on late phase asthmatic response to allergen challenge in asthmatic patients: results of two phase 2a studies. Lancet 370:1422–1431. https://doi.org/10.1016/S0140-6736(07)61600-6
Rabe KF, Nair P, Brusselle G et al (2018) Efficacy and safety of dupilumab in glucocorticoid-dependent severe asthma. N Engl J Med 378:2475–2485. https://doi.org/10.1056/NEJMoa1804093
Feldmann DP, Merkel OM (2015) The advantages of pulmonary delivery of therapeutic siRNA. Ther Deliv 6:407–409. https://doi.org/10.4155/tde.15.8
Aneja MK, Geiger JP, Himmel A et al (2009) Targeted gene delivery to the lung. Expert Opin Drug Deliv 6:567–583. https://doi.org/10.1517/17425240902927841
Elfinger M, Maucksch C, Rudolph C (2007) Characterization of lactoferrin as a targeting ligand for nonviral gene delivery to airway epithelial cells. Biomaterials 28:3448–3455. https://doi.org/10.1016/j.biomaterials.2007.04.011
Elfinger M, Geiger J, Hasenpusch G et al (2009) Targeting of the beta(2)-adrenoceptor increases nonviral gene delivery to pulmonary epithelial cells in vitro and lungs in vivo. J Control Release 135:234–241. https://doi.org/10.1016/j.jconrel.2009.01.012
Hattori Y, Nakamura M, Takeuchi N et al (2019) Effect of cationic lipid in cationic liposomes on siRNA delivery into the lung by intravenous injection of cationic lipoplex. J Drug Target 27:217–227. https://doi.org/10.1080/1061186X.2018.1502775
Darcan-Nicolaisen Y, Meinicke H, Fels G et al (2009) Small interfering RNA against transcription factor STAT6 inhibits allergic airway inflammation and hyperreactivity in mice. J Immunol 182:7501–7508. https://doi.org/10.4049/jimmunol.0713433
Maouche K, Polette M, Jolly T et al (2009) {alpha}7 nicotinic acetylcholine receptor regulates airway epithelium differentiation by controlling basal cell proliferation. Am J Pathol 175:1868–1882. https://doi.org/10.2353/ajpath.2009.090212
Kuperman DA, Huang X, Nguyenvu L et al (2005) IL-4 receptor signaling in Clara cells is required for allergen-induced mucus production. J Immunol 175:3746–3752. https://doi.org/10.4049/jimmunol.175.6.3746
Dokka S, Toledo D, Shi X et al (2000) Oxygen radical-mediated pulmonary toxicity induced by some cationic liposomes. Pharm Res 17:521–525. https://doi.org/10.1023/a:1007504613351
Acknowledgements
The authors extend their gratitude to Sangah Clara Lee for her valuable comments on this manuscript. This work was supported by the Korea Research Foundation (Grant number 2022R1A2C1011348).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures were performed in accordance with the guidelines and protocols approved by the Institute of Animal Care and Use Committee of Hanyang University (2013-0144A).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ullah, I., Choi, H.S., Choi, C. et al. Targeted siRNA delivery to lung epithelia reduces airway inflammation in a mouse model of allergic asthma. Biotechnol Bioproc E 29, 97–108 (2024). https://doi.org/10.1007/s12257-024-00027-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12257-024-00027-3