Summary
Two exciting phase 2 dates were presented at Asco. This results in a new phase III study for Hepatocelluar cancer that will be launched soon. With Cholangiocarcinoma there is a new substance that shows very good oberall response rates in a subgroup of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Exciting news was presented at this year’s American Society of Clinical Oncology (ASCO) annual meeting in the field of hepatocellular carcinoma and biliary tract cancers. While not immediately practice changing, results suggest major development in the near future.
This short review summarizes novel data and is divided into two parts: hepatocellular carcinoma (HCC) news followed by biliary tract cancer (BTCs) news.
Based on annual estimates, the World Health Organization predicts that more than 1.3 million people will die from liver cancer by 2040 (Cancer Tomorrow, accessed 20 February 2021). Unfortunately, HCC is usually diagnosed at an advanced stage, indicating the importance of systemic therapy.
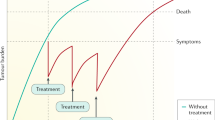
In recent years, the therapeutic armamentarium has significantly expanded as reflected in current guidelines: the combination of atezolizumab with bevacizumab (atezo + beva) is currently the first-choice first-line treatment for patients in the advanced stage (BCLC-C), as it offers a superior survival benefit compared to sorafenib [1]. Another option in the first line—especially for patients with a high risk of bleeding—is a single priming dose of tremelimumab added to durvalumab. The phase III trial HIMALAYA provided a statistically significant survival benefit vs. sorafenib [2].
In addition, therapy with TKIs such as lenvatinib and sorafenib still have a role. Lenvatinib was non-inferior to sorafenib in overall survival in untreated advanced hepatocellular carcinoma [3] and TKI therapy is relevant in patients with contraindications to immunotherapy such as liver transplantation or severe autoimmune disease.
In HCC, promising data with a novel immunotherapy approach were presented at the ASCO 2023 meeting. The MORPHEUS-liver study (NCT04524871) is a phase Ib/II, open-label, multicenter, randomized umbrella study. Data from cohort 1 were presented. The combination tiragolumab (tira) + atezo + beva were compared with the control arm (atezo + beva) in patients with unresectable, locally advanced or metastatic hepatocellular carcinoma (uHCC).
TIGIT also identified as WUCAM, VSTM3 is a co-inhibitory molecule that was first identified in 2009 [4]. Similar to LAG3 and TIM3, TIGIT belongs to the immunoglobulin superfamily [5]. TIGIT is expressed on tumor-infiltrating cytotoxic T cells, helper T cells, regulatory T cells and NK cells and its main ligand CD 155 is expressed on tumor-infiltrating myeloid cells and upregulated on cancer cells, which contributes to local suppression on immune surveillance. While single TIGIT blockade has limited anti-tumor efficacy, preclinical studies indicate that co-blockade of TIGIT and PD-1/PD-L1 pathway leads to tumor rejection, even in anti-PD-1-resistant tumor models [6]. The hypothesis is that tiragolumab (anti-TIGIT) may synergize with other immunotherapies, such in this case with a PD-L1/PD‑1 inhibitors. Since only a subset of patients show durable clinical response, we absolutely need an enlargement of our therapeutic arsenal. It seems that we are one step closer to this plan with tiragolumab in the treatment of uHCC.
In the MORPHEUS study, patients with previously untreated uHCC were randomized to receive atezo (1200 mg iv) and beva (15 mg/kg iv) with or without tira (600 mg iv) every 3 weeks.
A total of 58 patients were randomize—40 patients in the test arm and 18 in the standard treatment arm. Confirmed objective response rate (ORR), which was defined as the primary study endpoint, was 42.5% in the triplet arm compared with 11.1% in the control group. This effect was also evident in the prolonged PFS (mPFS 11.1 months, 95% confidence interval [CI] 8.2–NE) vs (4.2 month; 95% CI 1.6–7.4). Happily, no new safety signals were identified.
While the control arm had relatively poor outcomes in this study—probably explained by the small number of cases—results of the MORPHEUS-liver study still suggest a clear benefit from the combination tira + atezo + beva but results from larger studies are required and a phase III study is currently being planned (IMbrave152/SKYSCRAPER-14).
We are certainly only at the beginning of the new therapeutic landscapes, because other interesting combinations are currently being launched, for instance,
-
Phase I/II study [RELATIVITY-106] (NCT05337137)
-
Nivolumab + bevacizumab + relatlimab (anti-LAG-3)
-
-
Phase II study (NCT05359861)
-
SRF388 or placebo in combination with atezolizumab and bevacizumab
-
As opposed to HCC, biliary tract cancers (BTCs) are adenocarcinoma derived from epithelial tissue and are defined by their anatomical location in the biliary system. The three main anatomical subgroups of BTC include intrahepatic cholangiocarcinoma (iCCA), extrahepatic cholangiocarcinoma (eCCA), and gallbladder carcinoma. Although these tumors are often grouped together as cholangiocarcinoma, we learned in the past few years that there are differences in molecular characteristics and cell of origin [7].
Prognosis of all stages of BTCs is unfortunately poor due to the lack of adequate early detection, challenging anatomical access, aggressive tumor biology and modest benefit of systemic treatment. Currently, treatment of BTC in the first line is immunotherapy (durvalumab or pembrolizumab) in combination with chemotherapy [8].
Nowadays, molecular profiling with a comprehensive panel is suggested, specially, in the unresectable and or metastatic situation (ESMO guidelines). They propose the ESCAT classification (ESMO Scale of Clinical Actionability for Molecular Targets) [9]. The HER2 alterations are classified as ESCAT III (hypothetical target).
Nevertheless, HER2 (also known as ERBB2) or its gene is mutated, amplified, or overexpressed in 19.1–31.3% of gallbladder cancers, 17.4–18.5% of extrahepatic cholangiocarcinomas, and 3.7–4.8% of intrahepatic cholangiocarcinomas [10].
But it is precisely in this area that an interesting study was presented at ASCO: the HERIZON-BTC-01-trial: a multicenter, single-arm phase 2b study. In this trial, the authors used zanidatamab, a new bispecific antibody targeting two distinct HER2 epitopes: the HER2 dimerization domain and the extracellular juxtamembrane domain. This biparatopic geometric arrangement results in HER2 trans binding, which leads to the formation of receptor–antibody clusters, receptor internalization, and HER2 downregulation.
Already in preclinical studies, zanidatamab exhibited antitumor activity in HER2-driven neoplasia that was superior to both trastuzumab monotherapy and trastuzumab combined with pertuzumab [11].
The HERIZON trial tested the hypothesis that zanidatamab is an active therapy for patients with HER2-amplified biliary tract cancer.
For this reason, patients with ERBB2-amplified—confirmed by in situ hybridization per central testing in unresectable, locally advanced or metastatic biliary tract cancer with progression on a gemcitabine-based therapy were recruited at 32 clinical trial sites in nine countries in North and South America, Asia and Europe. Between 2020 and 2022, 87 patients were enrolled in the trial. The patients were assigned into cohorts based on HER2 immunohistochemistry (IHC) score: cohort 1 (IHC 2+ or 3+; HER2-positive) and cohort 2 (IHC 0 or 1+). Of the 80 patients in cohort 1, there were 45 (56%) women and 35 (44%) men; 7 patients were included in cohort 2 (2 women [29%], 5 men [71%]).
All patients received zanidatamab 20 mg/kg intravenously every 2 weeks. At the time of the data cutoff (October 10, 2022), 18 (21%) patients (17 in cohort 1 and one in cohort 2) were continuing to receive zanidatamab. Confirmed objective responses by independent central review were observed in 33 patients in cohort 1 (41.3% [95% CI 30.4–52.8]). In all, 16 (18%) patients had grade 3 treatment-related adverse events; the most common were diarrhea (4 [5%] patients) and decreased ejection fraction (3 [3%] patients).
The authors of the study concluded from the data collected that zanidatamab demonstrated meaningful clinical benefit with a manageable safety profile in patients with treatment-refractory, HER2-positive biliary tract cancer.
Further studies are to follow with the test substance (HER2-positive biliary tract cancer in combination with standard first-line cisplatin–gemcitabine [NCT03929666]).
The HERIZON-BTC-01 trial was published shortly after the ASCO [12].
In summary, both substances—tiragolumab and zanidatamab—have great potential and if the benefit is confirmed in larger trials, rapid incorporation into clinical routine can be expected.
References
Finn RS, et al. Atezolizumab plus bevacizumab in unresectable hepatocelullar carcinoma. N Eng J Med. 2020;382:1894–905. https://doi.org/10.1056/EVIDoa2100070.
Abou-Alfa GK, et al. Tremelimumab plus durvalumab in unresectable heepatocellular carcinoma. N Eng J Med. 2022;1(8).
Kudo M, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2019;391:1163–73.
Yu X, et al. The surface protein TIGIT suppresses T cell activation by promoting the generation of mature immunoregulatory dendritic cells. Nat Immunol. 2009;10:48–57. https://doi.org/10.1038/ni.1674.
Stanietsky N, et al. The interaction of TIGIT with PVR and PVRL2 inhibits human NK cell cytotoxicity. Proc Natl Acad Sci U S A. 2009;106:17858–63. https://doi.org/10.1073/pnas.0903474106.
Zhouhong Ge, et al. Front Immunol. 2012;12:699895.
Blechacz B, et al. Nat Rev Gastroenterol Hepatol. 2011;8:512–22.
Oh D‑Y, et al. NEJM Evid. 2022;.
Mosele F Ann oncol 2020; 31:1491–1505
Galdy S, et al. HER2/HER3 pathway in biliary tract malignancies; systematic review and metaanalysis: a potential therapeutic target? Cancer Metastasis Rev. 2017;36:141–57.
Lee CK, Chon HJ, Cheon J, et al. Trastuzumab plus FOLFOX for HER2positive biliary tract cancer refractory to gemcitabine and cisplatin: a multiinstitutional phase 2 trial of the Korean Cancer Study Group (KCSGHB1914). Lancet Gastroenterol Hepatol. 2023;8:56–65.
Harding JJ, et al. Lancet Oncol. 2023;24:772–82.
Razumilava N et al the Lancet 2014, Vol.383, 2168–2179
R.K. Kelley, Lancet 2023 Jun 3;401(10391):1853–1865
Hiraoka N, et al. Details of human epidermal growth factor receptor 2 status in 454 cases of biliary tract cancer. Hum Pathol. 2020;105:9–19.
Funding
Open access funding provided by University of Innsbruck and Medical University of Innsbruck.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Djanani declares that she has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Djanani, A. ASCO update—hepatocellular carcinoma and cholangiocellular carcinoma. memo 16, 234–236 (2023). https://doi.org/10.1007/s12254-023-00929-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12254-023-00929-7