Abstract
The aim of this study was to determine the influence of different CYP2C19 genotypes on selected liver function parameters, and ADR occurrence during VCZ prophylaxis in adult patients after allo-HSCT (allogeneic hematopoietic stem cell transplantation). CYP2C19 mutations were determined in a cohort of 30 adults using PCR-RFLP methods established by Sim et al. and Goldstein and Blaisdell. The patients’ protocol included biometrical and biochemical data, information on the underlying disease, chemotherapy, molds infections occurring during VCZ treatment, adverse drug reactions typical for the use of voriconazole, and probable drug - drug interactions. The observation and reporting of ADR took place from the −1 until the +20th day of VCZ therapy. For statistical analysis the χ2 test was used (p < 0.05). Among the examined patients 23 suffered from at least one side effect during VCZ therapy. Most frequent ADR were gastrointestinal disturbances (n = 15), nervous system (n = 11) and skin (n = 7) disorders. Patients with at least one loss of function allele (*2) were more likely to experience adverse drug reactions than those, with different genotypes. Due to the limited number of patients the result could not be proven with a statistical significance. Previous determination of CYP2C19 genotype may be a useful tool for prevention of adverse drug reactions during VCZ prophylaxis among patients after allo-HSCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antifungal prophylaxis is crucial for the success of each hematologic treatment. Especially for patients classified as those at highest risk of developing invasive fungal infections (IFIs). These are patients receiving intensive chemotherapy for acute myeloid leukemia and myelodysplastic syndrome, as well as corticosteroid therapy for graft-versus-host disease (GVHD) after allogeneic hematopoietic stem cell transplantation (allo-HSCT) [1].
In this group of patients, IFIs are mainly caused by Aspergillus spp. and Candida spp. The mortality rates are 56% for invasive aspergillosis and approximately 10–25% for candidiasis, what supports the necessity for appropriate antifungal prophylaxis [1,2,3].
One of the new generation triazol antifungal agents with broad-spectrum activity is voriconazole (VCZ). It is indicated for treatment of invasive aspergillosis, candidemia in non-neutropenic patients, fluconazole-resistant serious invasive Candida spp. infections and serious fungal infections caused by Scedosporium spp. and Fusarium spp. VCZ can also be an alternative for posaconazole in the prophylaxis of high risk patients in hematological units [1, 4]. The agent has saturable nonlinear pharmacokinetics, which properties are mainly influenced by food intake, inter–individual variability and drug-drug interactions. The drug is almost completely absorbed when administered under fasted conditions. The liver metabolism is primarily conducted by the hepatic cytochrome P450 CYP2C19 isoenzyme, and to a lesser extent by CYP3A4 and CYP2C9. Significant genetic polymorphisms in the CYP2C19 gene encoding for the CYP2C19 enzyme may result phenotypically in rapid or slow metabolism of voriconazole, possibly resulting in approximately 30–50% variation of plasma concentrations [5, 6]. This is why many authors postulate the need for CYP2C19 genotyping as a part of therapeutic drug monitoring of VCZ concentrations to avoid adverse drug reactions (ADRs) [7].
Voriconazole may lead to neurological (agitation, dizziness, confusion, anxiety, tremor, auditory and visual hallucinations), respiratory, thoracic and mediastinal, gastrointestinal, hepatobiliary (significant transaminitis) and skin disorders (rash, pruritus, photosensitivity). Pyrexia is another common adverse drug reaction [4]. Dose-related visual disturbances (blurred vision, photophobia, altered visual and color perception) occur in 22–45% of patients. Cardiovascular events (QT prolongation and torsade de pointes) have been reported rarely, especially with other risk factors e.g. cardiomyopathy or pro-arrhythmic medications [8]. Drug-drug interactions during hematologic treatment are also important factors leading to changes in VCZ pharmacokinetic parameters. The co-administration of e.g. cyclosporine A, phenytoin or fluconazole was reported to cause side effects due to variabilities in pharmacokinetic properties of the drug [9,10,11]. Other important drug-drug interaction during VCZ treatment are presented in Table 1.
In a previously published article, we describe 4 patients with CYP2C19*2/*17 genotype experiencing more often side effects of voriconazole then others treated with the same protocols [15]. The aim of this study was to determine the influence of different CYP2C19 genotypes on selected liver function parameters, and ADR occurrence during voriconazole treatment in a larger number of adult patients after allo-HSCT. We also performed a concomitant drug–drug interaction analysis to indicate other factors potentially causing side effects.
Materials and Methods
In the conducted study, carried out with the permission of the Bioethics Committee of Wrocław Medical University, a cohort of 30 patients, 11 women and 19 men, was examined. An observation and reporting of ADR took place from the −1 day before VCZ administration till the +20th day of treatment.
DNA Isolation and Genotyping
The material used for genetic testing was whole blood, drawn on the anticoagulant ethylenediaminetetraacetic acid (EDTA). We isolated DNA using the QIAamp® DNA Blood Mini Kit, according to the manufacturer’s instruction in a laminar flow cabinet. Two modified PCR-RFLP methods, previously adapted to the requirements of the Pharmacogenetics and Pharmacogenomics Laboratory of the Department of Clinical Pharmacology, for CYP2C19 allele 1, 2 and 17 determination by Goldstein and Blaisdell and Sim et al. were used [16, 17]. Most important information on the methods are presented in Table 2.
Patients’ Observation Protocol
Considering literature and summaries of product characteristics a patient’s protocol with most important biometrical and biochemical data was evaluated. The protocol also included information on the underlying disease, chemotherapy, molds infections occurring during VCZ treatment, adverse drug reactions typical for the use of voriconazole, and probable drug - drug interactions.
Treatment Protocol
Twenty-three patients were treated with reduced-intensity conditioning (RIC) and 7, suffering from ALL, with myeloablative conditioning (MAC). The treatment protocols were described previously by Sienkiewicz et al. [15].
Statistical Analysis
Statistical analysis was performed with the STATISTICA statistical software (STATISTICA 12, StatSoft, Tulsa, Okl.). P values less than 0.05 were considered statistically significant. To determine the influence of variables such as BMI and genotype on the occurrence and frequencies of ADR the χ2 test was used.
Results
In the examined cohort the median age was 52 years and the median BMI was 26. Ten patients were overweight (with BMI values over 25). All of the recruited patients underwent hematopoietic stem cell transplantation at the Department and Clinic of Haematology, Blood Neoplasms, and Bone Marrow Transplantation of Wrocław Medical University between 2015 and 2016 due to; acute myeloid leukemia (AML) 11 cases, acute lymphoblastic leukemia (ALL) 7 cases, myelodysplastic syndrome (MDS) 6 cases, aplastic anemia (AA) 2 cases, multiple myeloma (MM) 2 cases, myeloproliferative syndrome (MPS) 1 case, and lymphoma in 1 case.
The CYP2C19 genotypes found by performed genetic testing are presented in Fig. 1.
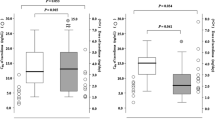
VCZ prophylaxis failed in two cases, where an invasive pulmonary aspergillosis occurred. Twenty-three patients suffered from at least one side effect during therapy. The experienced adverse drug reactions among the patients’ cohort in relation to CYP2C19 genotypes are shown in Fig. 2. Most frequent ADR were gastrointestinal disturbances (n = 15), nervous system (n = 11) and skin (n = 7) disorders.
Patients demonstrating the CYP2C19*1/*17 genotype suffered mainly from skin (rash, erythema), nervous system (headache, vertigo), and gastrointestinal disorders (nausea, gastritis). Patients with CYP2C19*1/*2 genotype experienced nervous system (headache, vertigo) and gastrointestinal disorders (constipation, nausea), CYP2C19*2/*17 patients suffered from gastrointestinal (nausea, vomiting), nervous system (headache, vertigo), skin disorders (erythema, rash), haematuria and elevated GGT values. Patients with CYP2C19*17/*17 genotype experienced vomiting and skin disorders whereas wild type genotype was connected with swelling (face and peripheral oedema). According to the presented results, patients with at least one loss of function allele (*2) experienced adverse drug reactions more often than those with different genotypes. Due to the limited number of patients the result could not be proven with a statistical significance. As for published case reports suggesting an impact of BMI on ADR we also tried to determine if there is such an influence among the examined cohort of patients [18, 19]. No relationship between BMI and frequency of side effects was found. The presented complications were temporary and had no impact on the dosage regimen nor the conducted pharmacotherapy. After convalescence, the patients were discharged from hospital.
Discussion
Thirty patients were recruited for our study. The most frequent adverse effects were gastrointestinal disturbances, skin disorders, headache, swelling, liver abnormalities (elevated GGT), pyrexia, chills, haematuria, hypertension and depression respectively. To our knowledge there are few studies on the topic of adverse drug reactions caused by voriconazole in the group of adult HSCT-patients. In a study by Brüggemann et al. visual and gastrointestinal disorders appeared most often [20]. Kim et al. and Chu et al. reported liver function abnormalities, gastrointestinal, renal, skin and visual disorders, appearing with different frequencies [21, 22].
In our cohort ten patients were overweight, no correlation with an increased number of adverse drug reactions among this group could be proven. Our findings are consistent with those from Koselke et al. who also did not observe toxicity differences in a group of 21 overweight patients, although a correlation between strongly obese patients and sub-therapeutic concentrations of voriconazole (used in standard doses) was found [23].
In the conducted study no statistical correlation between CYP2C19 genotype and the frequencies of adverse drug reactions, but a tendency of patients with loss of function allele to experience side effects more often was found. As CYP2C19 mutations are connected with lower (allele*17) or higher (allele*2) VCZ concentrations after standard dosing, an impact on the toxicity of the drug is plausible. Pascual et al. found a correlation between high VCZ concentrations and neurological disorders [24]. In a review Dolton et al. also identified a relationship between voriconazole concentrations hepatobiliary and visual disorders [25]. Our different findings can be due to a limited number of patients, similarly to the study conducted by Kim et al., where no correlation between CYP2C19 genotypes and VCZ concentrations was found [21]. Another factor having an impact on our results could be the concomitant use of cyclosporine A and methotrexate. Voriconazole is an P-gp inhibitor leading to elevated cyclosporine A concentrations, and its ADR [4]. Methotrexate use may also cause adverse drug reactions such as depression, headache, pneumonia and haematuria [26].
Conclusion
Adult patients after allo-HSCT, demonstrating minimum one loss of function allele of CYP2C19 isoenzyme, are more likely to experience adverse drug reactions during VCZ prophylaxis. Previous determination of CYP2C19 genotype may be a useful tool for prevention of adverse drug reactions during VCZ prophylaxis among hematologic patients after allo-HSCT.
There is a need for more investigation on the topic of voriconazoles’ ADR in relation to CYP2C19 genotype, which could help to identify patients potentially more likely to experience side effects.
References
Fleming S, Yannakou CK, Haeusler GM, Clark J, Grigg A, Heath CH, Bajel A et al (2014) Consensus guidelines for antifungal prophylaxis in haematological malignancy and haemopoietic stem cell transplantation, 2014. Intern Med J 44:1283–1297
Gautier-Veyret E, Fonrose X, Tonini J, Thiebaut-Bertrand A, Bartoli M, Quesada J-L, Bulabois C-E, Cahn J-Y, Stanke-Labesque F (2015) Variability of voriconazole plasma concentrations after allogeneic hematopoietic stem cell transplantation: impact of cytochrome P450 polymorphisms and comedications on initial and subsequent trough levels. Antimicrob Agents Chemother 59:2305–2314
Groll AH, Castagnola E, Cesaro S, Dalle JH, Engelhard D, Hope W, Roilides E, Styczynski J, Warris A, Lehrnbecher T (2014) Fourth European conference on infections in leukaemia (ECIL-4): guidelines for diagnosis, prevention, and treatment of invasive fungal diseases in paediatric patients with cancer or allogeneic haemopoietic stem-cell transplantation. Lancet Oncol 15:327–340
Summary of Product Characteristics Vfend (2012) http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000387/WC500049756.pdf. Accessed 10 Nov 2016
Moriyama B, Kadri S, Henning SA, Danner RL, Walsh TJ (2015) Therapeutic drug monitoring and genotypic screening in the clinical use of voriconazole. Curr Fungal Infect Rep 9:74–87
Obeng AO, Egelund EF, Alsultan A, Peloquin CA, Johnson JA (2014) CYP2C19 polymorphisms and therapeutic drug monitoring of voriconazole: are we ready for clinical implementation of pharmacogenomics? Pharmacotherapy 34:703–718
Trubiano JA, Crowe A, Worth LJ, Thursky KA, Slavin MA (2014) Putting CYP2C19 genotyping to the test: utility of pharmacogenomic evaluation in a voriconazole-treated haematology cohort. J Antimicrob Chemother 70:1161–1165
Chau MM, Kong DCM, Hal SJ, Urbancic K, Trubiano JA, Cassumbhoy M, Wilkes J, Cooper CM, Roberts JA, Marriott DJE, Worth LJ (2014) Consensus guidelines for optimizing antifungal drug delivery and monitoring to avoid toxicity and improve outcomes in patients with haematological malignancy. Intern Med J 44:1364–1388
Purkins L, Wood N, Ghahramani P, Love ER, Eve MD, Fielding A (2003) Coadministration of voriconazole and phenytoin: pharmacokinetic interaction, safety, and toleration. B J Clin Pharmacol 56:37–44
Damle B, Varma MV, Wood N (2011) Pharmacokinetics of voriconazole administered concomitantly with fluconazole and population-based simulation for sequential use. Antimicrob Agents Chemother 55:5172–5177
Summary of Product Characteristics Sandimmun (2013) http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Sandimmun_Neoral_30/WC500144886.pdf. Accessed 15 Nov 2016
Andes D, Azie N, Yang H, Harrington R, Kelley C, Tan R-D, Wu EQ, Franks B, Kristy R, Lee E, Khandelwal N, Spalding J (2016) Drug-drug interaction associated with mold-active triazoles among hospitalized patients. Antimicrob Agents Chemother 60:3398–3406
Lopez JL, Tayek JA (2016) Voriconazole-induced hepatitis via simvastatin- and lansoprazole-mediated drug interactions: a case report and review of the literature. Drug Metab Dispos 44:124–126
Vadlapatla RK, Patel M, Paturi DK, Pal D, Mitra AK (2014) Clinically relevant drug-drug interactions between antiretrovirals and antifungals. Expert Opin Drug Metab Toxicol 10(4):561–580
Sienkiewicz B, Urbaniak-Kujda D, Dybko J, Wróbel T, Wiela-Hojeńska A (2017) Influence of CYP2C19*2/*17 genotype on adverse drug reactions of voriconazole in patients after allo-HSCT - a four case report. J Cancer Res Clin Oncol 143:1103–1106
Goldstein JA, Blaisdell J (1996) Genetic tests which identify the principal defects in CYP2C19 responsible for the polymorphism in mephenytoin metabolism. Methods Enzymol 272:210–218
Sim SC, Risinger C, Dahl ML, Aklillu E, Christensen M, Bertilsson L, Ingelman-Sundberg M (2006) A common novel CYP2C19 gene variant causes ultrarapid drug metabolism relevant for the drug response to proton pump inhibitors and antidepressants. Clin Pharmacol Ther 79:103–113
Moriyama B, Falade O, Leung J, Penzak SR, Jjingo C, Huang X, Henning SA, Wilson WH, Walsh TJ (2011) Prolonged half-life of Voriconazole in CYP2C19 homozygous poor metabolizer recieving vincristine chemotherapy: avoiding a serious adverse drug interaction. Mycoses 54:1–5
Moriyama B, Jarosinski PF, Figg WD, Henning SA, Danner RA, Penzak SR, Wayne AS et al (2013) Pharmacokinetics of intravenous voriconazole in obese patients: implications of CYP2C19 homozygous poor metabolizer genotype. Pharmacotherapy 33:19–22
Brüggemann RJM, Blijlevens NMA, Burger DM, Franke B, Troke PF, Donnelly JP (2010) Pharmacokinetics and safety of 14 days intravenous voriconazole in allogeneic haematopoietic stem cell transplant recipients. J Antimicrob Chemother 65:107–113
Kim SH, Yim DS, Choi SM, Kwon JC, Han S, Lee DG, Park C, Kwon EY, Park SH, Choi JH, Yoo JH (2011) Voriconazole-related severe adverse events: clinical application of therapeutic drug monitoring in Korean patients. Int J Infect Dis 15:753–758
Chu HY, Jain R, Xie H, Pottinger P, Fredricks DN (2013) Voriconazole therapeutic drug monitoring: retrospective cohort study of the relationship to clinical outcomes and adverse events. BMC Infect Dis 13:105
Koselke E, Kraft S, Smith J, Nagel J (2012) Evaluation of the effect of obesity on voriconazole serum concentrations. J Antimicrob Chemother 67:2957–2962
Pascual A, Calandra T, Bolay S, Buclin T, Bille JMO (2008) Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin Infect Dis 46:201–211
Dolton MJ, McLachlan AJ (2014) Voriconazole pharmacokinetics and exposure-response relationships: assessing the links between exposure, efficacy and toxicity. Int J Antimicrob Agents 44:183–193
Summary of Product Characteristics Methotrexat-EBEWE (2013) http://leki.urpl.gov.pl/files/26_MethotrexatEbewe.pdf. Accessed 15 Nov 2016
Acknowledgements
This study was founded by the Ministry of Science and Higher Education, Republic of Poland (No ST-774).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sienkiewicz, B., Urbaniak-Kujda, D., Dybko, J. et al. Influence of CYP2C19 Genotypes on the Occurrence of Adverse Drug Reactions of Voriconazole among Hematological Patients after Allo-HSCT. Pathol. Oncol. Res. 24, 541–545 (2018). https://doi.org/10.1007/s12253-017-0264-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-017-0264-9