Abstract
Purpose
Assessment of the US FDA-issued WLs content is an educational tool that can be used in the continuous training program of community pharmacists in compounding pharmacies. The study was designed to critically assess FDA warning letters (WLs) issued to compounding pharmacies in 2017–2022 for violations of Current Good Manufacturing Practices (cGMP).
Methods
Content analysis was used to evaluate WLs issued concerning (1) type of violations; (2) frequency of violations mentioned in the WLs; (3) specific evaluations of the deviations related to compounded sterile products, and (4) evaluation of corrective measures requested by the US FDA.
Results
A total of 141 WLs were evaluated. The main observed violations in the analyzed WLs were adulterated drug products (130), misbranded drugs (103), unapproved new drug products (42), failure to report adverse events (22), and failure to report drugs (11). Other violations were evaluated related to sterile product compounding with emphasis on personnel qualifications, quality control procedures, equipment, etc.
Conclusion
The continuous issuance of WLs by the FDA indicates the need for compounding pharmacies become more vigilant to reduce the recurrence of the addressed violations through establishing adequate training/retraining programs. The analysis of issued WLs can serve as a learning tool to help improve compounding procedures, reduce the recurrence of these violations, and enhance patient safeguards.
Similar content being viewed by others
Introduction
Medication compounding is a process that involves combining, mixing, or altering ingredients to create distinctive medications in response to a prescription [1]. The need for compounding is crucial in the pharmaceutical profession for several reasons, including dose reduction in the pediatric patient, allergy to medication components other than the active drug, providing a liquid dosage form due to swallowing inability, etc. Compounded drugs may be made starting with active pharmaceutical ingredients (API), FDA-approved brands, or generic drugs; for example, a tablet or capsule may be converted to a liquid form for administration to a child. Benefits of compounding from approved dosage forms include basic confirmation of the identity of the active ingredient and its initial dose. Potential disadvantages include formulation complications from inactive ingredients that may not be suitable for the compounded formulation [2]. For example, an oral tablet may contain inactive ingredients that should not be administered by the intravenous route [3]. While benefits of compounding from APIs include the avoidance of binders and the possibility of accessing drug substances that are not available in suitable commercial forms for the intended use of the compounded product [1, 4, 5].
US Food and Drug Administration is the regulatory agency responsible for enforcing regulations related to public health. These regulations are in place to control the safety, efficacy, and quality of compounded products [1]. It should be emphasized that, by necessity, compounded drugs are made under standards that are less stringent than those applied to commercial products approved by the FDA; furthermore, it is difficult for compounding pharmacies to comply with the complexities of cGMP requirements under the Federal Food, Drug, and Cosmetic Act (FFDCA) and its Amendments. In 1938, the Federal Food, Drug, and Cosmetic Act (FDCA) authorized FDA oversight of pharmaceutical manufacturing. However, due to the small scale of pharmaceutical compounding compared to conventional drug manufacturers, compounding remained under the regulatory purview of individual state boards of pharmacy [6]. Cases of contaminated compounded products were reported in the twentieth century. However, the most remarkable incident was in 2012, an outbreak of fungal meningitis occurred amongst patients who had received compounded spinal epidural injections affecting 753 patients across 20 states, killing 64, later known as the Framingham outbreak. It should be emphasized that prior to and following the Framingham incident, efforts have been made at the federal level to improve oversight of compounding. There are two types of pharmacies in the US, 503A compound only in response to individual prescriptions and outsourcing facility compound in bulk and should comply with stringent CGMP standards and reporting requirements, besides paying the FDA a user fee. As a result, 503A pharmacies largely avoid the challenging regulations required of drug manufacturers under the FDCA, including adhering to cGMP [2, 7]. However, the FDA continue auditing these pharmacies in order to safeguard the patients of any harmfulness resulting from poor compounding practices. A compounded product that does not comply with the cGMP regulations can potentially risk the safety of many patients [8, 9]. Once the FDA inspects a compounding pharmacy, the FDA Form 483 is issued, addressing FDA investigators’ observations to the most responsible person at the compounding pharmacy. The FDA expects a written response to this form that addresses the corrective action plan (procedures or documentation) with supporting documentation (if any) within 15 business days from Form 483 issuance. If the response is inadequate, a warning letter (WL) is issued to address all observed violations and other details identified by the inspection team [10, 11]. A WL is a public record document that identifies the name and address of the inspected firm (e.g., pharmacy, drug manufacturer, etc.), the violation and corrective action requirements, and the timeframes for corrective actions [12]. The main target of issuing a WL to compounding pharmacies is safeguarding patients. In addition, they can help as training tools in the pharmaceutical and academic fields. These letters are available for review on the website: https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/compliance-actions-and-activities/warning-letters. In response to the WL, the inspected firm will initiate corrective actions in follow-up to the violations mentioned in the WL, which is considered the last opportunity for the compounder to “voluntarily” comply with regulations. Consequently, if these actions were considered inadequate by the FDA or the firm failed to implement these actions, regulatory actions can be taken depending on the seriousness of these violations on public health [10]. The continued issuance of WLs by the FDA over the years indicates the persistence of many errors and malpractices in several pharmacies within pharmacies. Compromise in sterile compounded drugs, in specific, have in particular, can have a disastrous effect on that may vary depending on the distributed size of the defected batchthe patients. Depending on the size of the batch, many patients can be affected [2, 13].
According to a review published by Stevens et al., there are six primary sources of continuing pharmacy education for compounding pharmacists: 1) academia, 2) educational companies, 3) healthcare networks, 4) associations (local, state, national), 5) publishers/Government, and 6) other [14]. The increased clinical role of compounding pharmacists with increased interest in individualized patient care mandates the need for quality continuing pharmacy education [15]. The education should include the most recent federal and state laws and regulations, besides updates in drug and disease state knowledge. In 2017, 18% of all continuing pharmacy education activities were provided by educational companies. This 18% includes pharmaceutical manufacturers, of which many serve as compounding support companies. Prescribers are turning more and more to compounding pharmacists to create personalized medicines for those patients who are not served by mass-produced drugs. Pharmacists should take advantage of continuing pharmacy education offerings provided by compounding support companies to remain competent with patient care regarding pharmaceutical compounding [15]. In a survey study involving students in the fourth year to explore the need for inclusion of sterile compounding as part of education and training in four years of the pharmacy curriculum of PharmD graduates, only 40.2% of students were scored in the confident or very confident range of the survey. Landry et al. suggested that sterile compounding should be part of pharmacy curricula that highlight sterility maintenance techniques, antimicrobial risk levels, contamination sources, including touch contamination, and the appropriate techniques in sterile product packaging [16].
The main objective of this article is to provide the most recent comprehensive analysis of the violations described in the WLs related only to outpatient compounding pharmacies in the USA. The analysis will address the frequency of cGMP violations, their distribution to the U.S. market, their frequency over the 5-year interval, and the type of violations. Selected examples of these violations and the FDA-recommended corrective actions will be discussed. Publishing content analysis of WLs allows teaching pharmacists and pharmacy students to focus on compliance with regulations by recognizing violations, and their corrective measures. In summary, the findings of this analysis are intended to be used as an educational tool in the continuous training program of students and community pharmacists and as a preventive measures to avoid violations in their future careers.
Methods
Source of Data and Data Extraction
The FDA WL databases can be accessed via the FDA’s Electronic Freedom of Information Reading Room. These files are made available to the public under the 1996 amendments to the Freedom of Information Act that mandates publicly accessible ‘electronic reading rooms’ with electronic search and indexing features. In this article, the following link was used: https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/compliance-actions-and-activities/warning-letters. The ‘‘Search, and Export Warning Letters to Excel’’ function was used to download an Excel Spreadsheet containing all the warning letters issued from January 1, 2017, to July 31, 2022. In the first assessment of the Excel spreadsheet, the subject of each warning letter was screened manually, and letters not associated with compounding pharmacies (e.g., food, animal products) were excluded. Then, PDF files of the remaining letters were downloaded and reviewed for qualitative and quantitative evaluation of violations. Only the content of warning letters related to compounding pharmacies was analyzed.
Data Analysis
In the first step, the sorting function in the Excel spreadsheet was used to sort the listed WLs according to the letter issuance date, letter closeout date, and issuing office. In this article, the type of violations was classified into two main categories:
Category 1: General Violations of the FDCA
-
1.
Violation related to misbranded drug
-
2.
Violation related to adulterated drug
-
3.
Violation related to unapproved new drug products
-
4.
Violation related to failure to report drugs
-
5.
Violation related to adverse events reporting
Category 2: Specific Violations
-
1.
Violations related to ineligible drug products
-
2.
Violations related to environmental monitoring
-
3.
Violations related to complaint handling
-
4.
Violations related to the recall process
The content of each WL was tabulated according to the above categories, verified, and checked versus the original and any discrepancies were resolved. Excel was used to compute descriptive statistics in addition to creating graphs.
Results
Description of the Nature of WLs
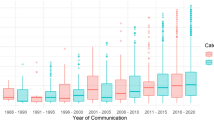
A total of 141 WLs issued to the compounding pharmacies between 2017 and 2022 were reviewed in this article. The highest number of issued WLs was reported in 2017 (55(39.00%)) compared to 6 (4.26%) in 2022 and 15 (10.64%) in 2019 and 2021, as depicted in Fig. 1A. The Office of Pharmaceutical Quality Operations issued the highest number of WLs, Division II (28 (19.86%) followed by Dallas District Office (20 (14.18%)) and the least number was issued by New England, Seattle, New Orleans, Center for Tobacco, New York Offices (one WL each) as seen in Table 1. Four inspected compounding firms received a WL more than once. The closeout interval for an issued WL ranged between 4 months and 4.62 years, with an average of 1.96 years.
As shown in Fig. 1B, drug product adulteration was the main reported violation (130 WLs (92.20%)), followed by misbranded drug products ((103 WLs (73.05%)). Violations of unapproved drug products were addressed in 42 WLs (29.79%), while failure to correctly report adverse events was reported in 22 WLs (15.60%). The failure to report drugs was mentioned only in 11 WLs (7.80%). The following paragraphs will quantitatively assess these violations, and specific examples will be explained; in addition, tables, and figures will be used to list subcategories of these violations when needed.
Drug Product Adulteration
Factors contributing to drug product adulteration are listed in Tables 2, 3, and 4. Inadequacy of the aseptic process/system (110 WLs (78.01%)) was the most reported factor, followed by personnel qualifications involved in the compounding process (103 WLs (73.04%)). Inadequate environmental monitoring-related violations (58 WLs (41.10%) and inadequate procedures to prevent microbiological contamination of drug products were reported in 51 WLs (36.17%). The table also shows other important violations that contribute to drug product adulteration, including failures due to adequately validate the aseptic process (54 WLs), failure to perform stability testing (34 WLs), pyrogen/dehydrogenation-related issues (25 WLs), air quality issues (34 WLs), and procedures related to batch release mainly active /inactive ingredient (35 WLs).
Factors contributing to drug product adulteration
Inadequacy of the aseptic process/system
The inadequate sterilization process has many components that can result in adulterated products, as seen in Fig. 2. As can be seen, the unsanitary conditions were the most contributing factor to drug product adulteration (128 WLs (90.78%), followed by failure to adopt aseptic technique (111 WLs (78.72%)) and ISO area (108 WLs (76.60%) Other violations were related to inadequate disinfection procedures, inadequate smoke (air flow) studies, and poor air quality (76, 50, 47 WLs respectively). Specifically, violations related to smoke studies conduction where failure to perform adequate smoke studies under dynamic conditions to demonstrate unidirectional airflow within the ISO 5 area was reported in 46 WLs (32.62%), and no simulation video or inadequate simulation video was reported in 17 WLs (12.06%).
Violations related to personnel qualification contributing to drug product adulteration
Table 3 details the violations related to personnel qualification. For example, inadequate personnel training/retraining and deficiencies in training records and documentation were reported in 11 and 13 WLs, respectively. Among the interesting finding were violations related to inadequate gowning (35 WLs) in the sterile area production, where the use of reused or contaminated gowns was the most observed violation (18 WLs), followed by exposure to skin and using bare hands during operation (8 WLs).
Violations related to equipments contributing to drug product adulteration
Factors that result in drug product adulteration due to equipment conditions used in compounding are listed in Table 4. The most frequently observed violation that contributes to drug product adulteration were equipment cleaning and disinfecting (85 WLs (60.28%) followed by inadequate maintenance in 24 WLs (17.02%), insufficient calibration, and routine checks (7 WLs (4.96%)).
Figure 3 depicts additional violations related to adulterated drug products that were observed during the WLs analysis.
Misbranded Drug Products
The second category of violations is related to misbranded drugs, which were mentioned in 103 WL (73.05%), whereas the failure in adequate labeling of the compounded drugs (for example, incorrect amounts declared on the label) was reported in 126 WLs (89.36%). The failure to receive valid prescriptions for individually-identified patients was reported in 92 WLs (65.25%) for a portion of the drug products produced that were considered misbranded drug products.
Unapproved New Drugs
A new drug may not be introduced or delivered for introduction into interstate commerce unless an application is approved by FDA under Sect. 505 of the FDCA. Violations related to unapproved new drugs were mentioned in 42 WLs (29.79%). The FDA considers compounded drugs as ineligible drugs due to failure to meet the conditions of Sect. 503A and is not eligible for the exemptions in that section from the FDA approval requirement of Sect. 505 of the FDCA. The manufacture of ineligible drug products is subject to FDA’s cGMP regulations, Title 21, Code of Federal Regulations (CFR), parts 210 and 211 (7,11). According to the analyzed WLs, ineligible drug products (reported in 31 WLs), where 23 drugs (or drug combinations) were considered ineligible according to the regulations. A detailed list of these drugs is mentioned in Fig. 4. It is clear from the list of ineligible drugs that domperidone alone (10 WLs) followed by melatonin (7 WLs) were the most frequently reported ineligible drugs.
Failure to Report Drugs
Compounding pharmacies are expected to submit a report identifying all the drug products that they compounded during the 6-month period as described in Sect. 503B(b)(2) of the FDCA, which is a prohibited act under Sect. 301(ccc)(3) of the FDCA (21 U.S.C. § 331(ccc)(3)). Eleven WLs (7.80%) were issued about failure to submit a report, 6 of which were following the initial registration of a compounding pharmacy as an outsourcing facility.
Violations Related to Adverse Events Reporting
The final category of violations was related to adverse events reporting, which were described in 22 WLs (15.6%).
Discussion
Compliance with cGMP regulations has been obligatory for both pharmaceutical companies and compounding pharmacies. However, according to FDA warning letter database, the number of issued WL to pharmaceutical companies showed a significant increase in the years 2015 to 2019, which can be attributed to an increase in the number of inspections performed on pharmaceutical companies in the USA and worldwide compared to US compounding pharmacies. In the years 2020 to 2021, a decrease in the number of issued WLs, was observed due to the COVID-19 pandemic and the repeated lockdowns [5]. It should be pointed out that this large number of issued WL can be due to the presence of a larger number of personnel, premises, processes, and equipment involved in drug product manufacturing. According to a very recently published study (August 2022), the most commonly identified violations in pharmaceutical companies were due to documentation (20–25% of WL). Major documentation issues include failure to maintain records of each batch produced, backdated records, misplaced records, and others. The failure of the quality unit in providing assurance of testing of materials, deficiencies in proper control of batch records, and lack of corrective and preventive actions (CAPA) in case of deviations with process performance and product quality (12–15% of WL). Manufacturing issues typically included discrepancies observed during batch-to-batch production and inadequate microbiologic investigation. These microbial contamination issues were reported for both non-sterile and sterile drugs indicating poor microbiology practices in the pharmaceutical industry. Less reported violations were associated with facilities, equipment misbranding, personnel, and adulteration. Equipment and facilities-related issues accounted for an average of 8%, while that of manufacturing was at 10%. Adulteration was consistently at the bottom of the list of violations. Facility issues included poor aseptic operations and poor monitoring of environmental conditions. Equipment issues highlighted were poor cleaning and maintenance practices, lack of cleaning validation, and sterilization of equipment [5]. Despite the violations in common between the two sectors, compounding pharmacies issued WL remain much less than that issued to pharmaceutical companies.
Nature of Violations
Adulterated Drug Products
The most common violation in the analyzed WLs was related to adulterated drug products described within the meaning of Sect. 501(a)(2)(B) of the FDCA. Section 501(b) of the Food, Drug, and Cosmetic Act (the Act) deems an official drug (i.e., a drug purported to be or represented as a drug, the name of which is recognized in an official compendium) to be adulterated if it fails to conform to compendial standards of quality, strength or purity. Additionally, the alteration, mutilation, destruction, obliteration, or removal of the whole or any part of the labeling of, or the doing of any other act with respect to, a food, drug, device, tobacco product, or cosmetic, if such act is done while such article is held for sale (whether or not the first sale) after shipment in interstate commerce and results in such article being adulterated or misbranded [6, 7]. The cGMP regulations consider the process of sterile drug production to consist of several elements, including personnel, aseptic technique, equipments’ checks, packaging, etc., and all of them contributed to the reported violations in the assessed WLs.The process of sterile drug production involves several elements like personnel, aseptic technique, equipment checks, and packaging, and all contributed to the reported violations in the assessed WLs. In 128 WLs (90.78%), insanitary conditions were the main observation contributing to the adulterated drug production. The preparation, packaging, or holding of a drug product under insanitary conditions is a chance to be contaminated with filth or rendered injurious to health, causing them to be adulterated within the meaning of Sect. 501(a)(2)(A) of the FDCA and the FDA guideline “Insanitary Conditions at Compounding Facilities’ [17]. One factor that was frequently reported in the analyzed WLs is the insanitary conditions resulting from defective personnel gowning and inadequate equipment cleaning, etc., described in detail in Table 2 and Fig. 2.
Many factors have been observed contributing to drug product adulteration, as seen in Fig. 4. For example, tasks accomplished by quality control (QC) unit are a vital contributor to cGMP compliance and have a vital impact on the early detection of drug product adulterations. Inadequate environmental monitoring and non-compliance with regulations controlling batch release can also add to drug adulteration. Violations in the batch release were related both to active and inactive ingredient testing, packaging, labeling, etc. were reported.
It is well established that the need for properly designed equipment, correct positioning together with periodic checks can facilitate the workflow of drug compounding and minimize contamination errors. Consequently, implementing equipment cleaning, routine calibration, and maintenance program is an obligatory cGMP requirement and part of the preventive measures within any compounding working environment. This also applies to automatic, mechanical, or electronic equipment regardless of the dedicated task of this equipment as requested by (21 CFR 211.68(a)), (21 CFR 211.42(c)(10)(vi)), etc. One contributing factor to drug adulteration was personnel gowning involved in aseptic operations, which is an important part of the staff compliance to cGMP. As described in Table 3, personnel qualification and mainly gowning in the sterile area production were frequently addressed in the investigated WLs. The violations involved written procedures, gowning rooms, gown sampling, and exposing naked skin (bare hand) during operation. In addition, the main equipment-related violation was inadequate cleaning and disinfecting procedures followed by poor equipment maintenance and missing routine checks that can lead to mix-ups (detailed in Table 4).
Consequences of Compounding an Adulterated Drug Product: Recall Process
An evaluation of FDA drug recalls reports revealed that the five most common recall reasons were contamination, mislabeling, adverse reactions, defective products, and incorrect potency. Compounding firms were associated more frequently with contamination than non-compounding firms [18]. The financial implications of drug recall also are substantial. If the pharmacy or FDA detects a risk to patients or public health due to causes that would constitute adulteration, the pharmacy may conduct a voluntary recall process [19]. Of the 141 issued WLs, recalls were conducted in 52 (36.88%) WLs, and 5 of them were related to ophthalmic products (eye drops or ophthalmic injection listed in Fig. 4). In addition, the cessation of production of reported adulterated sterile products was performed by 37 WLs, while suspending production was performed by 25 firms. The recall process registry can be found at the FDA-maintained website Compounding: https://www.fda.gov/drugs/human-drug-compounding/compounding-inspections-recalls-and-other-actions (accessed June 27, 2022).
Misbranded Drugs
A drug or drug product (as defined in § 320.1) in finished package form is misbranded under section 502 (a) and (b)(1) of the act if its label does not bear conspicuously the name and place of business of the manufacturer, packer, or distributor [20]. Misbranded drug products were mentioned in 103 WLs attributed to inadequately labeled compounded drug products described in 102 WLs. In the following paragraph, two cases of false or misleading labeling following the analysis of an active ingredient by the FDA are discussed.
Case 1
Failure to correctly record the exact concentration of an ingredient drug product, Nalbuphine HCl 10 mg/mL in 0.2% Saline, which contains 0.063% citric acid anhydrous. However, the container label states it contains 0.63% citric acid anhydrous. In addition, in the same WL, the labeling of the container did not specify the storage conditions adequately (i.e., it cannot be frozen; and needs to be protected from light).
Case 2
The drug product Buprexone Banana Cream 6–0.6 mg Troche, Buprenorphine Watermelon 8 mg Troche, and Buprenorphine Black Cherry 2 mg Troche drug products contained 85.7% (80.2% for Naloxone), 92.5%, and 89.4%, respectively, of the labeled concentrations of Buprenorphine as analyzed by the FDA.
Case 3
The label showed on the products as biotin 100 mg contained less than the labeled concentration of biotin (only 48.4%), no biotin, or 4-aminopyridine instead of biotin.
According to the analyzed WLs, some ineligible drug products bore inadequate directions for their intended uses so that a layman can use these products safely; they were considered misbranded under Sect. 502(f)(1) of the FDCA.
The described failure of compounding pharmacies to receive valid prescriptions for individually-identified patients for a portion of the drug products they produced was described in 92 WLs as a misbranded product. In specific, five letters named the compounded drug product without receiving valid drug prescriptions for individually-identified patients (listed in Fig. 4).
Unapproved New Drug Products/Essentially a Copy
By definition, the term “essentially a copy of an approved drug” means [21]
(A) a drug that is identical or nearly identical to an approved drug, or a marketed drug not subject to Sect. 503(b) and not subject to approval in an application submitted under Sect. 505, unless, in the case of an approved drug, the drug appears on the drug shortage list in effect under Sect. 506E at the time of compounding, distribution, and dispensing (Sect. 503B(d)(2)(A) of the FDCA (21 U.S.C. § 353b(d)(2)(A))); or (B) a drug, a component of which is a bulk drug substance that is a component of an approved drug or a marketed drug that is not subject to Sect. 503(b) and not subject to approval in an application submitted under Sect. 505, unless there is a change that produces for an individual patient a clinical difference, as determined by the prescribing practitioner, between the compounded drug and the comparable approved drug (Sect. 503B(d)(2)(B) of the FDCA (21 U.S.C. § 353b(d)(2)(B))). These restrictions were placed since the agency states that these products pose a higher risk to patients than FDA-approved drugs because the agency does not evaluate compounded drugs for safety, effectiveness, and quality before they are used, despite some researchers saying they could be an alternative to expensive drugs. Four WLs mentioned the names of drugs as essentially a copy and they are listed in Fig. 2.
Biological Products
According to Sect. 351(i)(1) of the PHS Act (42 U.S.C. §262(i)(1), the term “biological product” is defined as a virus, therapeutic serum, toxin, antitoxin, vaccine, blood, blood component or derivative, allergenic product, protein (except any chemically synthesized polypeptide), or analogous product, or arsphenamine or derivative of arsphenamine (or any other trivalent organic arsenic compound), applicable to the prevention, treatment, or cure of a disease or condition of human beings [22]. It is well established that federal law does not provide a legal pathway for marketing biological products that have been prepared outside the scope of an approved biologics license application. Four WLs (2.84%) were issued regarding violations involving biological products. Among the compounded products that were mentioned twice in the analyzed WLs is Avastin® (bevacizumab), a biological product that is subjected to licensure under Sect. 351 of the Public Health Service (PHS) Act.
Violations Related to Adverse Event Reporting
According to the Adverse Event Reporting for Outsourcing Facilities Under Sect. 503B of the Federal Food, Drug, and Cosmetic Act, it is important that adverse event data for compounded products be sent to outsourcing facilities and investigated, and serious adverse events should be communicated to the FDA. Federal regulations contain specific adverse event reporting and labeling requirements for manufacturers, including outsourcing facilities. Outsourcing facilities should develop robust mechanisms to compile and investigate adverse event reports and submit them to the appropriate regulatory agencies, which could include the FDA and their state board of pharmacies. MedWatch is one module of adverse event reporting by consumers that, when appropriate, publishes safety alerts for FDA-regulated products such as prescription and over-the-counter drugs [23, 24]. MedWatch permits the submission of reports of adverse events or other problems with products by anyone—patients as well as health professionals—using Form 3500. Every MedWatch report is important and is recorded in an FDA database for review and comparison to similar previous reports. When added together, reports can signal potential harm and lead to an FDA action to protect the public. Annual adverse event reports for non-severe and non-life-threatening events should also be submitted. The analysis of the WLs showed frequent deficiencies in adverse events handling SOP that include but are not limited to missing definitions, reporting timelines, reporting procedures, etc. Examples of violations related to adverse events reporting that were observed in the revised WLs are shown in Fig. 5.
Violations Related to Complaint Investigation
According to cGMP Sec. 211.198: Complaint files describe written procedures describing the handling of all written and oral complaints regarding a drug product shall be established and followed. It includes the following information: the name and strength of the drug product, lot number, name of the complainant, nature of the complaint, and reply to the complainant [8, 25]. Five WLs (3.55%) were issued by the US FDA that were related to complaint handling, as depicted in Fig. 5, as a result of inadequate complaint handling procedures, investigations, or failure to resolve any complaint that resulted in the violation of cGMP regulation. It should be emphasized that failure to follow-up for all product lots that can be affected by a violation in one product was also considered part of an inadequate complaint handling system.
Examples of Corrective Actions Demanded During the US FDA Inspections
Pharmaceutical compounding has always been subjected to personal, procedural, and equipment errors. Implementing a strong preventive and corrective action system (CAPA) always will minimize the occurrence of these errors. As part of the educational aim of this article, some examples of the violations and the corrective actions requested by the FDA inspectors are depicted in Fig. 6 and 7 and discussed in the following paragraphs.
Example 1
Reporting Out of Specifications (OOS) and OOS-related standard procedures (WL no./date: 574756 - 03/20/2019)
In the first inspection of the firm, the FDA issued Form 483 due to inadequate OOS handling of unexplained discrepancies or failure of a compounded batch. Consequently, the compounding pharmacy response mentioned a CAPA involving performing a "service level agreement" with a third-party laboratory that any OOS results are reported following the FDA Guidance and developing SOPs concerning the "OOS handling process" and deviations. However, upon FDA follow-up, the firm did not provide the service agreement with the contractor lab or the OOS-related SOPs. As a result of this and other violations, the WL was issued.
Example 2
Missing batch records (WL no./date: 564139 - 09/10/2018)
The FDA performed a follow up- inspection following receiving the firm's response to Form 483. In this inspection, the investigators reported in the issued WL that the pharmacy failed to prepare batch production and control records with complete information relating to the production and control of each batch as requested by 21 CFR 211.188. The corrective action included updating the SOP "Batch Record Control, Usage and Issuance" to improve documentation practices.
Example 3
Inadequate review of document (WL no./date: 574756 - 03/20/2019)
According to this WL, Form 483 stated that batch production and control records were not adequately reviewed. The firm responded that all batch and production records" will implement a review log prior to distribution. As a corrective action, a supporting document should be supplied, including staff training records on the completeness and correctness of batch records.
Example 4
Analytical errors (WL no./date: 595556 - 06/12/2020)
In a follow-up visit to the firm, FDA collected samples of a product labeled to contain 416 mg/ml of toltrazuril and 17 mg/ml of pyrimethamine. FDA analytical results of one of the samples contained 13.5 mg/mL of toltrazuril, which is 3% of the declared concentration, and 361 mg/mL of pyrimethamine, which is 2122% of the declared concentration. In addition, another sample of the same product contained 11.2 mg/mL of toltrazuril, which is 3% of the declared concentration, and 307 mg/mL of pyrimethamine, which is 1808% of the declared concentration. The corrective action included the determination of the root cause of the sub potency and superpotency in the toltrazuril/pyrimethamine paste, which was attributed to a mix-up in the weighing of the two active pharmaceutical ingredients. In addition, standard operating procedures were revised to prevent this mix-up in the future, including assigning a second staff member to check and verify weights prior to mixing and third-party vendor testing under certain circumstances.
Example 5
Insanitary conditions (WL no./date: 548673 / 04/02/2018)
In the follow-up inspection to the response related to Form 483, the FDA investigators noted drug products intended or expected to be sterile were prepared, packed, or held under insanitary conditions, which can make them become contaminated. This includes the ISO 5 hood having an area of rust with silicone applied over it; the ISO 5 hood appeared to be a crack along its overhead paneling; the pharmacy technician's beard cover left exposed skin and hair while conducting aseptic practices. Additionally, components were not adequately sanitized before placement into the ISO 5 hood. The corrective action included providing support documentation, including reviewing the SOP related to cleaning and providing training record for the technician on media fills handling.
Example 6
Pest control (WL no./date: 544530 - 01/16/2018)
According to the WL, the firm did not provide supporting documentation regarding the corrective actions of insanitary condition that was mentioned in Form FDA 483, specifically, conducting a full cleaning of the non-sterile compounding lab. The corrective actions included providing documentation of the pest control service agreement and plan. In addition, supplying supportive documentation to confirm that personnel training occurred on SOP related to "Pest Control" and "Cleaning and Maintenance of the Non-Sterile Compounding Area" for FDA review.
Example 7
Compounding product with well-known adverse events (WL no./date: 574044 - 07/09/2019)
The FDA has received several reports of serious adverse events associated with the administration of colloidal silver with inadequate well-controlled studies to support the use of this drug for any disease or condition. Additionally, colloidal silver is not the subject of an applicable USP or NF monograph and is not a component of an FDA-approved human drug. However, during the follow-up inspection to Form 483 observations, the investigator noted the production of the bulk drug substance colloidal silver for inhalation solutions (21 CFR 310.548). The corrective action included stopping manufacturing, compounding, or selling colloidal silver solutions in addition, to destroying all colloidal silver solutions stored in the firm.
Example 8
Inadequate product labeling to help adverse events reporting (WL no./date: 613792 - 10/15/2021)
In up inspection, the FDA investigator noticed that the products HCG (LYO) 12,000 IU Injectable, testosterone Cypionate in GSO (5ml) 200mg/ml Injectable, FSH (LYO) 1,500 IU Injectable, and Menotropins (HMG)(LYO) 500 IU Injectable, did not include adequate information on the container to facilitate adverse event reporting. The labeling should include www.fda.gov/medwatch and 1–800–FDA–1088. [Section 503B(a)(10) of the FDCA [21 U.S.C. §353b(a)(10)]]. The corrective action involved updating the adverse events reporting procedures to include a requirement to promptly investigate and submit a follow-up report regarding a serious, unexpected adverse event within 15 calendar days of receipt of new information or as requested by the FDA. [Section 503B(b)(5) of the FDCA [21 U.S.C. §353b(b)(5)]; 21 CFR 310.3
Example 9
Inadequate Stability testing (WL no./date: 560524 - 07/25/2018)
In the follow-up visit of the FDA following the issued Form 483, they reported that the firm failed to establish a written testing program designed to assess the stability characteristics of drug products and to use results of such stability testing to determine appropriate storage conditions and expiration dates (21 CFR 211.166(a)). The corrective action included the recall of all lots of drug products that were within expiry due to a lack of sterility assurance.
Violations related to drug product handling and the recommended corrective action (References of these examples are provided in the Supplementary Information Table S1)
Violations related to adverse event handling and the recommended corrective action (References of these examples are provided in the Supplementary Information Table S2)
Responses from Compounding Pharmacies to Issued Warning Letters
All firms accepted the findings and assured the FDA that they would look into why the problems had arisen and that needed corrective action would be taken. Despite the follow-up of the compounding pharmacies as a response to the issued letters, only two firms have been logged to send a response letter to the FDA.
For a compounding pharmacy to minimize the number of issued WLs, it is essential to strictly comply with cGMP and FDA regulations through embracing a quality management system that continuously assesses compounding procedures, building suitability, personnel, qualification, equipment conditions, product components, etc. Since drug product adulteration and misbranded products were the most reported violations, there is a need for a standard operating procedure to handle these violations as described in the issued WLs to prevent and minimize their recurrence. In addition, the need to confidently communicate with FDA inspectors, whether verbally or through written communication, is an important skill that needs to be part of training programs in the pharmaceutical profession.In addition, training programs should also emphasize the importance of verbal communication between staff during an FDA inspection. For example, verbally communicated corrective actions during an inspection without providing adequate supporting documentation can be inscribed in WL (Supplementary Information (S3)). As seen in this analysis, the initiation of a recall process or cessation of drug production was a mandatory procedure to prevent further risk to the patient. The critical evaluation of the violations mentioned in the issued WLs enables the avoidance of many regulatory actions. For example, the negative impact of the recall process can affect a firm's reputation, the pharmacy's financial profile, and its performance in the market. Thus, the establishment of a robust preventive measure and corrective action system is mandatory to avoid them in the future. As stated in all issued WL, the failure to promptly correct these violations may result in legal action without further notice, including, without limitation, seizure and injunction. The degree of penalties to be imposed in any given case is affected by many factors, including actual or potential harm to the public or to any consumer, the presence of a prior disciplinary record, etc. [6,7,8, 13].
Conclusions
The critical nature of the compounding process with its direct impact on patient health mandates the need to evaluate the violations described in the US FDA WLs. As an educational and training tool for students and pharmacists in the continuous training programs, these WLs have been reviewed for violations of cGMP regulations to reduce patients’ exposure to the risk of drug consumption resulting from non-compliance to cGMP regulations. In conclusion, the establishment and compliance with an adequate internal procedure in a compounding pharmacy will minimize the violations and consequently the number of issued WLs, which in turn will decrease the risk to patients and save a lot of time and effort.
References
Gudeman J, Jozwiakowski M, Chollet J, et al. Potential risks of pharmacy compounding. Drugs R&D. 2013;13(1):1–8. https://doi.org/10.1007/s40268-013-0005-9.
Watson CJ, Whitledge JD, Siani AM, Burns MM. Pharmaceutical compounding: a history, regulatory overview, and systematic review of compounding errors. J Med Toxicol. 2021;17(2):197–217. https://doi.org/10.1007/s13181-020-00814-3. Epub 2020 Nov 2. PMID: 33140232; PMCID: PMC7605468.
Taylor S, Hays C, Glass B. Compounding medications in a rural setting: an interprofessional perspective. J Multidiscip Healthc. 2018;20(11):197–204. https://doi.org/10.2147/JMDH.S156161. PMID: 29719402; PMCID: PMC5916384.
Mohiuddin AK. Extemporaneous compounding: selective pharmacists with separate skill. Innov Pharm. 2019;10(4). https://doi.org/10.24926/iip.v10i4.1660. Retraction in: Innov Pharm. 2020 Feb 25;11(1): PMID: 34007590; PMCID: PMC8051898.
Rathore, A.S., Li, Y., Chhabra, H. et al. FDA Warning Letters: A Retrospective Analysis of Letters Issued to Pharmaceutical Companies from 2010–2020. J Pharm Innov (2022). https://doi.org/10.1007/s12247-022-09678-2.
https://www.fda.gov/drugs/human-drug-compounding/compounding-laws-and-policies. Accessed 10 Oct 2022.
https://www.fda.gov/regulatory-information/laws-enforced-fda/federal-food-drug-and-cosmetic-act-fdc-act. Accessed 10 Oct 2022.
Current Good Manufacturing Practice For Finished Pharmaceuticals. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=211. Accessed 8 Oct 2022.
US Food and Drug Administration. Quality system (QS) regulation/medical device good manufacturing practices. https://www.fda.gov/medical-devices/postmarket-requirements-devices/quality-system-qs-regulationmedical-device-good-manufacturing-practices. Accessed 10 Oct 2022.
PART 210 - Current good manufacturing practice in manufacturing, processing, packing, or holding of drugs; General, https://www.ecfr.gov/current/title-21/chapter-I/subchapter-C/part-210. Accessed 08 Oct 2022.
Jain, SK. and Jain, RK. Review of FDA Warning Letters to Pharmaceuticals : Cause and Effect Analysis. Research J. Pharm. and Tech 2018; 11(7): 3219–3226. https://doi.org/10.5958/0974-360X.2018.00592.9.
Food and Drug Administration. Regulatory procedures manual. Chapter 4: Advisory actions exhibit 4-1—procedures for clearing FDA warning letters and untitled letters. https://www.fda.gov/media/71878/download. (Accessed June 2022)
Stewart KA, Neumann PJ. FDA actions against misleading or unsubstantiated economic and quality-of-life promotional claims: an analysis of warning letters and notices of violation. Value Health. 2002;5:390–7.
Stevens JT. Summary of Educational Offerings Provided by Compounding Support Companies in 2019. Int J Pharm Compd. 2019 May-Jun;23(3):188–191. Erratum in: Int J Pharm Compd. 2019 Sep-Oct;23(5):438. PMID: 31085786.
van der Schors, T., Amann, S., Makridaki, D., & Kohl, S. (2021). Pharmacy preparations and compounding. European journal of hospital pharmacy: science and practice, 28(4), 190–192. https://doi.org/10.1136/ejhpharm-2020-002559.
Landry SW., Singleton B., Al-Dahir S., Nguyen A., Robinson DS.. Sterile Compounding Knowledge, Skills, and Confidence Among Graduating Doctor of Pharmacy Students. Am J Pharm Educ. 2021 Mar;85(3):8345. https://doi.org/10.5688/ajpe8345. Epub 2020 Dec 23. PMID: 34283771; PMCID: PMC8006480.
Insanitary guideline. https://www.fda.gov/media/124948/download. Accessed 10 Oct 2022.
Hall K, Stewart T, Chang J, Freeman MK. Characteristics of FDA drug recalls: A 30-month analysis. Am J Health Syst Pharm. 2016 Feb 15;73(4):235–40. https://doi.org/10.2146/ajhp150277. PMID: 26843501.
Industry Guidance For Recalls. https://www.fda.gov/safety/recalls-market-withdrawals-safety-alerts/industry-guidance-recalls. Accessed 03 June 2022.
Code of Federal Regulations, Title 21, Volume 4. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=201&showFR=1&subpartNode=21:4.0.1.1.2.1. Accessed 10 Oct 2022.
Compounded Drug Products That Are Essentially Copies of a Commercially Available Drug Product Under Section 503A of the Federal Food, Drug, and Cosmetic Act Guidance for Industry. January 2018. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/compounded-drug-products-are-essentially-copies-commercially-available-drug-product-under-section. Accessed 09 Oct 2022.
FDA. 2018a. MedWatch. https://www.fda.gov/safety/medical-product-safety-information/medwatch-forms-fda-safety-reporting. Accessed 10 Oct 2022.
MedWatch: The FDA Safety Information and Adverse Event Reporting Program. https://www.fda.gov/safety/medwatch-fda-safety-information-and-adverse-event-reporting-program. Accessed 10 Oct 2022.
Veronin MA, Schumaker RP, Dixit R. The Irony of MedWatch and the FAERS Database: an assessment of data input errors and potential consequences. J Pharm Technol. 2020;36(4):164–167. https://doi.org/10.1177/8755122520928495. Epub 2020 Jun 7. PMID: 34752566; PMCID: PMC7359666.
DOJ. 2018c. United States files false claims act complaint against compounding pharmacy, private equity firm, and two pharmacy executives alleging payment of kickbacks 2018c. https://www.justice.gov/opa/pr/united-states-files-false-claims-act-complaint-against-compounding-pharmacy-private-equity. Accessed 03 March 2020.
Acknowledgements
The author is very thankful to the research assistant, Eng. Lujaine AbuBajeh, for her assistance in data extraction and data entry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
No human subjects were involved in this study. IRB/REC review not required.
Conflicts of Interest
The author declares no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dmour, I. Content Analysis of US FDA Warning Letters Issued to Compounding Pharmacies Regarding Violations of Current Good Manufacturing Practices Between 2017 and 2022. J Pharm Innov 18, 965–979 (2023). https://doi.org/10.1007/s12247-022-09692-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12247-022-09692-4