Abstract
Non-fermentative Gram-negative bacilli are now one of the most important causes of severe infections in Polish hospitals. Acinetobacter species are serious concern because of the high prevalence of multi-drug resistance among strains. Resistance profiles for 53 Gram-negative non-fermentative blood isolates were done. MLST was carried out using 44 strains representing the most commonly isolated species: A. baumannii, P. aeruginosa, and S. maltophilia. MLST revealed that all 22 A. baumannii belonged to sequence type (ST) 2. The P. aeruginosa isolates belonged to 10 different STs. Four S. maltophilia isolates matched STs present in the database (ST4, ST15, ST116, ST142), seven isolates showing novel sequence types. Among P. aeruginosa and S. maltophilia PFGE confirmed the genetical variety of strains.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infections, including bloodstream infections (BSI), caused by non-fermentative Gram-negative bacteria are an emerging problem in hospital settings, especially when caused by multi-drug resistant (MDR) strains. The most commonly isolated bacterial species are Acinetobacter baumannii and Pseudomonas aeruginosa, with infections caused by these species significantly outnumbering those caused by other species such as Stenotrophomonas maltophilia. Gram-negative bacteria are ubiquitous in the environment, but MDR A.baumannii adapts extremely quickly to the hospital environment, and may cause outbreaks (Wybo et al. 2007; Baang et al. 2012).
According to World Health Organization data, the number of BSI caused by P. aeruginosa is increasing: from 2009 to 2010 about 3.8% of BSI were caused by P. aeruginosa, compared with about 3% from 1992 to 1997. Interestingly, 17% of pneumonia cases were caused by P. aeruginosa in 2010, which was lower than in 1997 (21%) (Sievert et al. 2013). In addition, the mortality rate for BSI caused by P. aeruginosa is quite high (about 30%), with P. aeruginosa being identified as a risk factor for mortality in BSI cases (Pena et al. 2012a, b). In China, the mortality rate is even higher, with about 40% of BSI caused by P. aeruginosa resulting in death (Kang et al. 2003).
In a national survey of hospital laboratories, A. baumannii infections accounted for only 1.3% of healthcare-associated BSI (Wisplinghoff et al. 2004). However, other studies have indicated an increase in the number of reported BSI caused by A. baumannii, such as one study in patients from military medical facilities in Iraq, Kuwait, and Afghanistan (Centers for Disease Control and Prevention 2004). S. maltophilia is naturally resistant to many antimicrobial agents, including carbapenems, what may be the cause of treatment failure in infections linked to this bacterium. Therefore, the overall mortality rate of S. maltophilia BSI is very high, and ranges from 21% to 50% (Araoka et al. 2010; Senol et al. 2002; Garazi et al. 2012). One study found that risk factors associated with S. maltophilia bacteremia included use of carbapenems and antipseudomonal cephalosporins, and the isolation of S. maltophilia within 30 days of treatment (Hotta et al. 2014).
Data from a Spanish national survey conducted in 2012 showed that about 20% of bacterial strains isolated from BSI are MDR, 20% of which are carbapenem-resistant (Pena et al. 2012a, b). Therefore, the aim of this study was to analyze the molecular epidemiology and resistance profiles of Gram-negative non-fermentative bacteria isolated from patients hospitalized as a result of BSI in southern Poland, with a particular focus on multi-locus sequence typing (MLST).
Material and methods
Study population
Consecutive, non-repetitive non-fermentative Gram-negative bacillus isolates from hospitalized patients with BSI were collected from seven hospitals in southern Poland. Patients were hospitalized in three intensive care units, four internal, and three nephrology or urology wards. Isolates were received by the Department of Microbiology at Jagiellonian University Medical College, and were collected in collaboration with two other laboratories 1st January and 31st December, 2013. Patient information, including age, sex, and place of hospitalization, was also collected.
This work was approved by the Bioethics Committee of Jagiellonian University Medical College (no. KBET/312/B/2012 and KBET/362/B/2012). All data were anonymized prior to analysis.
Bacterial isolates
Specimens were collected from patients at the onset of symptoms of infection. During the study period, microbiological examination was performed on 1721 blood samples, with a total of 53 Gram-negative non-fermentative isolates tested. Identification of microorganisms was performed using the semi-automated Phoenix system (Becton-Dickinson Diagnostic System, France) according to standard methods.
Susceptibility testing
Susceptibility testing was performed using the semi-automated Phoenix NMIC/ID-204 system (Becton-Dickinson) according to the manufacturer’s instructions. Antimicrobial susceptibility was assessed according to the current European Committee on Antimicrobial Susceptibility Testing guidelines (EUCAST clinical breakpoint tables v. 5.0; http://www.eucast.org/clinical_breakpoints/, accessed 25.09.2015) and the results were considered as resistant (R) and susceptible (S). Resistant and intermediate strains were grouped together as drug resistant. For ampicillin-sulbactam and tetracycline, antimicrobial susceptibility was assessed according to the Clinical Laboratory Standards Institute guidelines.
For P.aeruginosa 13 antimicrobials were tested (gentamicin, tobramycin, amikacin, netilmicin, imipenem, meropenem, ciprofloxacin, levofloxacin, piperacillin/tazobactam, ceftazidime, cefepime, aztreonam, colistin). For A.baumannii 15 antimicrobials were tested (gentamicin, tobramycin, amikacin, netilmicin, imipenem, meropenem, ciprofloxacin, levofloxacin, piperacillin/tazobactam, ceftazidime, cefepime, trimethoprim/sulfamethoxazole, ampicillin/sulbactam, colistin, tetracycline). For S. maltophilia only trimethoprim-sulfamethoxazole and ceftazidime were tested. (Supplementary Table S1).
Different patterns of resistance, including extensively drug resistant (XDR) and multi-drug resistant (MDR) were defined according to Magiorakos et al. (2012): (1) bacteria non-susceptible to at least one agent in three or more antimicrobial categories were considered as MDR strains; (2) bacteria non-susceptible to at least one agent in all antimicrobial categories, except two or fewer categories were considered as XDR strains.
Multi-locus sequence typing
MLST was carried out as described previously using 44 strains representing the three most commonly isolated species: A.baumannii (Diancourt et al. 2010), P.aeruginosa (Curran et al. 2004), and S.maltophilia (Kaiser et al. 2009). Sequencing was performed by Genomed SA (Warsaw, Poland), and the resulting sequences were analyzed using ChromasPro 1.4 software (Technelysium Pty Ltd., Australia). MLST data were then compared with the database (http://pubmlst.org) to identify sequence types.
Pulsed field gel-electrophoresis
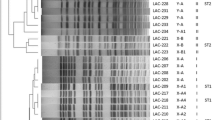
Analysis of the genetic similarity between P. aeruginosa strains or between S. maltophilia strains (separately within species) was performed using pulsed field gel electrophoresis (PFGE) in accordance with a previously published protocol (Shueh et al. 2013). Restriction enzyme digestion of P. aeruginosa strains was performed with 25 U of Spe I enzyme in Tango buffer and S. maltophilia strains were digested by Xba I enzyme in Tango buffer (Thermo-Scientific, USA). Electrophoresis was conducted in a CHEFIII PFGE unit applying the parameters: for P.aeruginosa- initial pulse 1 s, final pulse 35 s, run time 23 h, voltage 6 V/cm; for S.maltophilia- block 1: initial pulse 1 s, final pulse 15 s, run time 10 h, voltage 6 V/cm, block2: initial pulse 15 s, final pulse 60s, run time 11 h, voltage 6 V/cm. Gel Compar II 6.5 (AppliedMaths, Belgium) was used for cluster analysis using the Dice coefficient and unweighted pair group method with arithmetic mean.
Isolates with more than 90% similarity were clustered together as identical.
Repetitive PCR (rep-PCR)
Epidemiological typing of A. baumannii strains from ICUs was performed by repetitive-PCR typing using DiversiLab system (bioMerieux, France) as previously described (Chmielarczyk et al. 2016). Isolates that clustered ≥91.3% were considered related. Results of A.baumannii typing were already published.
Results
Of the 53 patients with BSI, 40 (74.1%) were men. The median age was 64 years (1st and 3rd quartile:40 and 75 years, respectively). The majority of patients were hospitalized in intensive care units (n = 30, 56.5%), followed by nephrology or urology wards (n = 14, 26.5%) and internal medicine wards (n = 9, 17.0%).
A. baumannii was the most frequently (n = 22, 41.5%), followed by P. aeruginosa (n = 11, 20.7%) and S. maltophilia (n = 11, 20.7%). Other species identified at much lower frequencies included Achromobacter denitrificans (n = 5, 9.4%), Acinetobacter lwoffii (n = 1, 1.9%), Acinetobacter ursingii (n = 1, 1.9%), Comamonas testosterone (n = 1, 1.9%), and Ochrobactrum anthropi (n = 1, 1.9%). The prevalence rates of the non-fermentative Gram-negative bacterial species in blood were: A. baumannii, 1.3%; P. aeruginosa, 0.6%; S. maltophilia, 0.6%; and others (pooled), 0.4%. In addition, multiple pathogens were isolated from the blood samples of five patients. These samples contained: A.baumannii together with coagulase-negative Staphylococcus; A.baumannii together with Enterococcus faecium; A. ursingii together with S.maltophilia; S.maltophilia together with coagulase-negative Staphylococcus; and C. testosterone together with Achromobacter denitrificans.
The vast majority of A.baumannii isolates (n = 19, 86.3%) were XDR, while the remaining isolates were MDR. Fourteen A.baumannii strains (63.6%) were resistant to all tested antibiotics except colistin. Among the P. aeruginosa isolates, only one was XDR, one was MDR, and all remaining isolates were susceptible to the tested antimicrobials. All S.maltophilia isolates were susceptible to sulfamethoxazole/trimethoprim and resistant to ceftazidime. Detailed results of resistance are in Supplementary Table S1.
MLST revealed that all 22 A.baumannii strains from the BSI samples belonged to sequence type (ST) 2. Seventeen of these isolates came from one hospital ward. The P.aeruginosa isolates belonged to 10 different STs. Only four S.maltophilia isolates matched STs present in the database (ST4, ST15, ST116, ST142), with all other isolates showing novel sequence types. Five of these isolates had an identical allele pattern, four of which were isolated from patients on a single unit (Table 1). The detailed nucleotide sequences that were obtained by MLST, are a part of the Supplementary Material.
PFGE typing of P.aeruginosa strains has shown very high heterogenity among the strains. Pulsotypes showed similarity between 50 and 65%. Two strains of P. aeruginosa with the same sequence type (ST253) were characterized by different pulsotypes (Fig. 1). It was different in case of S.maltophilia strains, where 5 strains showed similarity at the level of 90%. These strains had also the same allele pattern in the MLST method and, what is more, four of them were derived from the patients hospitalized on the same single unit (Fig. 2).
In rep-PCR sixteen strains of A.baumannii (72.7%) belonged to European clone II (EUII) assigned, three strains belonged to other clones and 3 strains have not been tested (only strains from ICU were been tested). This data was previously published (Chmielarczyk et al. 2016).
Discussion
The prevalence of BSI caused by non-fermentative Gram-negative bacilli has increased in recent years (Rattanaumpawan et al. 2013). A. baumannii and P. aeruginosa remain the predominant species, but other species are now frequently being identified (Livermore et al. 2008; Vidal et al. 2003). This may be the result of better identification techniques, or changes in the local epidemiology in the hospital wards.
The dissemination of carbapenem-resistant A. baumannii in hospitals worldwide is understood as a clonal process: the strains are transmitted through patients and it may cause outbreaks (Munoz-Price et al. 2010). The remarkably high prevalence of A.baumannii is partly the result of clonal spreading, as all isolated strains in the current study belonged to ST2. We have previously confirmed (by rep-PCR with DiversiLab system) the dominance in southern Poland of international clone 2,which is ubiquitous in Europe (Chmielarczyk et al. 2016). Epidemiological studies are important for monitoring XDR A. baumannii strains. Apart from such typing methods as MLST and rep-PCR, whole genome sequencing (WGS) is the promising technique for strain typing and outbreak investigation. WGS seems to be more discriminatory than band-based techniques however still is very expensive, and requires an additional person skilled in bioinformatics (Fitzpatrick et al. 2016).
Of serious concern is the phenotype of this our clone, with strains of this type mainly only susceptible to colistin. Unfortunately, we have no data regarding the mortality rates of patients, nor the use of central venous catheters, which is needed for more in-depth study of XDR A. baumannii. In the ICU the most frequent empirically prescribed antibiotics are carbapenems. The major limitation of using tygecycline in treatment of BSIs is the low concentration that this substance achieves in serum. Therefore, the most adequate in salvage therapy in the case of XDR A.baumannii or P.aeruginosa would be colistin in monotherapy or in combination therapy with other agents (Martis et al. 2014; Dimopoulos et al. 2015).
P. aeruginosa was isolated from BSI in the current study at a frequency only half that of A. baumannii, which is not consistent with other studies: P. aeruginosa is generally more common than A. baumannii (Picot-Guéraud et al. 2015; Sligl et al. 2015; Hotta et al. 2014). There was also a higher level of diversity among the P. aeruginosa isolates, with only two isolates showing the same ST (ST253), both of which were isolated from patients hospitalized on the same ward. Only one P. aeruginosa isolate belonged to globally disseminated XDR ST235 clone type. The PFGE method confirmed the genetic diversity among P. aeruginosa strains.
Our study also identified a relatively high number of S. maltophilia (20.7% of the total number of isolates) and A. denitrificans (9.4%) isolates. These prevalence rates were much higher than in a previous study by Rattanaumpawan et al. (5.4% and 0%, respectively), but similar to results obtained by Hotta et al. (S. maltophilia prevalence of 18.6%). Five of the S. maltophilia isolates had the same novel ST, and four of these isolates came from the same ward. What is more, they were characterized by identical pulsotypes according to PFGE method. We therefore assume that horizontal transmission was responsible for these infections. All S. maltophilia isolates were susceptible to sulfamethoxazole/trimethoprim, but some previous studies have suggested that levofloxacin should be used as an alternative treatment of BSI caused by S. maltophilia (Cho et al. 2014).
Interestingly, while other Gram-negative bacillus species were identified as the cause of BSI in the current study, none of these isolates were MDR. A. denitrificans rarely causes infectious disease in humans, and is mainly associated with immunocompromised patients.
An outbreak caused by C. testosteroni affecting hematological patients resulted from contamination of a disinfectant dispenser in a hospital in France in 2007 have been reported (Siebor et al. 2007), but no other infectious outbreaks caused by C. testosteroni have been reported. In addition, there is currently no MLST protocol for this species.
Analysis of the local epidemiology and antimicrobial susceptibility patterns of bacteria causing BSI may aid in the development of empiric therapy guidelines, infection surveillance programs, and improved patient outcomes.
Conclusions
Non-fermentative Gram-negative bacilli are now one of the most important causes of severe infections in Polish hospitals. Acinetobacter species are more commonly isolated from BSI in Poland than in other countries, which is of serious concern because of the high prevalence of multi-drug resistance among A. baumannii strains. Treatment options are severely limited for these bacteria, which are a known risk factor for increased patient mortality. The MLST technique (as well as rep-PCR) allows confirmation of horizontal transfer of Acinetobacter strains, and may aid in the identification of a common source of infection. Among P. aeruginosa, both typing methods (MLST and PFGE) showed the genetical variety of strains. While there is no one method guaranteed to reduce the number of infections caused by Gram-negative bacilli, in the case of Acinetobacter, appropriate infection control and hand hygiene may be effective.
References
Araoka H, Baba M, Yoneyama A (2010) Risk factors for mortality among patients with Stenotrophomonas maltophilia bacteremia in Tokyo, Japan, 1996–2009. Eur J Clin Microbiol Infect Dis 29:605–608
Baang JH, Axelrod P, Decker BK, Hujer AM, Dash G, Truant AR et al (2012) Longitudinal epidemiology of multidrug-resistant (MDR) Acinetobacter species in a tertiary care hospital. Am J Infect Control 40(2):134–137
Centers for Disease Control and Prevention (2004) Acinetobacter Baumannii infections among patients at military medical facilities treating injured U.S. service members, 2002–2004. MMWR Morb Mortal Wkly Rep 53:1063–1066
Chmielarczyk A, Pilarczyk-Żurek M, Kamińska W, Pobiega M, Romaniszyn D, Ziółkowski G et al (2016) Molecular epidemiology and drug resistance of Acinetobacter Baumannii isolated from hospitals in southern Poland: ICU as a risk factor for XDR strains. Microb Drug Resist 22(4):328–335
Cho SY, Kang CI, Kim J, Ha YE, Chung DR, Lee NY et al (2014) Can levofloxacin be a useful alternative to trimethoprim-sulfamethoxazole for treating Stenotrophomonas maltophilia bacteremia? Antimicrob Agents Chemother 58(1):581–583
Curran B, Jonas D, Grundmann H, Pitt T, Dowson CG (2004) Development of a multilocus sequence typing scheme for the opportunistic pathogen Pseudomonas Aeruginosa. J Clin Microbiol 42(12):5644–5649
Diancourt L, Passet V, Nemec A, Dijkshoorn L, Brisse S (2010) The population structure of Acinetobacter Baumannii: expanding multiresistant clones from an ancestral susceptible genetic pool. PLoS One 7:e10034
Dimopoulos G, Koulenti D, Tabah A, Poulakou G, Vesin A, Arvaniti K et al (2015) Bloodstream infections in ICU with increased resistance: epidemiology and outcomes. Minerva Anestesiol 81(4):405–418
Fitzpatrick MA, Ozer EA, Hauser AR (2016) Utility of whole-genome sequencing in characterizing Acinetobacter epidemiology and analyzing hospital outbreaks. J Clin Microbiol 54(3):593–612
Garazi M, Singer C, Tai J, Ginocchio CC (2012) Bloodstream infections caused by Stenotrophomonas maltophilia: a seven-year review. J Hosp Infect 81:114–118
Hotta G, Matsumura Y, Kato K, Nakano S, Yunoki T, Yamamoto M et al (2014) Risk factors and outcomes of Stenotrophomonas maltophilia bacteraemia: a comparison with bacteraemia caused by Pseudomonas Aeruginosa and Acinetobacter species. PLoS One 9(11):e112208
Kaiser S, Biehler K, Jonas D (2009) A Stenotrophomonas maltophilia multilocus sequence typing scheme for inferring population structure. J Bacteriol 191(9):2934–2943
Kang CI, Kim SH, Kim HB, Park SW, Choe YJ, Oh MD et al (2003) Pseudomonas Aeruginosa bacteremia: risk factors for mortality and influence of delayed receipt of effective antimicrobial therapy on clinical outcome. Clin Infect Dis 37:745–751
Livermore DM, Hope R, Brick G, Lillie M, Reynolds R (2008) BSAC working parties on resistance surveillance. Non-susceptibility trends among Pseudomonas Aeruginosa and other non-fermentative gram-negative bacteria from bacteraemias in the UK and Ireland, 2001-06. J Antimicrob Chemother 62(Suppl 2):ii55–ii63
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG et al (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18(3):268–281
Martis N, Leroy S, Blanc V (2014) Colistin in multi-drug resistant Pseudomonas Aeruginosa blood-stream infections: a narrative review for the clinician. J Inf Secur 69(1):1–12
Munoz-Price LS, Zembower T, Penugonda S, Schreckenberger P, Lavin MA, Welbel S et al (2010) Clinical outcomes of carbapenem-resistant Acinetobacter Baumannii bloodstream infections: study of a 2-state monoclonal outbreak. Infect Control Hosp Epidemiol 31(10):1057–1062
Pena C, Gomez-Zorrilla S, Suarez C, Dominguez MA, Tubau F, Arch O et al (2012a) Extensively drug-resistant Pseudomonas Aeruginosa: risk of bloodstream infection in hospitalized patients. Eur J Clin Microbiol Infect Dis 31:2791–2797
Pena C, Suarez C, Gozalo M, Murillas J, Almirante B, Pomar V et al (2012b) Spanish network for research in infectious diseases REIPI. Prospective multicenter study of the impact of carbapenem resistance on mortality in Pseudomonas Aeruginosa bloodstream infections. Antimicrob Agents Chemother 56:1265–1272
Picot-Guéraud R, Batailler P, Caspar Y, Hennebique A, Mallaret MR (2015) Bacteremia caused by multidrug-resistant bacteria in a French university hospital center: 3 years of collection. Am J Infect Control 43(9):960–964
Rattanaumpawan P, Ussavasodhi P, Kiratisin P, Aswapokee N (2013) Epidemiology of bacteremia caused by uncommon non-fermentative gram-negative bacteria. BMC Infect Dis 13:167
Senol E, Des Jardin J, Stark PC, Barefoot L, Snydman DR (2002) Attributable mortality of Stenotrophomonas maltophilia bacteremia. Clin Infect Dis 34:1653–1656
Shueh CS, Neela V, Hussin S, Hamat RA (2013) Simple, time saving pulsed-field gel electrophoresis protocol for the typing of Stenotrophomonas maltophilia. J Microbiol Methods 94(2):141–143
Siebor E, Llanes C, Lafon I, Ogier-Desserrey A, Duez JM, Pechinot A et al (2007) Presumed pseudobacteremia outbreak resulting from contamination of proportional disinfectant dispenser. Eur J Clin Microbiol Infect Dis 26(3):195–198
Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A et al (2013) Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010. Infect Control Hosp Epidemiol 34:1–14
Sligl WI, Dragan T, Smith SW (2015) Nosocomial gram-negative bacteremia in intensiva care: epidemiology, antimicrobial susceptibilities, and outcomes. Int J Infect Dis 7:129–134
Vidal F, Mensa J, Almela M, Olona M, Martínez JA, Marco F et al (2003) Bacteraemia in adults due to glucose non-fermentative gram-negative bacilli other than P. Aeruginosa. QJM 96(3):227–234
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39:309–317
Wybo I, Blommaert L, De Beer T, Soetens O, De Regt J, Lacor P et al (2007) Outbreak of multidrug-resistant Acinetobacter Baumannii in a Belgian university hospital after transfer of patients from Greece. J Hosp Infect 67(4):374–380
Acknowledgments
This work was supported by the National Science Centre (grant number UMO-2012/05/B/NZ7/02880). The funder played no role in study design, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Chmielarczyk, A., Pobiega, M., Romaniszyn, D. et al. Multi-locus sequence typing (MLST) of non-fermentative Gram-negative bacilli isolated from bloodstream infections in southern Poland. Folia Microbiol 63, 191–196 (2018). https://doi.org/10.1007/s12223-017-0550-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12223-017-0550-7