Abstract
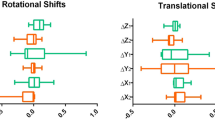
The purpose of this study was to evaluate the effect of quality assurance (QA)-related setup errors in passive proton therapy for prostate cancer with and without a hydrogel spacer. We used 20 typical computed tomography (CT) images of prostate cancer: 10 patients with and 10 patients without spacers. The following 12 model errors were assumed: output error ± 2%, range error ± 1 mm, setup error ± 1 mm for three directions, and multileaf collimator (MLC) position error ± 1 mm. We created verification plans with model errors and compared the prostate-rectal (PR) distance and dose indices with and without the spacer. The mean PR distance at the isocenter was 1.1 ± 1.3 mm without the spacer and 12.9 ± 2.9 mm with the spacer (P < 0.001). The mean rectum V53.5 GyE, V50 GyE, and V34.5 GyE in the original plan were 2.3%, 4.1%, and 12.1% without the spacer and 0.1%, 0.4%, and 3.3% with the spacer (P = 0.0011, < 0.001, and < 0.001). The effects of the range and lateral setup errors were small; however, the effects of the vertical/long setup and MLC error were significant in the cases without the spacer. The means of the maximum absolute change from original plans across all scenarios in the rectum V53.5 GyE, V50 GyE, and V34.5 GyE were 1.3%, 1.5%, and 2.3% without the spacer, and 0.2%, 0.4%, and 1.3% with the spacer (P < 0.001, < 0.001, and = 0.0019). This study indicated that spacer injections were also effective in reducing the change in the rectal dose due to setup errors.






Similar content being viewed by others
References
Nakajima K, Iwata H, Ogino H, et al. Acute toxicity of image-guided hypofractionated proton therapy for localized prostate cancer. Int J Clin Oncol. 2018;23(2):353–60. https://doi.org/10.1007/s10147-017-1209-8.
Li Z. Prescribing, recording, and reporting proton-beam therapy. Int J Radiat Oncol. 2009;73(5):1602. https://doi.org/10.1016/j.ijrobp.2008.10.084.
Iwata H, Ishikawa H, Takagi M, et al. Long-term outcomes of proton therapy for prostate cancer in Japan: a multi-institutional survey of the Japanese Radiation Oncology Study Group. Cancer Med. 2018;7(3):677–89. https://doi.org/10.1002/cam4.1350.
Hedrick SG, Fagundes M, Case S, et al. Validation of rectal sparing throughout the course of proton therapy treatment in prostate cancer patients treated with SpaceOAR®. J Appl Clin Med Phys. 2017;18(1):82–9. https://doi.org/10.1002/acm2.12010.
Morita M, Fukagai T, Hirayama K, et al. Placement of SpaceOAR hydrogel spacer for prostate cancer patients treated with iodine-125 low-dose-rate brachytherapy. Int J Urol. 2020;27(1):60–6. https://doi.org/10.1111/iju.14123.
Su Z, Slopsema R, Flampouri S, et al. Impact of intrafraction prostate motion on clinical target coverage in proton therapy: a simulation study of dosimetric differences in two delivery techniques. J Appl Clin Med Phys. 2019;20(10):67–73. https://doi.org/10.1002/acm2.12714.
Chung H, Polf J, Badiyan S, et al. Rectal dose to prostate cancer patients treated with proton therapy with or without rectal spacer. J Appl Clin Med Phys. 2017;18(1):32–9. https://doi.org/10.1002/acm2.12001.
Thörnqvist S, Muren LP, Bentzen L, et al. Degradation of target coverage due to inter-fraction motion during intensity-modulated proton therapy of prostate and elective targets. Acta Oncol (Madr). 2013;52(3):521–7. https://doi.org/10.3109/0284186X.2012.752860.
Kubota Y, Kawamura H, Sakai M, et al. Changes in rectal dose due to alterations in beam angles for setup uncertainty and range uncertainty in carbon-ion radiotherapy for prostate cancer. PLoS ONE. 2016;11(4):1–11. https://doi.org/10.1371/journal.pone.0153894.
Tang S, Deville C, McDonough J, et al. Effect of intrafraction prostate motion on proton pencil beam scanning delivery: a quantitative assessment. Int J Radiat Oncol Biol Phys. 2013;87(2):375–82. https://doi.org/10.1016/j.ijrobp.2013.05.048.
Andersen AG, Casares-Magaz O, Muren LP, et al. A method for evaluation of proton plan robustness towards inter-fractional motion applied to pelvic lymph node irradiation. Acta Oncol (Madr). 2015;54(9):1643–50. https://doi.org/10.3109/0284186X.2015.1067720.
Malyapa R, Lowe M, Bolsi A, et al. Evaluation of robustness to setup and range uncertainties for head and neck patients treated with pencil beam scanning proton therapy. Int J Radiat Oncol Biol Phys. 2016;95(1):154–62. https://doi.org/10.1016/j.ijrobp.2016.02.016.
Wohlfahrt P, Möhler C, Hietschold V, et al. Clinical implementation of dual-energy CT for proton treatment planning on pseudo-monoenergetic CT scans. Int J Radiat Oncol Biol Phys. 2017;97(2):427–34. https://doi.org/10.1016/j.ijrobp.2016.10.022.
Sejpal SV, Amos RA, Bluett JB, et al. Dosimetric changes resulting from patient rotational setup errors in proton therapy prostate plans. Int J Radiat Oncol Biol Phys. 2009;75(1):40–8. https://doi.org/10.1016/j.ijrobp.2008.08.042.
Oliver M, Bush K, Zavgorodni S, et al. Understanding the impact of RapidArc therapy delivery errors for prostate cancer. J Appl Clin Med Phys. 2011;12(3):32–43. https://doi.org/10.1120/jacmp.v12i3.3409.
Smith K, Balter P, Duhon J, et al. AAPM medical physics practice guideline 8.a.: linear accelerator performance tests. J Appl Clin Med Phys. 2017;18(4):23–39. https://doi.org/10.1002/acm2.12080.
Bonfantini F, Giandini T, Meroni S, et al. Application of failure mode and effects analysis to optimization of linac quality controls protocol. Med Phys. 2019;46(6):2541–55. https://doi.org/10.1002/mp.13538.
O’Daniel JC, Yin FF. Quantitative approach to failure mode and effect analysis for linear accelerator quality assurance. Int J Radiat Oncol Biol Phys. 2017;98(1):56–62. https://doi.org/10.1016/j.ijrobp.2017.01.035.
Rucinski A, Brons S, Richter D, et al. Ion therapy of prostate cancer: daily rectal dose reduction by application of spacer gel. Radiat Oncol. 2015;10(1):1–10. https://doi.org/10.1186/s13014-015-0348-1.
Juneja P, Kneebone A, Booth JT, et al. Prostate motion during radiotherapy of prostate cancer patients with and without application of a hydrogel spacer: a comparative study. Radiat Oncol. 2015;10(1):4–9. https://doi.org/10.1186/s13014-015-0526-1.
Toshito T, Omachi C, Kibe Y, et al. A proton therapy system in Nagoya Proton Therapy Center. Australas Phys Eng Sci Med. 2016;39(3):645–54. https://doi.org/10.1007/s13246-016-0456-8.
Yasui K, Toshito T, Omachi C, et al. A patient-specific aperture system with an energy absorber for spot scanning proton beams: verification for clinical application. Med Phys. 2015. https://doi.org/10.1118/1.4935528.
Yasui K, Toshito T, Omachi C, et al. Evaluation of dosimetric advantages of using patient-specific aperture system with intensity-modulated proton therapy for the shallow depth tumor. J Appl Clin Med Phys. 2018;19(1):132–7. https://doi.org/10.1002/acm2.12231.
Yasui K, Toshito T, Omachi C, et al. Dosimetric verification of IMPT using a commercial heterogeneous phantom. J Appl Clin Med Phys. 2019;20(2):114–20. https://doi.org/10.1002/acm2.12535.
Moyers MF, Miller DW, Bush DA, et al. Methodologies and tools for proton beam design for lung tumors. Int J Radiat Oncol Biol Phys. 2001;49(5):1429–38. https://doi.org/10.1016/S0360-3016(00)01555-8.
Arjomandy B, Sahoo N, Zhu XR, et al. An overview of the comprehensive proton therapy machine quality assurance procedures implemented at the University of Texas M. D. Anderson Cancer Center Proton Therapy Center-Houston. Med Phys. 2009;36(6):2269–82. https://doi.org/10.1118/1.3120288.
Klein EE, Hanley J, Bayouth J, et al. Task group 142 report: quality assurance of medical acceleratorsa. Med Phys. 2009;36(9):4197–212. https://doi.org/10.1118/1.3190392.
Arjomandy B, Taylor P, Ainsley C, et al. AAPM task group 224: comprehensive proton therapy machine quality assurance. Med Phys. 2019;46(8):e678-705. https://doi.org/10.1002/mp.13622.
Mok G, Benz E, Vallee JP, et al. Optimization of radiation therapy techniques for prostate cancer with prostate-rectum spacers: a systematic review. Int J Radiat Oncol Biol Phys. 2014;90(2):278–88. https://doi.org/10.1016/j.ijrobp.2014.06.044.
Polamraju P, Bagley AF, Williamson T, et al. Hydrogel spacer reduces rectal dose during proton therapy for prostate cancer: a dosimetric analysis. Int J Part Ther. 2019;5(4):23–31. https://doi.org/10.14338/ijpt-18-00041.1.
Hatiboglu G, Pinkawa M, Vallée JP, et al. Application technique: placement of a prostate—rectum spacer in men undergoing prostate radiation therapy. BJU Int. 2012;110:647–52. https://doi.org/10.1111/j.1464-410X.2012.11373.x.
Acknowledgements
The authors thank Dr. Shingo Hashimoto, Dr. Koichiro Nakajima, Dr. Yukiko Hattori, and the members of the NPTC who performed the treatment planning and accuracy management associated with this study.
Funding
This work was supported by JSPS KAKENHI Grant Number 19K17181.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have read the journal’s policy on conflicts of interest and have none to declare.
Ethical approval
This study did not involve any animal experiments. All the procedures involving human participants were conducted in accordance with the ethical standards of the institutional and/or national research committee as well as with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all the individuals included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Omi, Y., Yasui, K., Shimomura, A. et al. Dosimetric effects of quality assurance-related setup errors in passive proton therapy for prostate cancer with and without a hydrogel spacer. Radiol Phys Technol 14, 328–335 (2021). https://doi.org/10.1007/s12194-021-00632-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-021-00632-4