Abstract
Conventional mammographic dosimetry has been developed over the past 40 years. Prior to the availability of high-resolution three-dimensional breast images, certain assumptions about breast anatomy were required. These assumptions were based on the information evident on two-dimensional mammograms; they included assumptions of thick skin, a uniform mixture of glandular and adipose tissue, and a median breast density of 50%. Recently, the availability of high-resolution breast CT studies has provided more accurate data about breast anatomy, and this, in turn, has provided the opportunity to update mammographic dosimetry. Based on hundreds of data sets on breast CT volume, a number of studies were performed and reported which have shed light on the basic breast anatomy specific to dosimetry in mammography. It was shown that the average skin thickness of the breast was approximately 1.5 mm, instead of the 4 or 5 mm in the past. In another study, 3-D breast CT data sets were used for validation of the 2-D algorithm developed at the University of Toronto, leading to data suggesting that the overall average breast density is of the order of 16–20%, rather than the previously assumed 50%. Both of these assumptions led to normalized glandular dose (DgN) coefficients which are higher than those of the past. However, a comprehensive study on hundreds of breast CT data sets confirmed the findings of other investigators that there is a more centralized average location of glandular tissue within the breast. Combined with Monte Carlo studies for dosimetry, when accurate models of the distribution of glandular tissue were used, a 30% reduction in the radiation dose (as determined by the DgN coefficient) was found as an average across typical molybdenum and tungsten spectra used clinically. The 30% average reduction was found even when the thinner skin and the lower average breast density were considered. The article reviews three specific anatomic observations made possible based on high-resolution breast CT data by several different research groups. It is noted that, periodically, previous assumptions pertaining to dosimetry can be updated when new information becomes available, so that more accurate dosimetry is achieved. Dogmatic practices typically change slowly, but it is hoped that the medical physics community will continue to evaluate changes in DgN coefficients such that they become more accurate.


Adapted from a figure in Ref. [26]

Adapted from a figure in Ref. [26]

Adapted from a figure in Ref. [26]

Adapted from a figure in Ref. [32]

Adapted from a figure in Ref. [32]

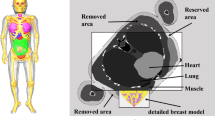
Adapted from a figure in Ref. [33]

Adapted from a figure in Ref. [33]

Adapted from a figure in Ref. [33]

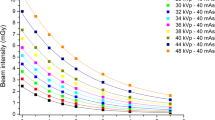
Adapted from a figure in Ref. [36]

Adapted from a figure in Ref. [36]

Adapted from a figure in Ref. [36]

Adapted from a figure in Ref. [36]

Adapted from a figure in Ref. [36]
Similar content being viewed by others
References
Pagani JJ, Bassett LW, Gold R, et al. Efficacy of combined film-screen/xeromammography: preliminary report. Am J Roentgenol. 1980;135(1):141–6.
Jensen J, Butler P. Breast exposure: nationwide trends; a mammographic quality assurance program—results to date. Radiol Technol. 1978;50(3):251.
Fitzgerald M, White DR, White E, Young J. Mammographic practice and dosimetry in Britain. Br J Radiol. 1981;54(639):212–20.
Breslow L, Thomas LB, Upton AC. Final reports of National-Cancer-Institute Ad Hoc Working Groups on Mammography in screening for breast-cancer and a summary report of their joint findings and recommendations. J Natl Cancer Inst. 1977;59(2):467–541.
Boag JW, Stacey AJ, Davis R. Radiation exposure to the patient in xeroradiography. Br J Radiol. 1976;49(579):253–61.
Dance DR, Skinner CL, Carlsson GA. Breast dosimetry. Appl Radiat Isot. 1999;50(1):185–203.
Barnes GT, Medicine SEAAoPi. Screen film mammography: imaging considerations and medical physics responsibilities. In: Proceedings of SEAAPM spring symposium, 6 Apr 1990, Columbia, South Carolina. Medical Physics Publishing; 1991.
Haus A, Yaffe M. A categorical course in physics: technical aspects of breast imaging. In: 80th Scientific assembly of the Radiological Society of North America (RSNA). Oak Brook; 1994.
Huda W, Nickoloff EL, Boone JM. Overview of patient dosimetry in diagnostic radiology in the USA for the past 50 years. Med Phys. 2008;35(12):5713–28.
Dance DR, Sechopoulos I. Dosimetry in X-ray-based breast imaging. Phys Med Biol. 2016;61(19):R271–304.
Hammerstein GR, Miller DW, White DR, Masterson ME, Woodard HQ, Laughlin JS. Absorbed radiation dose in mammography. Radiology. 1979;130(2):485–91.
Karlsson M, Nygren K, Wickman G, Hettinger G. Absorbed dose in mammary radiography. Acta Radiol Ther Phys Biol. 1976;15(3):252–8.
Sabel M, Ruff A, Weishaar J. Thermoluminescent dosimetry for radiation exposure of the breast during film and xeromammography (author’s transl). Rofo. 1978;128(5):616–22.
Schneider G, Kindl P, Spreizer H. New aspects in evaluation of average-absorbed dose of parenchyma in mammography. Fortschr Rontg Neuen. 1978;128(1):82–6.
Shrivastava PN. Radiation-dose in mammography—an energy-balance approach. Radiology. 1981;140(2):483–90.
Stanton L, Villafana T, Day JL, Lightfoot DA. Dosage evaluation in mammography. Radiology. 1984;150(2):577–84.
Lindfors KK, Boone JM, Nelson TR, Yang K, Kwan AL, Miller DF. Dedicated breast CT: initial clinical experience. Radiology. 2008;246(3):725–33.
Boone JM, Nelson TR, Lindfors KK, Seibert JA. Dedicated breast CT: radiation dose and image quality evaluation. Radiology. 2001;221(3):657–67.
Sechopoulos I, Sabol JM, Berglund J, et al. Radiation dosimetry in digital breast tomosynthesis: report of AAPM Tomosynthesis Subcommittee Task Group 223. Med Phys. 2014;41(9):091501.
Chen L, Abbey CK, Nosratieh A, Lindfors KK, Boone JM. Anatomical complexity in breast parenchyma and its implications for optimal breast imaging strategies. Med Phys. 2012;39(3):1435–41.
Boone JM. Normalized glandular dose (DgN) coefficients for arbitrary X-ray spectra in mammography: computer-fit values of Monte Carlo derived data. Med Phys. 2002;29(5):869–75.
Dance DR. Monte Carlo calculation of conversion factors for the estimation of mean glandular breast dose. Phys Med Biol. 1990;35(9):1211–9.
Wu X, Barnes GT, Tucker DM. Spectral dependence of glandular tissue dose in screen-film mammography. Radiology. 1991;179(1):143–8.
Wu X, Gingold EL, Barnes GT, Tucker DM. Normalized average glandular dose in molybdenum target-rhodium filter and rhodium target-rhodium filter mammography. Radiology. 1994;193(1):83–9.
Boone JM. Glandular breast dose for monoenergetic and high-energy X-ray beams: Monte Carlo assessment. Radiology. 1999;213(1):23–37.
Huang SY, Boone JM, Yang K, Kwan AL, Packard NJ. The effect of skin thickness determined using breast CT on mammographic dosimetry. Med Phys. 2008;35(4):1199–206.
Shi L, Vedantham S, Karellas A, O’Connell AM. Technical note: skin thickness measurements using high-resolution flat-panel cone-beam dedicated breast CT. Med Phys. 2013;40(3):031913.
Boone JM, Buonocore MH, Cooper VN. Monte Carlo validation in diagnostic radiological imaging. Med Phys. 2000;27(6):1294–304.
Packard N. Boone JM. Glandular segmentation of cone beam breast CT volume images. SPIE. 2007;6510:38–46.
Yaffe MJ. Mammographic density. Measurement of mammographic density. Breast Cancer Res. 2008;10(3):209.
Byng JW, Yaffe MJ, Jong RA, et al. Analysis of mammographic density and breast cancer risk from digitized mammograms. Radiographics. 1998;18(6):1587–98.
Yaffe MJ, Boone JM, Packard N, et al. The myth of the 50–50 breast. Med Phys. 2009;36(12):5437–43.
Huang SY, Boone JM, Yang K, et al. The characterization of breast anatomical metrics using dedicated breast CT. Med Phys. 2011;38(4):2180–91.
Vedantham S, Shi L, Karellas A, O’Connell AM. Dedicated breast CT: fibroglandular volume measurements in a diagnostic population. Med Phys. 2012;39(12):7317–28.
Hernandez AM, Boone JM. Tungsten anode spectral model using interpolating cubic splines: unfiltered X-ray spectra from 20 kV to 640 kV. Med Phys. 2014;41(4):042101.
Hernandez AM, Seibert JA, Boone JM. Breast dose in mammography is about 30% lower when realistic heterogeneous glandular distributions are considered. Med Phys. 2015;42(11):6337–48.
Dance DR, Hunt RA, Bakic PR, et al. Breast dosimetry using high-resolution voxel phantoms. Radiat Prot Dosim. 2005;114(1–3):359–63.
Sechopoulos I, Bliznakova K, Qin X, Fei B, Feng SS. Characterization of the homogeneous tissue mixture approximation in breast imaging dosimetry. Med Phys. 2012;39(8):5050–9.
Acknowledgements
This communication was funded in part by NIH Grants P30 CA093373 and R01 CA181081. The comments made are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All research described was performed with Institutional Review Board (IRB) approval, and is HIPAA compliant.
About this article
Cite this article
Boone, J.M., Hernandez, A.M. & Seibert, J.A. Two-dimensional breast dosimetry improved using three-dimensional breast image data. Radiol Phys Technol 10, 129–141 (2017). https://doi.org/10.1007/s12194-017-0404-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-017-0404-7