Abstract
When teaching infection prevention and control (IPC), nursing education tends to focus on skills and fostering good practice rather than challenging students’ thinking. Therefore, students’ misconceptions about IPC receive less attention than they deserve. The purpose of the study was to make an inventory of student nurses’ misconceptions about IPC before instruction and to make these misconceptions visible to teachers. The study was conducted in one vocational institute in Finland and is based on the answers of 29 practical nurse students before IPC training. The students took an online test requiring them to justify their answers to two multiple-true–false questions: 1) What is the main route of transmission between patients in healthcare facilities, and 2) What is the most effective and easiest manner to prevent the spreading of pathogens, e.g., multi-resistant bacteria in long-term care facilities? Analysis of the students’ written justifications resulted in three mental models: 1) the Household Hygiene Model manifesting lay knowledge learned in domestic situations, 2) the Mixed Model consisting of lay knowledge, enriched with some professional knowledge of IPC, and 3) the Transmission Model manifesting a professional understanding of IPC. The first two mental models were considered to be misconceptions. Only one of the participants showed a professional understanding (i.e., the Transmission Model). To conclude, student nurses manifested systematic patterns of misconceptions before instruction. Unless the students are confronted with their misconceptions of IPC during instruction, it is likely that these misconceptions will impede their learning or make learning outcomes transient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background and aim
Although the healthcare system is meant to prevent and treat diseases, and to care for patients, it repeatedly fails to achieve this goal. Treatments can have side-effects that need to be treated in turn, and procedures can be performed carelessly. An example of the latter is healthcare associated infections (HAI) (Cieslak et al., 2009). The World Health Organization (WHO, 2016) defines HAI as an infection that occurs in a patient during the process of care, which was either not present or incubating at the time of admission. HAI is a serious threat to public health. For instance, about 8.9 million episodes of HAI are estimated to occur in EU countries yearly; 1% of the cases are lethal (Suetens et al., 2018). Of these infections 50% could have been prevented by consistent and careful application of professional hand hygiene (WHO, 2016). Nevertheless, it was found that a majority of the healthcare workers (HCWs) do not adhere to these procedures. Improvements of the HAI situation must come from healthcare practice and education, but these are difficult to accomplish. The recent experiences during the Covid-19 pandemic made the benefits of hygiene practices very clear. The public campaigns that emphasised wearing surgical masks and washing and disinfecting hands led to a reduction in incidence of respiratory and gastrointestinal virus infections. However, despite the increased use of hand disinfectants HAIs did not decrease (Dapper et al., 2022). Dapper et al. (2022) hypothesised that increased use of hand disinfectants helped protect the staff but did not influence the protection of the patients. Infection prevention and control (IPC) and hand hygiene are mainly taught as skills in nurse training programmes (Kısacık et al., 2021; Korhonen et al., 2019). Such training programmes mostly focus on good practice, whilst challenging the pre-existing beliefs of students receives less attention; however, these beliefs warrant more consideration. In this article, we focus on these beliefs in order to discover how far they correspond with professional IPC knowledge.
Conceptual change and infection prevention and control
When student nurses start their studies, they have a basic knowledge of how to take care of their own personal and domestic hygiene as this is a general learning requirement in life (Boshuizen & Marambe, 2020; Moll et al., 1992; Vosniadou et al., 2001). A wealth of knowledge is already accumulated during early childhood by observing parents at home, e.g., from the revulsion parents show when confronted with unpleasant smelling food or bodily secretions (Curtis & Biran, 2001), and by learning from caretakers in nurseries or from teachers in schools (Boshuizen & Marambe, 2020). This familiarity with domestic hygiene situations results in a form of lay knowledge such as having a “gut feeling” for things, substances and odours which are “disgusting” (Curtis & Biran, 2001), and that washing one’s hands prevents the spreading of “bugs” and sicknesses. Some of this knowledge causes physical reactions such as feeling the urge to withdraw when touching slimy materials or knowing where to cough and how to clean one’s hands.
In the course of vocational education, student nurses need to construct professional knowledge based on official guidelines of IPC. IPC is a scientific approach and a set of practical procedures which prevent patients from being harmed by avoidable HAIs (WHO, 2016). HAIs are caused by lapses in IPC (Cieslak et al., 2009). Vocational education does seem to influence student nurses’ knowledge of IPC, but during clinical training discrepancies between theory and practice may appear (Boshuizen et al., 2020; Cox et al., 2014; Korhonen et al., 2019). There is evidence that student nurses’ knowledge and the ability to apply IPC are not sufficient (AL-Rawajfah & Tubaishat, 2015; Kelcíkova et al., 2012). The nursing curricula should prepare students to understand and apply IPC knowledge in a professional way in a range of clinical situations (Cox et al., 2014). It is possible that existing preconceptions may interfere with the construction of professional knowledge.
There is a strong line of earlier research on the misconceptions, preconceptions, alternative conceptions, naïve theories or mental models of learners which educators see as barriers to knowledge restructuring (Guzzetti et al., 1993). This lay knowledge has proven to be difficult to modify (Vosniadou & Brewer, 1992). In the context of IPC, nurses may have a preconception emphasising the importance of self-protection (Dapper et al., 2022; Jansson et al., 2016; Jeong & Kim, 2016). Unknown patients may be considered “dirty” (Curtis & Biran, 2001), and nurses need to protect themselves from the patients’ “bugs” with, e.g., gloves. In other domains, studies about the persistence of faulty mental models, e.g., of the cardiovascular system have demonstrated that not all medical students reach the necessary scientific level of understanding about the circulatory system even after instruction (Ahopelto et al., 2011; Mikkilä-Erdmann et al., 2012; Södervik et al., 2019). According to Chi (2013), a mental model is an organised collection of an individual’s beliefs. It can be an internal representation of a concept, or an interrelated system of concepts. Individuals use mental models to solve problems or answer questions (Vosniadou & Brewer, 1992).
It has been argued that students’ prior misconceptions are often hard to transform into scientific knowledge because students attempt to reconstruct professional knowledge based on their misconceptions (Boshuizen & Marambe, 2020; Merenluoto & Lehtinen, 2004). This process can result in the enrichment of existing misconceptions—instead of a transformation—because some but not all false beliefs are altered based on the instruction (Vosniadou et al., 2001). This enrichment occurs at an easier level of learning (Merenluoto & Lehtinen, 2004), whereas Conceptual Change requires a more profound revision of students’ mental models (Vosniadou et al., 2001). Before this occurs, students might have mixed, or fragmented conceptions about the topic.
When students are taught to be mindful of their existing misconceptions instead of being merely taught scientific knowledge, the result may lead to belief revision (Chi, 2013; Vosniadou et al., 2001). This revision of existing misconception may result in the abandonment of previous misconceptions and the acquisition of enriched knowledge, which according to Södervik et al. (2019) occurs gradually.
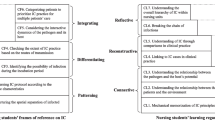
An alternative line of inquiry stresses that students do not need to abandon their lay conceptualisations (Linn, 2008; Lundholm, 2018; Solomon, 1983). Instead, naïve models based on everyday knowledge and scientific models learned in educational settings can coexist in the minds of learners. The scientific models are learnt in a meaning-making process involving a perpetual process concerning the interpretation of isolated pieces of knowledge and reflections regarding a coherent whole (Halldén, 1993; Halldén et al., 2009). Importantly, in this view on the conceptual change process, the role of education is to offer more powerful ideas and discussion of context (private context of one’s own home versus professional context) so that students can build their meta-knowledge by learning to identify differences between these two ways of thinking (Lundholm, 2022) (See Fig. 1).
In education, students are expected to see the difference between conceptions generated by everyday experiences and perceptions, and the concepts and evidence created by scientific communities. While concepts refer to classifications and the set of knowledge the person associates with the concept’s name, conceptions are systems of explanation (White, 1994) (see Fig. 1). Lay thinking and scientific thinking differ in many important ways. First, lay thinking is based on personal values, which are likely to be influenced by cultural norms and stem from personal preferences and cultural influences. For example, cultural norms about hygiene and cleanliness dictate what is edible and what is not, when one washes oneself, or what can be touched with bare hands. Instead, professional thinking needs to be built on professional values which include that absolute priority is given to the patient’s safety; IPC procedures are viewed as a means of ensuring patient safety. Second, in lay thinking, causality tends to be understood as a simple linear relation (e.g., use of gloves blocks pathogen spreading) without taking into consideration an emerging process with multiple feedback loops as in the scientific model. Third, lay thinking relies on personal experience, whereas scientific thinking relies on a review of the accumulated empirical evidence (see Fig. 1). Students also need to learn the context of applicability i.e., an awareness regarding which system of explanation and related IPC procedures to use under different circumstances (Halldén, 1999; Lundholm, 2018); students need to know that in household cleaning activities a pair of gloves can be put on without applying a hand rub in advance, while in healthcare facilities this is mandatory. Students’ values and identities are part of this process. Little by little they must learn to think like a nurse.
Finally, learning to think like a professional is likely to be moderated by motivational factors such as control beliefs and the influence of significant others (see Pintrich et al., 1993). It is important to know what kind of lay conceptions the students bring into vocational education so that teachers are able to identify lay conceptions and assist the students in making comparisons between the two ways of thinking. There are essentially two types of values: the values of the discipline and the values and emotions that the students hold (see Fig. 1).
Therefore, the purpose of the present study is to make an inventory of practical nurse students’ misconceptions about IPC. The following research questions are addressed: 1) What kind of misconceptions of IPC are held by students? 2) How prevalent are these misconceptions?
To make the misconceptions “visible”, the students were asked to answer some multiple-true–false questions and to justify their answers. Based on these written justifications, the research team created mental models to describe the typical ways students thought about IPC.
Methods
Context of the study
The study was conducted in the context of practical nurse education in Finland. Practical nurse education leads to a vocational, upper secondary degree requiring 120 ECTS. The studies take approximately three years to complete (Finnish National Agency for Education, 2018). Practical nurses are the largest group of healthcare workers in Finland (Virtanen, 2020). They typically work in basic public healthcare or private social care, including long-term care and day-care facilities. They also work in specialised public medical care, e.g., inpatient wards, hospitals, ambulances, or homecare depending on their specialisation (Finnish National Agency for Education, 2018).
During their studies practical nurse students acquire a wide range of basic competences related to nursing and care including observing the vital functions and symptoms of patients. The students also obtain a medication administration licence allowing them to dispense and administer medications via natural routes, and by subcutaneous and intramuscular injections when instructed to do so. Regarding IPC, the curriculum states that “students follow the principles of aseptic working methods” (Finnish National Agency for Education, 2018).
Participants
Participants were recruited from a vocational school in Finland immediately prior to the outbreak of the COVID-19 pandemic. The first-year adult students had just begun their studies in practical nursing, and the first author was the teacher of the 30-h compulsory course on IPC. The study was conducted during the course but providing the material for the study was voluntary.
Of a total of 90 students, 67 students (74%) (54 females, 81%, 13 males, 19%) provided their written consent to participate in the study. However, only 29 participants (24 females, 83%, 5 males, 17%) supplied complete answers (i.e., answers including written justifications) to the questions this study focused on, resulting in a sample size of 29. The participants’ age varied from 18 to 55. Eight participants were under 25 years of age, thirteen were 26–40, and eight were over 40.
Materials and procedures
As a part of their studies, the students took a test on IPC before the start of the course. This test, containing multiple-true–false questions together with prompts to justify one’s responses, was administered during the first lesson using an on-line tool (Webropol). It was possible to complete the survey at home for those students who were absent. The link to the test was sent via the school’s learning management system with the possibility to complete it via a computer or a mobile device. The time to complete the test ranged from 12 to 61 min.
The present study is based on an examination of two questions from a more extensive questionnaire developed explicitly for the purpose of this study. The validity and reliability of the entire questionnaire will be reported elsewhere.
Students were asked to indicate whether each of the four answers provided for both questions were true or false (see Appendix 1). A point was given for every correct answer (a point for each true positive or true negative) with a maximum of eight points. The first question ‘What is the main route of transmission between patients in healthcare facilities?’ was inspired by the study conducted by Jeong and Kim (2016); the second question ‘What is the most effective and easiest manner to prevent the spreading of pathogens (e.g., multiresistant bacteria) in long-term care facilities?’ was derived from the study by Caniza et al. (2007). The questions were translated into Finnish and partly modified based on current, national, and international guidelines. The present study is based on an analysis of the written justifications given for the two multiple-true–false questions.
Ethical approval
The study was granted ethical approval, (code 27/2019) by the Ethical review board of the Finnish university involved in the study. The principal of the vocational school granted the research permit. The participants were informed about the research project, and informed consent was obtained at the beginning of the first lesson. Permission via email was sought from those participants who did not attend the first lesson. Participation in the study was voluntary. Participants or non-participants were not advantaged or disadvantaged in any way.
Data coding and analysis
The data analysis was based on a method initiated by Patel and Groen (1986) who investigated clinical reasoning in medicine. This method has been described very succinctly by Van de Wiel et al. (2000). To enable comparison at a conceptual level, students’ answers were rewritten as concept maps (Tversky, 2011). These concept maps consisted of nodes and links between nodes. The nodes represent the different concepts applied in a justification, and the links between nodes represent the relationship between the concepts. To enable comparison between maps some standard abbreviations or elements were used: P for patient, HCW for healthcare worker, arrow for connecting (causal) link, X connected to arrow for breaking that link, att for attributes such as “has features of…, or instr for instrument such as “with their hands”. The reliability of the methodology and validity of the outcomes was monitored through a combination of independent coding and a discussion of any differences.
Analysis proceeded in chronological order as follows:
-
1.
The research team read through the justifications of questions 1 and 2. A subset of 19 protocols (i.e., cases) was selected and visually represented as concept maps.
-
2.
The fourth author created two extreme prototypical models and visualised them as concept maps (see Appendix 2). The Household Hygiene Model was created bottom-up, i.e., based on the students’ justifications. The term was inspired by Moll et al., (1992, p 133) who used the term ‘household funds of knowledge’ to refer to the ‘historically accumulated and culturally developed bodies of knowledge and skills essential for household […] functioning’. The Transmission Model was created using a top-down approach based on scientific knowledge of IPC (WHO, 2016).
-
3.
Then the first author attempted to categorise the cases into these two extremes. To solve discrepancies, the research team created a third model called the Mixed Model, which contained features of both of the two previous models.
-
4.
These three models were translated into categorisation criteria (see Table 1).
-
5.
Using these criteria, the first author categorised the 19 cases into one of the three mental models. The responses to the multiple-true–false questions were ignored at this phase.
-
6.
Authors 1, 2 and 3 discussed the decisions made by the first author in phase 5. This resulted in transferring some cases to another category.
-
7.
The fourth author worked independently as a second coder. This resulted in disagreement regarding four cases.
-
8.
The team concluded that referring to “hand hygiene” instead of “hand disinfection” was a sufficient inclusion criterium for the Mixed Model. This resulted in agreement regarding all cases.
-
9.
To check for coder agreement the remaining ten cases were categorised by the first and fourth author independently. This resulted in complete agreement without the necessity for further discussions.
Results: the Three Mental Models
Based on the analyses of the students’ justifications to questions 1 and 2, three mental models were formed. These were defined as 1) the Household Hygiene Model, 2) the Mixed Model, and 3) the Transmission Model (see Table 1). The three models found showed that there were two large subclasses of misconceptions: household conceptions and household conceptions enriched with scientific professional knowledge.
The background knowledge of IPC and use of terminology in the present study requires some clarification. The main route of transmission is the HCWs’ direct contact with patients by means of undisinfected hands (WHO, 2009). Other routes of transmission include airborne transmission (via dust) and droplet (respiratory) transmission.
Hand hygiene is considered a general lay expression for cleaning one’s hands because there is no definition of how it should be applied. Hand disinfection means rubbing alcohol-based liquid to disinfect the healthcare workers’ hands (Pittet & Boyce, 2003). Hand disinfection (“hand rub”) is considered a professional expression when used in this context. Hand disinfection is the easiest, cheapest, and most favourable way to prevent the spreading of pathogens from the HCWs’ hands within healthcare. Improving HCWs’ hand disinfection according to official guidelines reduces the spreading of pathogens between vulnerable patients and therefore prevents HAIs (WHO, 2009).
In contrast, washing one’s hands (hand wash) is an action whereby the hands are cleaned using soap and water when they are visibly soiled. Several authors (AL-Rawajfah & Tubaishat, 2015; Caniza et al., 2007; Jeong & Kim, 2016; Ward, 2013) consider handwashing sufficient. In this study, hand washing was not considered to be a professional manner for healthcare workers to clean their hands at work. Finnish student nurses are taught according to the guidelines provided by the local authorities and the WHO, which state that the healthcare worker’s hands should be disinfected using an alcohol-based hand rub unless visibly soiled (Sairaalahygienia- ja infektiontorjuntayksikkö, 2023; WHO, 2009).
Gloves are disposable, and non-sterile. They are used during nursing procedures where there is a risk of contact with any kind of secretion (Pittet & Boyce, 2003). Appropriate use of gloves is poorly understood among HCW (e.g., when, and how to put on and take off gloves correctly). Using gloves in situations when they are not indicated can lead to cross-contamination between patients, and a waste of resources (WHO, 2009).
Household hygiene model
Instances of the Household Hygiene Model represent the clearest misconceptions students have about IPC. In this model, the knowledge is based on lay knowledge about domestic hygiene learned from everyday situations. It is typical of this model that the HCW is not mentioned as the pathogen-spreading link between patients. Instead, the patients and their visitors, surfaces, and secretions are reported as the main route of transmission. These students speak about hand hygiene or hand washing, but they do not mention hand disinfection. They use everyday language instead of professional language, with many of them emphasising the use of gloves in patient contacts.
The mental model of Student 12 (see Fig. 2) is presented, because it is closest to the prototypical model of the Household Hygiene Model (see Appendix 2). The original justifications for Question 1 and 2 are presented on the left side of the figure, and on the right side the justifications are visualised in the form of a concept map. Student 12 scored six out of eight points on the multiple-true–false test by answering most questions correctly but failing to indicate that the main transmission route is the healthcare worker’s hands.
The student was of the opinion that surfaces are the main route of transmission. When the student’s justifications were analysed, it seemed that the student had no idea of IPC in healthcare and believed that “poor cleaning” and “poor air quality” are the main routes of transmission, instead of the HCW’s hands. Perhaps by poor air quality, the student was referring to airborne transmission. By stating that “all relatives and healthcare workers prevent the spreading of pathogens by washing their hands”, the student was referring to basic household knowledge. This is clearly incorrect: both relatives and HCWs are instructed to prevent the spreading of pathogens by disinfecting their hands by using hand rub in healthcare settings.
Student 64’s mental model was also classified as an instance of the Household Hygiene Model. The student scored two out of eight points on the multiple-true–false questions, answering only two items correctly, namely 1) antibiotics are not the most effective manner to prevent infections, and 2) hand disinfection is the most effective manner to prevent the spreading of infections. The student specified that surfaces touched by patients who do not attend to hygiene sufficiently spread bacteria (see Fig. 3) which is correct, but it is not the main route of transmission; it is the HCWs’ hands that are the main route of transmission. The student also stated that “Infections can be prevented with vaccinations” which is also correct, but again not the correct answer to the question regarding the main route of transmission (WHO, 2009). It remains unclear what exactly the student meant by stating that “the right kind of protection can prevent the spreading of diseases”. Perhaps the student meant using personal protective equipment, meaning gloves, gowns, and masks. As in the case of Student 12, it is assumed that Student 64 had not internalised how critical the healthcare worker’s role is in IPC, because in the written accounts other people were held responsible for the spreading of pathogens.
The final example of the Household Hygiene Model (Student 63) is interesting, because the student (see Fig. 4) appears to have some working experience with the elderly. In the response, the student emphasises the use of gloves in IPC, instead of hand disinfection, which is typical of the household hygiene model. This student seems to focus on self-protection and resorts to intuitive-emotional decision-making (Aarkrog & Wahlgren, 2022) rather than protecting the patients. Similar to Student 64, Student 63 had the same two answers correct, with antibiotics not being the most effective manner to prevent infections and hand disinfection being the easiest way to prevent infections from spreading.
Student 63 justifies how surfaces and patients are the main route of transmission: “All patients may not necessarily control themselves and spreading their own secretions, while moving they touch the mouth (saliva) and then the surfaces of the corridor etc.” The student may be referring to droplet transmission. There is some idea of what patients and healthcare workers do, as evidenced by the comment “staff mainly wash their hands regularly and use gloves”. Claiming that “preventing vaccinations with protective gloves” is a clear misunderstanding of the purpose of gloves (Pittet & Boyce, 2003). Gloves should be used only when there is risk of contaminating the HCW’s hands with secretions. It also seems that the student has no awareness of the purpose of disinfecting a nurse’s hands.
Ten of the 29 (34%) mental models provided by the students were classified as instances of the Household Hygiene Model. Seven of these students scored 5–6 points out of a possible 8 from the multiple-true–false questions, and three students scored between 2 to 4 points.
The mixed model
In the Mixed Model, the students expressed some understanding of the critical role of the nurse in IPC. They expressed that the nurse is the main pathogen spreading link between the patients which is correct, but patients and visitors, surfaces and secretions were also reported as the main route of transmission as in the Household Hygiene Model. Hand disinfection or a hand rub, central in IPC, is also presented in this mental model. Everyday language such as “bugs” instead of professional phrases such as pathogens, bacteria or virus are typically used.
The mental model of Student 51 is the most characteristic instance of the Mixed Model (see Fig. 5). The student scored only two points out of eight on the multiple-true–false questions, stating that all the alternatives represent the main route of transmission, and all the alternatives are the most effective and easiest manners to prevent spreading of pathogens.
The student indicated professional knowledge and awareness of the critical role of the nurse in IPC stating that “Staff should clean their hands before and after touching the patient. Protective gloves should be changed (between procedures/ when the patient changes).” It is not clear what Student 51 meant by stating “If the secretions are not handled properly, the contact surfaces are contaminated”. In any case, this statement is interpreted as household hygiene knowledge because it is not the main route of transmission. Whilst the knowledge of vaccinations and antibiotics is correct in the sense that they can prevent infections, it is not the correct answer to the question regarding the most effective way to prevent infections. Stating that “Hand rub and the use of gloves always” emphasises the use of gloves, but there is no indication of the situations in which they are needed. Gloves should be used only in contact with secretions, not always (Pittet & Boyce, 2003). Student 51’s comments thus show some professional knowledge and some lay knowledge, which is typical for the Mixed Model.
Eighteen of the 29 (62%) students’ mental models were classified as instances of the Mixed Model. Six of these students scored a maximum of 8 points from the multiple-true–false questions. The remaining students scored between 2 and 6 points.
The transmission model
The Transmission Model is based on scientific knowledge of IPC. In this model, the nurse is understood as the main pathogen spreading link between the patients (WHO, 2016), and it is acknowledged that the patients need to be protected against the spreading of pathogens by the HCWs’ hands. Hand disinfection, the cornerstone of IPC, is expected to be mentioned (Pittet & Boyce, 2003). In addition, the use of professional language is a characteristic of this model (see Table 1).
Only one of the concept maps (Student 18) was categorised as an instance of the Transmission Model. The student scored a maximum of 8 points on the multiple-true–false questions.
The student manifested professional knowledge in a written explanation by stating that the nurse is the pathogen spreading link “with poor hand hygiene healthcare workers spread diseases to other patients”, and the best way to prevent spreading of pathogens is hand disinfection “because hand disinfection is the most efficient and cheapest way to prevent the spreading of pathogens”. The student also used professional language (e.g., “pathogens”) (see Fig. 6).
Discussion
The purpose of this study was to make an inventory of the misconceptions of practical nurse students about IPC at the beginning of their studies, and to discover (1) what kind of IPC misconceptions are held by students, and (2) how prevalent they are. The Three Mental Models that were created based on the students’ justifications indicated that every third student maintained beliefs that were corresponding to a Household Hygiene Model. Patients and visitors, surfaces and secretions were seen as the main routes of transmission and hence should be cleaned. The use of gloves was emphasised, whereas neither the HCW nor hand disinfection were mentioned. This set of beliefs seems to serve a self-protection goal (Dapper et al., 2022; Jansson et al., 2016; Jeong & Kim, 2016). The Mixed Model was observed by almost two thirds of the students. It included the same kind of household beliefs, for instance claiming that bacteria spread easily from surfaces, but was enriched with some scientific knowledge of IPC, i.e., knowledge about the role of the HCWs in spreading disease and the importance of using hand rub before and after dealing with a patient. It is important that teachers are aware of how their students encounter hygiene in everyday life and what transgression of their in-built standards might mean to them. Teachers should not confuse almost perfect test results with understanding and practicing IPC, not even as an indicator that a student is on the right tract. Only one student expressed beliefs that are covered by the Transmission Model, reflecting scientific and discipline knowledge. The Transmission Model focuses on protecting the patient and is based on the scientific finding that the healthcare worker is the main route of transmission; hand disinfection plays a crucial role in disrupting this transmission route. Nevertheless, it should be noted that the Transmission Model is only a starting point for the HCW to learn very detailed IPC related routines for performing nursing procedures in compliance with the guidelines (Heininger et al., 2021; Purssell & Gould, 2022).
It can be concluded that all the students except one demonstrated beliefs that could be classified as household conception or mixed conceptions that have self-protection as a common value. A majority of the students also understood the role of healthcare workers in spreading disease and the importance of hand disinfection as a means to prevent this. At the same time, they believed that wearing gloves can also serve that role without necessarily being aware of the potential danger that gloves can also be transmitters. The study design makes it impossible to draw conclusions on how many students entertain specific lay beliefs. The extent of the students’ justifications for the answers to the multiple-true–false questions varied widely, which is a limitation of the study. Some of the participants provided elaborated responses, whereas others provided very short replies. However, this study provides evidence that a very small minority of the students at this stage of education have developed a scientific understanding of IPC in healthcare. These findings have implications for nursing education.
Our findings are in line with findings in healthcare practice. Researchers of compliance to hand hygiene standards in healthcare institutions have hypothesised that a preference for prioritising self-protection can explain part of the disappointing effects of promotional campaigns. Evidence for this is found in the discrepancy between hand rub ‘before patient contact’ (serving the patient) and ‘after patient contact’ (serving self). During the COVID-19 pandemic both increased dramatically but despite this the gap was not reduced (Israel et al., 2020).
The results of this study can be interpreted along the lines of transition from lay to scientific understanding. In this view, transformations of earlier knowledge and integration of scientific knowledge has to take place. In this process, knowledge fragmentation and formation of synthetic conceptions may take place (Vosniadou & Skopeliti, 2014), however, emotional or motivational factors may complicate these transitions (Curtis & Biran, 2001; Pintrich et al., 1993). The results are also in the line with earlier findings (Chi, 2013; Vosniadou & Skopeliti, 2014) that scientific mental models hardly exist in a “pure” form but include various perspectives simultaneously (e.g., Solomon, 1983). In the present study, it could even be claimed that the Household Hygiene Model represents a rather sophisticated set of knowledge and skills that can in no way be called naïve. It is the context and goal that define its applicability (WHO, 2009). We agree with the view of Lundholm (2018) and Halldén (1999) that the lay model and the scientific model may coexist in the minds of students and HCWs provided that students and HCWs are able to activate the scientific/professional model in a professional context (see Fig. 1). As Lundholm (2018) and Halldén (1999) emphasise: it is the learners who should become aware of their own mental models and build meta-knowledge about the relation and differences between the two, especially in regard to context demands and applicability.
Finally, the decision by an HCW to follow or not to follow IPC can also be considered a social dilemma. In a social dilemma, 1) the payoff for everyone to defect, i.e., act in self-interest, is higher than the payoff for acting in the interest of the collective regardless of what the others do, but 2) all individuals receive a lower payoff if all defects. There is a temptation for HCWs to discard IPC and to relapse into lay conceptions in the workplace simply because following IPC requires constant cognitive effort without immediate payoff to the individual. The temptation is even higher if the other HCWs are serving as poor role models (Cox et al., 2014; Oh, 2021). The study by Harring and Lundholm (2018) indicated that students with knowledge of social dilemmas showed more willingness to take personal responsibility in the context of mitigating climate change. Research on the incorporation of social dilemmas into teaching could be a direction for future research, as well as research on emotional and motivational complicating factors.
The practical implication of the study is that developing an awareness of students’ mental models in different situations related to hygiene, and their appropriateness to situation-specific demands, should be an explicit goal of nursing education. If the mental model of nurses does not involve the nurse as the pathogen-spreading link between patients, there is no reason for nurses to disinfect their hands or to learn about standard procedures. This awareness is referred to as “meta-knowledge” in Fig. 1. The ability to be aware of one’s thinking and to monitor one’s thinking in daily practice is important – even lifesaving, because in this context it is particularly easy to relapse into deeply-rooted thinking habits. We believe that the three mental models presented in this study can serve as reference points in class discussions on students’ understandings of IPC.
Availability of data and materials
As explained to the participants, the data will not be disclosed available to any third party.
References
Aarkrog, V., & Wahlgren, B. (2022). Goal orientation and decision-making in education. Vocations and Learning, 15(1), 71–86. https://doi.org/10.1007/s12186-021-09278-0
Ahopelto, I., Mikkilä-Erdmann, M., Olkinuora, E., & Kääpä, P. (2011). A follow-up study of medical students’ biomedical understanding and clinical reasoning concerning the cardiovascular system. Advances in Health Sciences Education, 16, 655–668. https://doi.org/10.1007/s10459-011-9286-3
AL-Rawajfah, O. M., & Tubaishat, A. (2015). Nursing students’ knowledge and practices of standard precautions: a Jordanian web-based survey. Nurse Education Today, 35(12), 1175–1180. https://doi.org/10.1016/j.nedt.2015.05.011
Boshuizen, H. P. A., & Marambe, K. N. (2020). Misconceptions in medicine, their origin and development in education and working life. International Journal of Educational Research, 100, 101536. https://doi.org/10.1016/j.ijer.2020.101536
Boshuizen, H. P. A., Vosniadou, S., & Lehtinen, E. (2020). Conceptual changes for and during working life. International Journal of Educational Research, 104, 101682. https://doi.org/10.1016/j.ijer.2020.101682
Caniza, M. A., Maron, G., Moore, E. J., Quintana, Y., & Liu, T. (2007). Effective hand hygiene education with the use of flipcharts in a hospital in El Salvador. Journal of Hospital Infection, 65(1), 58–64. https://doi.org/10.1016/j.jhin.2006.08.011
Chi, M. T. H. (2013). Two kinds and four sub-types of misconceived knowledge, ways to change it, and the learning outcomes. In S. Vosniadou (Ed.), International Handbook of Research on Conceptual Change (pp. 49–70). Routledge. https://doi.org/10.4324/9780203154472.ch3
Cieslak, P. R., Lee, L. E., Papafragkou, E., & An, N. (2009). Recurring norovirus outbreaks in a long-term residential treatment facility — Oregon, 2007. MMWR Morbidity and Mortality Weekly Report, 58(25), 694–698. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5825a2.htm
Cox, J. L., Simpson, M. D., Letts, W., & Cavanagh, H. M. A. (2014). Putting it into practice: Infection control professionals’ perspectives on early career nursing graduates’ microbiology and infection control knowledge and practice. Contemporary Nurse, 49(1), 83–92. https://doi.org/10.1080/10376178.2014.11081957
Curtis, V., & Biran, A. (2001). Dirt, disgust, and disease: Is hygiene in our genes? Perspectives in Biology and Medicine, 44(1), 17–31. https://doi.org/10.1353/pbm.2001.0001
Dapper, L., Dick, A., Nonnenmacher-Winter, C., & Günther, F. (2022). Influence of public health and infection control interventions during the severe acute respiratory syndrome coronavirus 2 pandemic on the in-hospital epidemiology of pathogens: In hospital versus community circulating pathogens. Antimicrobial Resistance & Infection Control, 11(1), 140. https://doi.org/10.1186/s13756-022-01182-z
Finnish National Agency for Education. (2018). Vocational Qualifications in Social and Health Care. https://eperusteet.opintopolku.fi/eperusteet-service/api/dokumentit/6671197
Guzzetti, B. J., Snyder, T. E., Glass, G. V., & Gamas, W. S. (1993). Promoting conceptual change in science: A comparative meta-analysis of instructional interventions from reading education and science education. Reading Research Quarterly, 28(2), 117–159. https://doi.org/10.2307/747886
Halldén, O. (1993). Leaners’ conceptions of the subject matter being taught A case from learning history. International Journal of Educational Research, 19(3), 317–325.
Halldén, O. (1999). Conceptual change and contextualisation. In W. Schnotz, S. Vosniadou, & M. Carretero (Eds.), New perspectives on conceptual change (pp. 53–65). Pergamon.
Halldén, O., Scheja, M., & Haglund, L. (2009). The contextuality of knowedge: An intentional approach to meaning making and conceptual change. In S. Vosniadou (Ed.), International handbook of research on conceptual change (pp. 537–560). Routledge.
Harring, N., & Lundholm, C. (2018). Does knowledge about social dilemmas generate cynical citizens? [Paper presentation]. American Political Science Association Annual Meeting, August 30-September 2, Boston, USA.
Heininger, S. K., Baumgartner, M., Zehner, F., Burgkart, R., Söllner, N., Berberat, P. O., & Gartmeier, M. (2021). Measuring hygiene competence: the picture-based situational judgement test HygiKo. BMC Medical Education, 21(1), 410. https://doi.org/10.1186/s12909-021-02829-y
Israel, S., Harpaz, K., Radvogin, E., Schwartz, C., Gross, I., Mazeh, H., Cohen, M. J., & Benenson, S. (2020). Dramatically improved hand hygiene performance rates at time of coronavirus pandemic. Clinical Microbiology and Infection, 26(11), 1566–1568. https://doi.org/10.1016/j.cmi.2020.06.002
Jansson, M. M., Syrjälä, H. P., Ohtonen, P. P., Meriläinen, M. H., Kyngäs, H. A., & Ala-Kokko, T. I. (2016). Simulation education as a single intervention does not improve hand hygiene practices: a randomized controlled follow-up study. American Journal of Infection Control, 44(6), 625–630. https://doi.org/10.1016/j.ajic.2015.12.030
Jeong, S. Y., & Kim, K. M. (2016). Influencing factors on hand hygiene behavior of nursing students based on theory of planned behavior: a descriptive survey study. Nurse Education Today, 36, 159–164. https://doi.org/10.1016/j.nedt.2015.09.014
Kelcíkova, S., Skodova, Z., & Straka, S. (2012). Effectiveness of hand hygiene education in a basic nursing school curricula. Public Health Nursing, 29(2), 152–159. https://doi.org/10.1111/j.1525-1446.2011.00985.x
Kısacık, Ö. G., Ciğerci, Y., & Güneş, Ü. (2021). Impact of the fluorescent concretization intervention on effectiveness of hand hygiene in nursing students: a randomized controlled study. Nurse Education Today, 97, 104719. https://doi.org/10.1016/j.nedt.2020.104719
Korhonen, A., Vuori, A., Lukkari, A., Laitinen, A., Perälä, M., Koskela, T., & Pölkki, T. (2019). Increasing nursing students’ knowledge of evidence-based hand-hygiene: A quasi-experimental study. Nurse Education in Practice, 35, 104–110. https://doi.org/10.1016/j.nepr.2018.12.009
Linn, M. C. (2008). Teaching for conceptual change: Distinguish or extinguish ideas. In S. Vosniadou (Ed.), International Handbook of Research on Conceptual Change (pp. 694–722). Routledge.
Lundholm, C. (2018). Conceptual change and the complexity of learning. In T. G. Amin & O. Levrini (Eds.), Converging Perspectives on Conceptual Change: Mapping an Emerging Paradigm in the Learning Sciences (pp. 34–42). Routledge. https://doi.org/10.4324/9781315467139
Lundholm, C. (2022). Conceptual change and teaching - focusing on social science and climate education. Keynote Speach Held at the 12th Conference on Conceptual Change, 8, 24–27. Zwolle, The Netherlands.
Merenluoto, K., & Lehtinen, E. (2004). Number concept and conceptual change: Towards a systemic model of the processes of change. Learning and Instruction, 14(5 SPEC.ISS), 519–534. https://doi.org/10.1016/j.learninstruc.2004.06.016
Mikkilä-Erdmann, M., Södervik, I., Vilppu, H., Kääpä, P., & Olkinuora, E. (2012). First-year medical students’ conceptual understanding of and resistance to conceptual change concerning the central cardiovascular system. Instructional Science, 40(5), 745–754. https://doi.org/10.1007/s11251-012-9212-y
Moll, L. C., Amanti, C., Neff, D., & Gonzalez, N. (1992). Funds of knowledge for teaching: Using a qualitative approach to connect homes and classrooms. Theory into Practice, 31(2), 132–141. https://doi.org/10.1080/00405849209543534
Oh, H. S. (2021). Knowledge, perception, and performance of hand hygiene and their correlation among nursing students in Republic of Korea. Healthcare, 9(7), 913. https://doi.org/10.3390/healthcare9070913
Patel, V. L., & Groen, G. J. (1986). Knowledge based solution strategies in medical reasoning. Cognitive Science, 10(1), 91–116. https://doi.org/10.1016/S0364-0213(86)80010-6. 10.1016/S0364-0213(86)80010-6.
Pintrich, P. R., Marx, R. W., & Boyle, R. A. (1993). Beyond cold conceptual change: the role of motivational beliefs and classroom contextual factors in the process of conceptual change. Review of Educational Research, 63(2), 167. https://doi.org/10.2307/1170472
Pittet, D., & Boyce, J. M. (2003). Revolutionising hand hygiene in health-care settings: guidelines revisited. The Lancet Infectious Diseases, 3(5), 269–270. https://doi.org/10.1016/S1473-3099(03)00601-7
Purssell, E., & Gould, D. (2022). Teaching health care students hand hygiene theory and skills: a systematic review. International Journal of Environmental Health Research, 32(9), 2065–2073. https://doi.org/10.1080/09603123.2021.1937580
Sairaalahygienia- ja infektiontorjuntayksikkö. (2023). Hoitoon liittyvien infektioiden torjunnan perusteet Varsinais-Suomen hyvinvointialueella. Varsinais-Suomen hyvinvointialue /Tyks Sairaalahygienia- ja infektiontorjuntayksikkö. https://hoito-ohjeet.fi/OhjepankkiVSSHP/Suositus hoitoon liittyvien infektioiden torjunnasta.pdf
Södervik, I., Mikkilä-Erdmann, M., & Chi, M. T. H. (2019). Conceptual change challenges in medicine during professional development. International Journal of Educational Research, 98(August 2018), 159–170. https://doi.org/10.1016/j.ijer.2019.07.003
Solomon, J. (1983). Learning about energy: How pupils think in two domains. European Journal of Science Education, 5(1), 49–59. https://doi.org/10.1080/0140528830050105
Suetens, C., Latour, K., Kärki, T., Ricchizzi, E., Kinross, P., Moro, M. L., Jans, B., Hopkins, S., Hansen, S., Lyytikäinen, O., Reilly, J., Deptula, A., Zingg, W., Plachouras, D., & Monnet, D. L. (2018). Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two european point prevalence surveys, 2016 to 2017. Eurosurveillance, 23(46), 1–17. https://doi.org/10.2807/1560-7917.ES.2018.23.46.1800516
Tversky, B. (2011). Visualizing Thought. Topics in Cognitive. Science, 3(3), 499–535. https://doi.org/10.1111/j.1756-8765.2010.01113.x
Van de Wiel, M. W. J., Boshuizen, H. P. A., & Schmidt, H. G. (2000). Knowledge restructuring in expertise development: evidence from pathophysiological representations of clinical cases by students and physicians. European Journal of Cognitive Psychology, 12(3), 323–356. https://doi.org/10.1080/09541440050114543
Virtanen, A. (2020). THL - Tilastoraportti 02/2020 Sosiaali- ja terveydenhuollon ammattioikeudet 2010 – 2018. https://www.julkari.fi/bitstream/handle/10024/139099/Tr02_20.pdf?sequence=5&isAllowed=y
Vosniadou, S., & Brewer, W. F. (1992). Mental models of the earth: a study of conceptual change in childhood. Cognitive Psychology, 24(4), 535–585. https://doi.org/10.1016/0010-0285(92)90018-W
Vosniadou, S., & Skopeliti, I. (2014). Conceptual change from the framework theory side of the fence. Science and Education, 23(7), 1427–1445. https://doi.org/10.1007/s11191-013-9640-3
Vosniadou, S., Ioannides, C., Dimitrakopoulou, A., & Papademetriou, E. (2001). Designing learning environments to promote conceptual change in science. Learning and Instruction, 11(4–5), 381–419. https://doi.org/10.1016/S0959-4752(00)00038-4
Ward, D. J. (2013). The barriers and motivators to learning infection control in clinical placements: interviews with midwifery students. Nurse Education Today, 33(5), 486–491. https://doi.org/10.1016/j.nedt.2012.05.024
White, R. T. (1994). Conceptual and conceptional change. Learning and Instruction, 4, 117–121. https://doi.org/10.1016/0959-4752(94)90022-1
WHO. (2009). WHO Guidelines on hand hygiene in health care. In World Health Organization (Vol. 30, Issue 1). World Health Organization Press. https://apps.who.int/iris/bitstream/handle/10665/70126/WHO_IER_PSP_2009.07_eng.pdf;sequence=1
WHO. (2016). Health care without avoidable infections: The critical role of infection prevention and control. World Health Organization. https://www.who.int/publications/i/item/health-care-without-avoidable-infections-the-critical-role-of-infection-prevention-and-control
Code availability
Not applicable.
Funding
Open Access funding provided by University of Turku (including Turku University Central Hospital). A total of EUR 3000 from the OPPI doctoral programme.
Author information
Authors and Affiliations
Contributions
The first author conceptualised, planned, collected the data, and wrote the original draft. All authors participated in the conceptualisation of the study, analysis of the results, reviewing, and editing the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was granted ethical approval by the Ethical Review Board of the Finnish university involved in the study. The principal of the vocational school granted the research permit.
Consent for publication
The students who volunteered to participate in this study were debriefed about the study beforehand and signed an Informed Consent Form. Each authors has read and approved the final version of the paper.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
The multiple-true–false questions
 = correct answer,
= correct answer,
 = incorrect answer
= incorrect answer

Appendix 2
The two prototypical concept maps; Household Hygiene Model on the left and Transmission Model on the right side

(P = patient, X = preventing transmission of pathogens, HD = hand disinfection, HH = hand hygiene, HW = hand wash, HCW = healthcare worker, → = affects, causes)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eronen, R., Helle, L., Palonen, T. et al. Practical nurse students’ misconceptions about infection prevention and control. Vocations and Learning 17, 143–164 (2024). https://doi.org/10.1007/s12186-023-09337-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12186-023-09337-8