Abstract
Background
Platelet transfusion refractoriness (PTR) remains an intractable issue in clinical practice, and is common in hematological patients. At present, it is believed that both immune and non-immune factors play a role. We conducted a meta-analysis of various risk factors which may contribute to PTR.
Methods
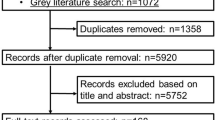
PubMed, Embase, Cochrane library, and Web of Science were selected as research database platforms. Citations included were further assessed for quality and bias using the Newcastle–Ottawa Scale. All analyses were performed using Review Manager Version 5.4 and STATA 16.0.
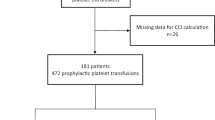
Results
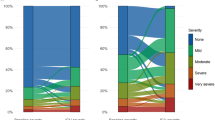
The preliminary search revealed 1069 publications, and 17 (5929 patients in total) were ultimately included in the quantitative analysis. The following variables were associated with the occurrence of PTR: fever (OR = 2.26, 95%CI 2.00–2.55, p < 0.00001), bleeding (OR = 2.10, 95%CI 1.36–3.24, p = 0.0008), female sex (OR = 2.06, 95%CI 1.13–3.75, p = 0.02), antibiotic use (OR = 2.94, 95%CI 1.54–5.59, p = 0.001), and infection (OR = 2.19, 95%CI 1.20–4.03, p = 0.01). Antibodies involved in immune activation were a higher risk factor (OR = 4.17, 95%CI 2.36–7.36, p < 0.00001), and splenomegaly was nearly significant (OR = 1.73, 95%CI 0.97–3.07, p = 0.06).
Conclusions
We identified some important risk factors for PTR, but further research is needed to identify the many other possible elements that may contribute to or mediate PTR.






Similar content being viewed by others
Data availability
Raw materials supporting the above-mentioned conclusions will be available without undue reservation if requested.
References
Forest SK, Hod EA. Management of the platelet refractory patient. Hematol Oncol Clin North Am. 2016;30(3):665–77. https://doi.org/10.1016/j.hoc.2016.01.008.
Saris A, Pavenski K. Human leukocyte antigen alloimmunization and alloimmune platelet refractoriness. Transfus Med Rev. 2020;34(4):250–7. https://doi.org/10.1016/j.tmrv.2020.09.010.
Slichter SJ, Davis K, Enright H, Braine H, Gernsheimer T, Kao KJ, et al. Factors affecting posttransfusion platelet increments, platelet refractoriness, and platelet transfusion intervals in thrombocytopenic patients. Blood. 2005;105(10):4106–14. https://doi.org/10.1182/blood-2003-08-2724.
Belizaire R, Makar RS. Non-alloimmune mechanisms of thrombocytopenia and refractoriness to platelet transfusion. Transfus Med Rev. 2020;34(4):242–9. https://doi.org/10.1016/j.tmrv.2020.09.002.
Juskewitch JE, Norgan AP, De Goey SR, Duellman PM, Wakefield LL, Gandhi MJ, et al. How do I … manage the platelet transfusion-refractory patient? Transfusion. 2017;57(12):2828–35. https://doi.org/10.1111/trf.14316.
Arabi S, Almahayni AO, Alomair AA, Masuadi EM, Damlaj M, Al-Dorzi HM. Prevalence, Risk Factors, and Outcomes of Platelet Transfusion Refractoriness in Critically Ill Patients: A Retrospective Cohort Study. Crit Care Res Pract. 2021;2021:5589768. https://doi.org/10.1155/2021/5589768.
Balduini CL, Salvaneschi L, Klersy C, Noris P, Mazzucco M, Rizzuto F, et al. Factors influencing post-transfusional platelet increment in pediatric patients given hematopoietic stem cell transplantation. Leukemia. 2001;15(12):1885–91. https://doi.org/10.1038/sj.leu.2402307.
Baron E, Charpentier J, François A, Ben Hadj Amor H, Habr B, Cariou A, et al. Post-transfusion platelet responses in critically ill cancer patients with hypoproliferative thrombocytopenia. Transfusion. 2020;60(2):275–84. https://doi.org/10.1111/trf.15596.
Beligaswatte A, Tsiopelas E, Humphreys I, Bennett G, Robinson K, Davis K, et al. The mean fluorescence intensities of anti-HLA antibodies detected using micro-bead flow cytometry predict the risk of platelet transfusion refractoriness. Br J Haematol. 2013;162(3):409–12. https://doi.org/10.1111/bjh.12369.
Chenna D, Shastry S, Baliga P. Evaluation and monitoring of response to platelet transfusion therapy: experience from a tertiary care center. Acta Clin Belg. 2021;76(4):300–3. https://doi.org/10.1080/17843286.2020.1732568.
Cheok KPL, Chhetri R, Wee LYA, Friel O, Pham A, Salvi A, et al. The burden of immune-mediated refractoriness to platelet transfusions in myelodysplastic syndromes. Transfusion. 2020;60(10):2192–8. https://doi.org/10.1111/trf.16029.
Hu X, Cai H, Zheng L, Luo Y, Zhou J, Hui Y, et al. Clinical and immunological features of platelet transfusion refractoriness in young patients with de novo acute myeloid leukemia. Cancer Med. 2020;9(14):4941–8. https://doi.org/10.1002/cam4.3140.
Kerkhoffs JL, Eikenboom JC, van de Watering LM, van Wordragen-Vlaswinkel RJ, Wijermans PW, Brand A. The clinical impact of platelet refractoriness: correlation with bleeding and survival. Transfusion. 2008;48(9):1959–65. https://doi.org/10.1111/j.1537-2995.2008.01799.x.
Kumawat V, Sharma RR, Malhotra P, Marwaha N. Prevalence of risk factors for platelet transfusion refractoriness in multitransfused hemato-oncological patients at tertiary care center in North India. Asian J Transfus Sci. 2015;9(1):61–4. https://doi.org/10.4103/0973-6247.150953.
Mishima Y, Tsuno NH, Matsuhashi M, Yoshizato T, Sato T, Ikeda T, et al. Effects of universal vs bedside leukoreductions on the alloimmunization to platelets and the platelet transfusion refractoriness. Transfus Apher Sci. 2015;52(1):112–21. https://doi.org/10.1016/j.transci.2014.11.001.
Seftel MD, Growe GH, Petraszko T, Benny WB, Le A, Lee CY, et al. Universal prestorage leukoreduction in Canada decreases platelet alloimmunization and refractoriness. Blood. 2004;103(1):333–9. https://doi.org/10.1182/blood-2003-03-0940.
Shastry S, Chaudhary R. Clinical factors influencing corrected count increment. Transfus Apher Sci. 2012;47(3):327–30. https://doi.org/10.1016/j.transci.2012.04.006.
Solves P, Sanz J, Freiria C, Santiago M, Villalba A, Gómez I, et al. Factors influencing platelet transfusion refractoriness in patients undergoing allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2018;97(1):161–7. https://doi.org/10.1007/s00277-017-3168-6.
Song T, Zhang Y, Huang J, Liu Z. Transfusion-induced platelet antibodies and regulatory T cells in multiply transfused patients. J Clin Lab Anal. 2021;35(7):e23864. https://doi.org/10.1002/jcla.23864.
Tanoue S, Konuma T, Kato S, Oiwa-Monna M, Isobe M, Jimbo K, et al. Platelet transfusion refractoriness in single-unit cord blood transplantation for adults: risk factors and clinical outcomes. Biol Blood Marrow Transplant. 2018;24(9):1873–80. https://doi.org/10.1016/j.bbmt.2018.05.006.
Wong M, Narra R, Selim M, Zimmerman MA, Kim J, Padmanabhan A, et al. Human leukocyte antigen class I antibodies and response to platelet transfusion in patients undergoing liver transplantation. J Surg Res. 2020;255:99–105. https://doi.org/10.1016/j.jss.2020.05.029.
Zhou Z, Gao Y, Li X, Ren J, Liu Y, Li J. The clinical characteristics of patients with acute leukemia or stem cell transplantation exhibiting immune based platelet refractoriness. Transfus Apher Sci. 2020;59(3):102725. https://doi.org/10.1016/j.transci.2020.102725.
Liu Y, Zhang Y, Chen D, Fu Y. Current status of and global trends in platelet transfusion refractoriness from 2004 to 2021: a bibliometric analysis. Front Med. 2022;9:873500. https://doi.org/10.3389/fmed.2022.873500.
Schiffer CA, Bohlke K, Delaney M, Hume H, Magdalinski AJ, McCullough JJ, et al. Platelet transfusion for patients with cancer: American society of clinical oncology clinical practice guideline update. J Clin Oncol. 2018;36(3):283–99. https://doi.org/10.1200/jco.2017.76.1734.
Stanworth SJ, Navarrete C, Estcourt L, Marsh J. Platelet refractoriness–practical approaches and ongoing dilemmas in patient management. Br J Haematol. 2015;171(3):297–305. https://doi.org/10.1111/bjh.13597.
Legler TJ, Fischer I, Dittmann J, Simson G, Lynen R, Humpe A, et al. Frequency and causes of refractoriness in multiply transfused patients. Ann Hematol. 1997;74(4):185–9. https://doi.org/10.1007/s002770050280.
Ojha A, Nandi D, Batra H, Singhal R, Annarapu GK, Bhattacharyya S, et al. Platelet activation determines the severity of thrombocytopenia in dengue infection. Sci Rep. 2017;7:41697. https://doi.org/10.1038/srep41697.
Bishop JF, McGrath K, Wolf MM, Matthews JP, De Luise T, Holdsworth R, et al. Clinical factors influencing the efficacy of pooled platelet transfusions. Blood. 1988;71(2):383–7.
Chu T, Tang Y, Wang H, Qi J, Zhao Y, Pan T, et al. Efficacy of recombinant factor VIIa for severe bleeding complicated by platelet transfusion refractoriness in patients with hematologic malignancies. Thromb Res. 2017;160:14–8. https://doi.org/10.1016/j.thromres.2017.10.015.
Aster RH. Pooling of platelets in the spleen: role in the pathogenesis of “hypersplenic” thrombocytopenia. J Clin Invest. 1966;45(5):645–57. https://doi.org/10.1172/jci105380.
Hussein MA, Lee EJ, Schiffer CA. Platelet transfusions administered to patients with splenomegaly. Transfusion. 1990;30(6):508–10. https://doi.org/10.1046/j.1537-2995.1990.30690333480.x.
Mauro M, Camoglio F, Piccoli P, De Bortoli M, Balter R, Pegoraro A, et al. The use of splenectomy to manage platelet transfusion refractoriness due to anti-human leukocyte antibodies in allogeneic stem cell transplantation. Pediatr Rep. 2016;8(1):6159. https://doi.org/10.4081/pr.2016.6159.
Trial to Reduce Alloimmunization to Platelets Study Group. Leukocyte reduction and ultraviolet B irradiation of platelets to prevent alloimmunization and refractoriness to platelet transfusions. N Engl J Med. 1997;337(26):1861–9. https://doi.org/10.1056/nejm199712253372601.
Ma N, Guo JP, Zhao XY, Xu LP, Zhang XH, Wang Y, et al. Prevalence and risk factors of antibodies to HLA according to different cut-off values of mean fluorescence intensity in haploidentical allograft candidates: A prospective study of 3805 subjects. Hla. 2022;100(4):312–24. https://doi.org/10.1111/tan.14704.
Ruggero MA, Abdelghany O, Topal JE. Vancomycin-induced thrombocytopenia without isolation of a drug-dependent antibody. Pharmacotherapy. 2012;32(11):e321–5. https://doi.org/10.1002/phar.1132.
Mohammadi M, Jahangard-Rafsanjani Z, Sarayani A, Hadjibabaei M, Taghizadeh-Ghehi M. Vancomycin-induced thrombocytopenia: a narrative review. Drug Saf. 2017;40(1):49–59. https://doi.org/10.1007/s40264-016-0469-y.
Chan CS, Tuazon CU, Lessin LS. Amphotericin-B-induced thrombocytopenia. Ann Intern Med. 1982;96(3):332–3. https://doi.org/10.7326/0003-4819-96-3-332.
Böck M, Muggenthaler KH, Schmidt U, Heim MU. Influence of antibiotics on posttransfusion platelet increment. Transfusion. 1996;36(11–12):952–4. https://doi.org/10.1046/j.1537-2995.1996.36111297091736.x.
McGrath K, Bertram JF, Houghton S, Boothman J, Manderson JA, Minchinton R. Amphotericin B-induced injury in stored human platelets. Transfusion. 1992;32(1):46–50. https://doi.org/10.1046/j.1537-2995.1992.32192116432.x.
Murphy S. Amphotericin B and platelet transfusion. Transfusion. 1992;32(1):7–8. https://doi.org/10.1046/j.1537-2995.1992.32192116437.x.
Li Y, Ryan J, Xu F, Vostal JG. Macrophage depletion mitigates platelet aggregate formation in splenic marginal zone and alleviates lps-associated thrombocytopenia in rats. Front Med. 2019;6:300. https://doi.org/10.3389/fmed.2019.00300.
Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the sepsis-3 definitions in critically Ill children. JAMA Pediatr. 2017;171(10):e172352. https://doi.org/10.1001/jamapediatrics.2017.2352.
Pavenski K, Freedman J, Semple JW. HLA alloimmunization against platelet transfusions: pathophysiology, significance, prevention and management. Tissue Antigens. 2012;79(4):237–45. https://doi.org/10.1111/j.1399-0039.2012.01852.x.
Wu KK, Thompson JS, Koepke JA, Hoak JC, Flink R. Heterogeneity of antibody response to human platelet transfusion. J Clin Invest. 1976;58(2):432–8. https://doi.org/10.1172/jci108487.
Curtis BR, McFarland JG. Human platelet antigens-2013. Vox Sang. 2014;106(2):93–102. https://doi.org/10.1111/vox.12085.
Kurz M, Greinix H, Höcker P, Kalhs P, Knöbl P, Mayr WR, et al. Specificities of anti-platelet antibodies in multitransfused patients with haemato-oncological disorders. Br J Haematol. 1996;95(3):564–9. https://doi.org/10.1046/j.1365-2141.1996.d01-1936.x.
Cohn CS. Platelet transfusion refractoriness: how do I diagnose and manage? Hematol Am Soc Hematol Educ Program. 2020;2020(1):527–32. https://doi.org/10.1182/hematology.2020000137.
Vassallo RR. Recognition and management of antibodies to human platelet antigens in platelet transfusion-refractory patients. Immunohematology. 2009;25(3):119–24.
Saito K, Ichikawa S, Ohtomo R, Hatta S, Katsuoka Y, Harigae H, et al. Severe platelet transfusion refractoriness due to anti-HPA-5a antibody during induction chemotherapy for acute promyelocytic leukemia. Ann Hematol. 2022;101(9):2103–5. https://doi.org/10.1007/s00277-022-04875-y.
Inoue H, Sakamoto R, Nishimiya H, Sakamoto H, Terasu S, Aminaka R, et al. Minor impact of patient alloantibodies against human platelet antigen (HPA)-15 in the effectiveness of platelet transfusion: a pilot study. Transfusion. 2021;61(3):738–43. https://doi.org/10.1111/trf.16181.
Liu J, Shao Y, Ding H, Deng J, Xu X, Wang J, et al. Distribution of CD36 deficiency in different Chinese ethnic groups. Hum Immunol. 2020;81(7):366–71. https://doi.org/10.1016/j.humimm.2020.05.004.
Flesch BK, Scherer V, Opitz A, Ochmann O, Janson A, Steitz M, et al. Platelet CD36 deficiency is present in 2.6% of Arabian individuals and can cause NAIT and platelet refractoriness. Transfusion. 2021;61(6):1932–42. https://doi.org/10.1111/trf.16398.
Schmidt AE, Sahai T, Refaai MA, Sullivan M, Curtis BR. Severe platelet transfusion refractoriness in association with antibodies against CD36. Lab Med. 2020;51(5):540–4. https://doi.org/10.1093/labmed/lmz091.
Funding
This work was supported by the National Natural Science Foundation of China (81873432 and 82070143), grants from the Jiangsu Province of China (BE2021645), and the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author information
Authors and Affiliations
Contributions
XFS did the retrieval of literatures. XFS and XQL extracted data from included studies. XFS, JQ Qi, and KF participated in data analysis and interpretation. XFS wrote the article. YH conceived of the study, participated in its design and coordination, and helped to draft the manuscript. All authors read and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors had a conflict of interest.
Ethical approval
Not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Song, X., Qi, J., Fang, K. et al. A meta-analysis of risk factors associated with platelet transfusion refractoriness. Int J Hematol 117, 863–875 (2023). https://doi.org/10.1007/s12185-023-03557-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-023-03557-3