Abstract
Background and Objective
Evidence-based guidelines on platelet transfusion therapy assist clinicians to optimize patient care, but currently do not take into account costs associated with different methods used during the preparation, storage, selection and dosing of platelets for transfusion. This systematic review aimed to summarize the available literature regarding the cost effectiveness (CE) of these methods.
Methods
Eight databases and registries, as well as 58 grey literature sources, were searched up to 29 October 2021 for full economic evaluations comparing the CE of methods for preparation, storage, selection and dosing of allogeneic platelets intended for transfusion in adults. Incremental CE ratios, expressed as standardized cost (in 2022 EUR) per quality-adjusted life-year (QALY) or per health outcome, were synthesized narratively. Studies were critically appraised using the Philips checklist.
Results
Fifteen full economic evaluations were identified. Eight investigated the costs and health consequences (transfusion-related events, bacterial and viral infections or illnesses) of pathogen reduction. The estimated incremental cost per QALY varied widely from EUR 259,614 to EUR 36,688,323. For other methods, such as pathogen testing/culturing, use of apheresis instead of whole blood-derived platelets, and storage in platelet additive solution, evidence was sparse. Overall, the quality and applicability of the included studies was limited.
Conclusions
Our findings are of interest to decision makers who consider implementing pathogen reduction. For other preparation, storage, selection and dosing methods in platelet transfusion, CE remains unclear due to insufficient and outdated evaluations. Future high-quality research is needed to expand the evidence base and increase our confidence in the findings.
Similar content being viewed by others
This is the first systematic review of full economic evaluations on the cost effectiveness of methods for the preparation, storage, selection and dosing of platelets for transfusion. |
Eight evaluations on the costs and health effects (adverse events, bacterial and viral infections or ilnesses) of pathogen reduction indicate that this technology has an estimated incremental cost per QALY ranging from EUR 259,614 to EUR 36,688,323. For other methods, such as pathogen testing/culturing, use of apheresis instead of whole blood-derived platelets, and storage in platelet additive solution, the evidence is sparse. |
Additional evaluations that use up-to-date efficacy and safety data and adequately assess the consistency of the applied models are needed to expand and strengthen the evidence base in order to facilitate informed decision making. |
1 Introduction
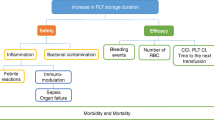
Platelet transfusions can be administered prophylactically or therapeutically to prevent or control bleeding, respectively, in patients with low platelet counts (thrombocytopenia). Platelet products can be obtained in two ways. Apheresis platelets are collected from a single donor, where a machine draws blood, isolates the platelets and returns the remaining blood back to the donor. Pooled platelets on the other hand are obtained by pooling four to six whole blood donations and extracting the platelets using either the buffy coat or platelet-rich plasma method. To reduce the risks associated with platelet transfusions, such as sepsis due to bacterial contamination, haemolysis (destruction of red blood cells) and platelet refractoriness (persistent suboptimal platelet count increments occurring after platelet transfusion), different strategies have been introduced during the platelet preparation phase. Bacterial risk control strategies recommended by the US Food and Drug Administration include bacterial testing/culturing and pathogen reduction [1]. The latter aims to impair the ability of viruses, bacteria and parasites to replicate, and involves the use of photochemicals that interact with the pathogen DNA and/or RNA and cross-link following exposure to UVA or visible light. In addition, leucodepletion or leucoreduction, referring to the process of removing white blood cells from a unit using centrifugation or filtration, has been shown to decrease alloimmunization (where an immune response is induced to foreign antigens in the blood of another human) and platelet refractoriness [2].
Platelet products can only be stored for a maximum of 4–7 days at room temperature, depending on national guidelines and type of product. Transfusion of older platelets has been shown to lead to increased risks of transfusion reactions, a higher number of platelet transfusions and a higher risk of bleeding [3]. Replacing the major part of the plasma by artificial platelet additive solutions (PAS) may not only increase storage time, thereby reducing waste, but may also lead to better patient outcomes [4].
The selection of ABO-identical platelets has been suggested to help avoid haemolytic transfusion reactions and the development of platelet refractoriness, but may not be feasible for all patients because of limited inventory [5, 6]. In addition, exclusively using ABO-matched platelets leads to platelet waste and may put additional pressure on the blood collection services. Selecting platelet products that are matched for human leucocyte antigen (HLA) is best practice in patients with platelet alloimmune refractoriness [2].
When it comes to dosing, a Cochrane systematic review found no evidence of a difference in the risk of clinically significant bleeding, the frequency or the severity of bleeding between low-dose (1.1 × 1011/m2), standard-dose (2.2 × 1011/m2) or high-dose (4.4 × 1011/m2) platelet transfusions [7]. Low-dose transfusions decrease the total amount of platelets patients received, but at the expense of a higher number of transfusions episodes. Increasing the dose from a standard to a high dose does not increase the transfusion interval, but may lead to an increase in transfusion-related adverse events. Therefore, guidelines recommend low-dose or standard-dose (as opposed to high-dose) prophylactic platelet transfusion for hospitalized patients with low platelet counts due to low platelet production [5].
Evidence-based guidelines are available to help clinicians decide on the appropriate use of platelets or platelet alternatives [8, 9]. However, these guidelines currently do not take into account the costs associated with the different methods used during preparation, storage, selection and dosing of platelets for transfusion. Like for any health intervention, it is important to determine if the value of these platelet preparation, storage, selection and dosing interventions justify their costs. A recent scoping review revealed that currently no systematic reviews exist to summarize the available literature regarding the cost effectiveness of these interventions [10]. The current systematic review therefore aims to fill in this research gap, thereby serving as an information source for future platelet transfusion guideline panels formulating recommendations.
2 Methods
This systematic review was planned and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA checklist, Online Resource 1, see electronic supplementary material [ESM]), and was registered prospectively in the PROSPERO International prospective register of systematic reviews as CRD42022301802. Online Resource 2 (see ESM) contains an extended version of this Methods section. In short, we included full economic evaluations that compared both the costs and consequences of different methods for preparation (e.g. apheresis vs whole blood-derived platelets, pathogen reduction vs no reduction), storage (e.g. temperature, duration, use of PAS), selection (e.g. ABO-matched vs unmatched platelets, HLA-matched vs unmatched) and dosing (e.g. low dose vs standard dose) of allogeneic platelets intended for transfusion in adults. Peer-reviewed publications, conference abstracts, conference papers, reports from national health authority agencies for health technology assessments and clinical trial registrations with study results reported were eligible. No restrictions were placed regarding the language or publication date of the publications.
Search strings (see Online Resource 3 in the ESM), consisting of free-text words and indexing terms, were designed to search for relevant publications in eight databases: MEDLINE (PubMed interface), The Cochrane Central Register of Controlled Trials, Embase (Embase.com interface), CINAHL (EBSCO interface), Transfusion Evidence Library, Web of Science Core Collection, International Network of Agencies for Health Technology Assessment International HTA database and ClinicalTrials.gov. The search was performed on 19 October 2021, without restrictions regarding publication dates or language. Additionally, we searched the websites of the HTA agencies and Health Economics institutions included in the ‘Grey Matters’ resource of the Canadian Agency for Drugs and Technologies in Health [11].
Studies were screened for eligibility by two reviewers independently (JL and BA), first at title and abstract and afterwards at full-text level, in the systematic review management tool Covidence [12]. Data extraction and critical appraisal was performed by two reviewers independently (JL and HVR/HS). Reporting quality was assessed via the Philips reporting checklist for economic evaluations [13], a relevant tool for the critical appraisal of model-based economic evaluations [14] that addresses 56 reporting items across three main domains: structure, data and consistency. In addition, the most important strengths and weaknesses of each study were identified, in collaboration with a content expert panel (JG, SN, NS, SS, VC). Discrepancies between reviewers regarding study selection, data extraction and quality appraisal were resolved by discussion. Where necessary, a third reviewer could be consulted (HVR/HS).
All cost data were inflation-adjusted to December 2022 and converted into the same currency (EUR), in accordance with the Professional Society for Health Economics and Outcomes Research (ISPOR) CiCERO checklist for systematic literature reviews that summarize cost and cost-effectiveness outcomes [14]. Meta-analyses were not planned given the anticipated heterogeneity in included models’ input variables and assumptions. Findings were synthesized narratively.
3 Results
3.1 Search Results
A total of 7278 unique records were screened, of which 15 met our eligibility criteria (Fig. 1). Online Resource 4 lists the excluded studies, as well as the seven studies labelled 'awaiting classification' because they provided insufficient information to make a justified decision to include or exclude them (see ESM).
3.2 Characteristics of Included Studies
Detailed information about the study characteristics can be found in Table 1.
More than half of the evaluations took place in the United States (US) [15,16,17,18,19,20,21,22], whereas one concerned Canada [23]. Five studies pertained to Europe: two to the Netherlands [24, 25] and one each to Belgium [26], Poland [27] and the United Kingdom [28]. One study was performed in Japan [29].
Most of the evaluations were published in the 2000s (n = 6 [17, 19, 24,25,26, 29]) and the 2010s (n = 6 [15, 18, 20, 23, 27, 28]). One and two evaluations dated from the 1980s [22] and 1990s [16, 21], respectively.
Eight evaluations were cost-utility analyses [15, 17, 21, 23, 24, 26, 27, 29]. The others included were cost-effectiveness analyses (n = 4 [16, 19, 25, 28]), cost-consequence analyses (n = 2 [18, 20]) and cost-benefit analyses (n = 1 [22]).
A lifetime horizon was reported by four evaluations [15, 21, 24, 25] and assumed by us to be adopted by four other evaluations [17, 23, 26, 29]. Two studies applied an in-hospital time horizon [18, 19], whereas two others used a 5-year time horizon [16, 22]. Kacker et al. [20] used a 1-year time horizon, whereas the time horizons were unclear for Agapova et al. 2015 and SaBTO [27, 28].
Three evaluations were conducted from the societal perspective [15, 25, 26], whereas three others chose the healthcare perspective [23, 24, 27]. The remaining evaluations were conducted from the hospital perspective (n = 2 [18, 20]), the blood centre perspective (n = 1 [22]), or failed to report the perspective (n = 6 [16, 17, 19, 21, 28, 29]).
Costs considered in the included studies are presented in Online Resource 5 (see ESM). Most evaluations included direct medical costs associated with the methods/technologies used (i.e. costs of consumables, equipment and labour), the transfusion, and the diagnosis, treatment and monitoring of adverse transfusion reactions. Consistent with their societal perspective, the evaluations by Agapova et al. 2010 [15], Moeremans et al. [26] and Postma et al. [25] additionally considered indirect costs, such as the cost of work productivity loss. One evaluation did not report on the cost items included [19].
Treatment effects described in the evaluations concerned platelet transfusion efficacy (e.g. refractoriness), safety (e.g. allergic transfusion reaction, sepsis, febrile reaction, bacterial or viral infection and subsequent disease, mortality) and/or quality of life (utilities) (Online Resource 6, see ESM).
Nearly all evaluations (14/15) covered methods used during the preparation of platelets. Eight of them evaluated the costs and effects of pathogen reduction [17, 23,24,25,26,27,28,29]. The other six covered parasite testing [15], bacterial testing/culturing [18, 24] and use of apheresis versus whole blood platelets [19, 21, 22]. Storage in PAS [20] and HLA-matching [22] were the other evaluated topics. Balducci et al. [16] compared the use of leucoreduced blood components until alloimmunization occurred and of crossmatch-compatible single-donor platelets thereafter to two other strategies: (1) the use of unfiltered pooled platelets until alloimmunization developed and of crossmatch-compatible single-donor platelets thereafter; and (2) the use of single-donor platelets from the beginning. None of the identified economic evaluations covered the dosing of platelets.
3.3 Summary of Cost-Effectiveness Findings
Tables 2 and 3 provide a summarized overview of the costs per quality-adjusted life-year (QALY) and per health outcome, respectively, sorted by method, with all cost data inflation-adjusted to December 2022 and converted to EUR using the average annual exchange rates of 2022. A narrative description according to method, using these 2022 EUR cost data, is provided in the following paragraphs. Detailed information on cost effectiveness estimates can be found in Online Resource 7, with costs presented in original values in the original currency, as reported by the study authors (see ESM).
3.3.1 Platelet Preparation: Pathogen Reduction
Seven of the eight evaluations on pathogen reduction modelled the estimated incremental cost per QALY, which ranged from EUR 259,614 to EUR 36,688,323.
In Agapova et al. 2015 [27], modelling pathogen reduction technology (PRT) for plasma and platelet components (PP-PRT) as an addition to the current safety interventions in Poland (i.e. serological and/or nucleic acid testing for HIV, HBV, HCV and syphilis, and in roughly 10% of the cases: gamma irradiation and cytomegalovirus screening) was estimated to cost EUR 435,141 per QALY. The results were most sensitive to the residual risk of bacterial contamination; the higher the risk, the higher the cost effectiveness of PP-PRT. In comparison with using pathogen reduction technology for plasma only (P-PRT) in combination with the current safety interventions, the cost of introducing PP-PRT was EUR 259,614 per QALY. The probability of PP-PRT being cost effective compared with P-PRT was higher across a range of willingness-to-pay thresholds (EUR 294,014–1,087,850 per QALY).
In a Canadian model by Custer et al. [23], using PP-PRT on top of the current blood safety screening (i.e. serological and/or nucleic acid testing for HIV, HCV, HBV, HTLV, syphilis and West Nile Virus) resulted in an estimate of EUR 1,420,767 per QALY. Cost effectiveness was most dependent on mortality rates in the year of transfusion (the lower the rate, the more cost effective), mortality rates associated with the type of blood components received (the lower, the more cost effective), the platelet preparation method used on whole blood (buffy-coat vs plasma-rich platelet method; the latter was more cost effective) and the percentage of single-donor apheresis platelets (the lower, the more cost effective).
The Dutch model of Janssen et al. [24] investigated the cost effectiveness of pathogen reduction and bacterial culturing in a setting where the diversion pouch is standard practice during blood collection. This pouch diverts the first 20–30 mL of blood, which is most likely to be contaminated by skin pathogens, thereby serving as a way to prevent bacterial contamination of the collected blood. The incremental cost per QALY for pathogen reduction was estimated at EUR 589,529. When compared with bacterial culturing, the estimate for pathogen reduction was EUR 4,268,592 per QALY. The main parameters affecting the cost effectiveness of pathogen reduction were the probability of sepsis given bacterial contamination (the higher, the more cost effective), the patients’ quality-adjusted life expectancy, the probability of death given sepsis, and the probability of bacterial contamination. For all these parameters, higher values yielded high cost effectiveness of pathogen reduction.
In a report by the Advisory Committee on the Safety of Blood, Tissues and Organs [28], which has an advisory role towards UK ministers and health departments on the most appropriate ways to ensure safe blood transfusions among others, pathogen reduction was compared with the current measures of gamma irradiation and bacterial and viral screening. However, it was unclear if the model assumed the introduction of pathogen reduction in addition to the current safety measures. The estimated incremental cost per QALY for patients aged <60 years when introducing three pathogen reduction systems in the UK varied from EUR 5,037,514 to EUR 13,482,760, assuming 35% apheresis platelets, a 0.75% reduction in wastage, and a 5% increase in demand to due pathogen reduction. Using 20% apheresis platelets was more cost effective, whereas using 50% apheresis platelets was less cost effective than 35%. When a 0% increase in platelet demand was assumed, cost effectiveness increased. Sensitivity analyses were carried out with alternative infectivity levels of variant Creutzfeldt Jakob disease and with alternative effectiveness rates of pathogen reduction. Higher infectivity levels resulted in lower cost effectiveness, whereas higher effectiveness rates of pathogen reduction lead to higher cost effectiveness.
Four studies investigated the cost effectiveness of the INTERCEPT™ Blood System [17, 25, 26, 29]. Bell et al. [17], Moeremans et al. [26] and Staginnus and Corash [29] modelled the estimated incremental cost per QALY, ranging from EUR 628,541 to EUR 36,688,323.
The Japanese model by Staginnus and Corash (2004) [29] showed that the incremental cost per QALY of using the INTERCEPT™ Blood System on single-donor apheresis platelets ranged from EUR 2,040,522 (60-year-old man undergoing coronary artery bypass grafting) to EUR 8,348,297 (70-year-old woman undergoing hip arthroplasty), when compared with the current safety measures of gamma irradiation, bacterial testing and viral testing. Cost effectiveness improved markedly with higher fatality rates due to bacterial contamination of platelet components and transfusion-related infection risk of a new emerging virus.
Although it is not clearly reported, Bell et al. [17] presumably compared the cost effectiveness of INTERCEPT™ in addition to the current safety measures in the US (viral testing and gamma irradiation) with that of the current safety measures alone. The model estimate ranged from EUR 3,555,439 (70-year-old woman undergoing hip arthroplasty) to EUR 7,110,898 (50-year-old man undergoing haematopoietic progenitor cell transplant for non-Hodgkin's lymphoma) per QALY. When using INTERCEPT™ in addition to bacterial testing, and comparing this to bacterial testing alone, the cost increased to EUR 17,087,383 (hip arthroplasty) and EUR 36,688,323 (non-Hodgkin's lymphoma). When introducing INTERCEPT™ to random-donor pooled platelet concentrates, the incremental cost per QALY was EUR 1,407,954 (hip arthroplasty) to EUR 2,900,906 (non-Hodgkin's lymphoma). The model was highly sensitive to mortality due to bacterial contamination (the higher, the more cost effective). In addition, increased platelet utilization decreased cost effectiveness, whereas elimination of the need for gamma irradiation and introducing an emergent HCV-like virus into the model increased cost effectiveness.
The Belgian evaluation by Moeremans et al. [26] compared the introduction of INTERCEPT™ pathogen reduction in addition to the current safety measures (i.e. nucleic acid testing, alkaline phosphatase testing, BactAlert testing and gamma irradiation) with the current safety measures alone. The model found a wide range of incremental cost-effectiveness ratios for INTERCEPT™ that were highly sensitive to the risk of emerging pathogen transmission and underlying disease. In the most conservative approach, in the absence of an emerging virus, the ratio ranged from EUR 628,541 per QALY (coronary artery bypass grafting) to EUR 5,142,697 per QALY (acute myelogenous leukaemia).
Postma and colleagues [25] estimated that net costs per life-year gained with INTERCEPT™ in addition to the standard procedures for platelet transfusion safety in the Netherlands (gamma irradiation, bacterial screening and viral screening) were EUR 719,232 for cardiology patients and EUR 1,029,685 for haematology patients. Sensitivity analysis revealed that cost effectiveness was insensitive to viral risks and indirect costing, but highly sensitive to the assumed excess transfusions required and discounting of life-years gained.
3.3.2 Platelet Preparation: Pathogen Testing/Culturing
Agapova and colleagues [15] evaluated the cost effectiveness of testing platelet donations for the parasite T. cruzi to reduce the risk of transfusion transmission of Chagas disease in US blood recipients. Compared with no testing, the incremental cost per QALY was EUR 446,153 per QALY in the hypothetical all-ages cohort.
In the analysis by Janssen and colleagues in the Netherlands [24], compared with a situation without bacterial culturing, the estimated incremental cost per QALY of introducing bacterial culturing was EUR 107,653. The probability of sepsis given bacterial contamination, the patients’ quality-adjusted life expectancy, the probability of death given sepsis, and the probability of bacterial contamination were the main parameters affecting cost effectiveness.
Bloch et al. [18] evaluated the costs and effects of implementing secondary bacterial testing of platelets in the US. The cost per averted transfusion of a positive culture was EUR 91,112.
3.3.3 Platelet Preparation: Apheresis Versus Whole Blood Platelets
Blumberg and Heal [19] and Lopez-Plaza et al. [21] evaluated the cost effectiveness of using single-donor apheresis platelets instead of pooled random-donor whole blood-derived platelets in the US. In Blumberg and Heal [19], the estimated cost per death prevented equalled EUR 25,156,317.
In Lopez-Plaza et al. [21], estimated costs per QALY varied from EUR 300,229 (non-Hodgkin's lymphoma) to EUR 925,106 (acute myelogenous leukaemia). The most influential parameters were the acquisition cost differential, the number of units in the pooled platelets equivalent to one apheresis platelet unit, the septic transfusion reaction risk from pooled platelets and the septic transfusion reaction-associated mortality rate.
3.3.4 Platelet Storage: Use of Platelet Additive Solutions (PAS)
In a US model, the use of platelets stored in PAS when patients experienced multiple mild allergic transfusion reactions to transfusion of leucoreduced single-donor apheresis platelets was cost saving for the entire range of costs for PAS storage evaluated (EUR 6–60) [20]. Using PAS from the start was only cost saving when these costs equalled EUR 6. Probabilistic sensitivity analysis revealed that cost savings associated with fewer allergic transfusion reactions when using PAS storage from the start persisted after considering uncertainty in the model input variables.
3.3.5 Combined Methods
Balducci et al. [16] evaluated the cost effectiveness of three strategies used to circumvent or prevent HLA alloimmunization in the US: (1) the use of unfiltered pooled platelets until alloimmunization and of crossmatch-compatible single-donor apheresis platelets thereafter; (2) the use of single-donor apheresis platelets from the beginning; and (3) the use of leucoreduced blood components (unclear if these were both pooled and single-donor platelets). In the model without allogeneic bone marrow transplantation, the modelled incremental cost of using pooled platelets compared with the leucoreduced blood components was EUR 98.79 per month of life. Compared with using leucoreduced blood components, use of single-donor platelets from the beginning had an incremental cost of EUR 163.71 per month of life. Monte Carlo sensitivity analysis with varying risk of refractoriness/alloimmunization, number of transfusions to refractoriness, number of transfusions to complete response, costs of single-donor platelets and filters, showed that there was at least a 75% chance that leucoreduced blood components are more cost effective than non-leucoreduced pooled platelets.
McFarland et al. [22] evaluated the costs and effects of the establishment and maintenance of a community donor plateletpheresis programme for transfusion of HLA-matched apheresis platelets in the US. Using actual programme costs, the cost-to-benefit ratio ranged from 1/1.39 to 1/2.14. When using an estimated minimum programme cost, the cost-to-benefit ratio was 1/1.58 to 1/2.42. In the sensitivity analysis, cost-to-benefit ratios remained favourable in all cases except when using the lower limit of the 95% confidence level of the estimated random-donor platelet units transfused in 1982, which yielded a ratio of 1/0.5.
3.4 Quality Appraisal
A full overview of the assessment of quality, applicability and conduct of the included studies using the Philips checklist is given in Online Resource 8 (see ESM). Appendix 1 contains narrative syntheses according to domain for each of the economic evaluations.
All of the evaluations clearly stated the decision problem and their objective, and all model-based evaluations chose an appropriate model type. The interventions and comparators (often standard practice strategies) under evaluation were clearly defined in 11 evaluations, and in eight of those, the time horizon was sufficient to reflect important differences between them. In four evaluations [16, 17, 28, 29], a clear definition of the strategies under evaluation was lacking, mainly due to poor description of the standard practice strategy. Seven evaluations did not include all the relevant interventions in the model [16,17,18, 25, 26, 29]. For example, Staginnus and Corash [29] did not consider the strategy of bacterial screening, although this is a very commonly used alternative for pathogen reduction. None of the evaluations transparently reported their data sources used to develop the model structure, which in itself was incomplete or outdated in eight evaluations [16, 17, 21, 23,24,25,26, 29]. Just two evaluations transparently reported and justified the structural assumptions used [16, 27]. Only three [15, 23, 25] addressed the four principal types of uncertainty (methodological, structural, parameter, heterogeneity). None of the evaluations showed evidence that the mathematical logic of the model was tested thoroughly before use. Just five evaluations [17, 23,24,25,26] compared their results with previous models or study findings.
4 Discussion
This systematic review identified 15 full economic evaluations that compared both the costs and consequences of different methods for preparation, storage and/or selection of allogeneic platelets intended for transfusion in adults. Eight of those investigated the cost effectiveness of pathogen reduction in different countries in Europe, North America and Asia. The incremental costs per QALY estimated in seven studies ranged from EUR 259,614 to EUR 36,688,323. In an eighth study, the cost per life-year gained for pathogen reduction was estimated at EUR 719,232 to EUR 1,029,685. For each of the other methods for platelet preparation, storage, selection and dosing, the evidence was sparse, due to a low number of full economic evaluations.
To the best of our knowledge, this is the first review to systematically search for, bundle and critically appraise full economic evaluations on this topic. We believe that our rigorous methodology is a major strength of this review. The comprehensive and systematic search in eight databases and grey literature websites ensures that this review provides a complete overview of the existing evidence to researchers, guideline developers, and/or decision makers in haematology and transfusion medicine.
Despite this strength, this review also has its limitations. For most of the methods used during preparation, storage and selection of platelets, less than a handful of full economic evaluations were found. The only exception was pathogen reduction, which was covered by eight studies. Nine of the 15 evaluations were published before 2010, making them outdated, further decreasing our confidence in the data. Moreover, the consistency of the models was not sufficiently assessed, which may result from a lack of data to support and/or validate the models. The low frequency of adverse events further increases the uncertainty of estimated outcomes. Furthermore, the generalisability of the incremental cost-effectiveness ratio (ICER) results to other countries may be limited due to possible differences in costs. Finally, from a methodological point of view, future GRADE guidance to assess the certainty of modelled evidence is required in order to critically appraise the model outputs directly.
The observed wide variation in ICERs for pathogen reduction (EUR 259,614 to EUR 36,688,323) probably stems from a combination of factors, including between-study differences in the comparators (not always clear due to lack of clear reporting), the populations, and explored scenarios (e.g. taking into account the emergence of new pathogens). Therefore, comparing ratios between studies for pathogen reduction is rather challenging. The fact that many evaluations presented ICERs in terms of QALYs gained, however, does allow for objective comparisons with other health interventions. Although the relevancy of using threshold values is still a matter of debate, the UK National Institute for Healthcare Excellence currently uses thresholds of GBP 20,000–30,000 per QALY gained [30], whereas the World Health Organisation promotes the threshold as three times the gross domestic product per capita as a guide to determine cost-effective healthcare interventions [31]. Applying any of these thresholds to our findings, in most cases, pathogen reduction cannot be considered cost effective, unlike bacterial culturing of platelets. The most likely reason for these very high ICERs of pathogen reduction is that the residual risk of transfusion-transmissible infections and other transfusion-related events is already quite low, because of the current standard strategies, for example thorough donor selection using medical questionnaires and routine screening for HIV, HCV, HBV and syphilis. However, cost-effectiveness ratios of other implemented blood safety measures also lie in the millions. Nucleic acid testing for HIV, HCV and HBV are estimated to cost USD 4,700,000–11,200,000 per QALY [32]. It has been suggested that transfusion safety measures should be evaluated using cost-effectiveness thresholds that are higher than those typically used by healthcare decision makers, reflecting the higher value placed on such types of interventions, where it is considered ‘unfair’ if patients have no access to the best possible protection [33]. In this light, implementation of pathogen reduction might be considered, nonetheless.
5 Conclusions
Based on the currently available economic evidence, the estimated incremental cost per QALY of pathogen reduction varies from EUR 259,614 to EUR 36,688,323. The cost effectiveness of other platelet preparation, storage, selection and dosing methods in platelet transfusion remains unclear due to insufficient and outdated evaluations. Future high-quality research is needed to expand the evidence base and increase our confidence in the findings, in order to facilitate informed decision making.
References
FDA. Bacterial Risk control strategies for blood collection establishments and transfusion services to enhance the safety and availability of platelets for transfusion—guidance for Industry2020 December 2020.
Saris A, Pavenski K. Human leukocyte antigen alloimmunization and alloimmune platelet refractoriness. Transfus Med Rev. 2020;34(4):250–7.
Kreuger AL, Caram-Deelder C, Jacobse J, Kerkhoffs JL, van der Bom JG, Middelburg RA. Effect of storage time of platelet products on clinical outcomes after transfusion: a systematic review and meta-analyses. Vox Sang. 2017;112(4):291–300.
van der Meer PF, de Korte D. Platelet additive solutions: a review of the latest developments and their clinical implications. Transfus Med Hemother. 2018;45(2):98–102.
Nahirniak S, Slichter SJ, Tanael S, Rebulla P, Pavenski K, Vassallo R, et al. Guidance on platelet transfusion for patients with hypoproliferative thrombocytopenia. Transfus Med Rev. 2015;29(1):3–13.
Shehata N, Tinmouth A, Naglie G, Freedman J, Wilson K. ABO-identical versus nonidentical platelet transfusion: a systematic review. Transfusion. 2009;49(11):2442–53.
Estcourt LJ, Stanworth S, Doree C, Trivella M, Hopewell S, Blanco P, et al. Different doses of prophylactic platelet transfusion for preventing bleeding in people with haematological disorders after myelosuppressive chemotherapy or stem cell transplantation. Cochrane Database Syst Rev. 2015;10:CD010984.
Estcourt LJ, Birchall J, Allard S, Bassey SJ, Hersey P, Kerr JP, et al. Guidelines for the use of platelet transfusions. Br J Haematol. 2017;176(3):365–94.
Kaufman RM, Djulbegovic B, Gernsheimer T, Kleinman S, Tinmouth AT, Capocelli KE, et al. Platelet transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2015;162(3):205–13.
Avau B, O D, Veys K, Georgsen J, Nahirniak S, Shehata N, et al. Systematic reviews on platelet transfusions—is there unnecessary duplication of effort? A scoping review. Vox Sanguinis [in revision]. 2022.
Grey matters: a practical tool for searching health-related grey literature [Internet]. Ottawa: CADTH; 2018. https://www.cadth.ca/grey-matters-practical-toolsearching-health-related-grey-literature. Accessed 8 May 2023.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. www.covidence.org. Accessed 8 May 2023.
Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess. 2004;8(36):iii–iv (ix-xi, 1-158).
Mandrik OL, Severens JLH, Bardach A, Ghabri S, Hamel C, Mathes T, et al. Critical appraisal of systematic reviews with costs and cost-effectiveness outcomes: an ISPOR Good Practices Task Force Report. Value Health. 2021;24(4):463–72.
Agapova M, Busch MP, Custer B. Cost-effectiveness of screening the US blood supply for Trypanosoma cruzi. Transfusion. 2010;50(10):2220–32.
Balducci L, Benson K, Lyman GH, Sanderson R, Fields K, Ballester OF, et al. Cost-effectiveness of white cell-reduction filters in treatment of adult acute myelogenous leukemia. Transfusion. 1993;33(8):665–70.
Bell CE, Botteman MF, Gao X, Weissfeld JL, Postma MJ, Pashos CL, et al. Cost-effectiveness of transfusion of platelet components prepared with pathogen inactivation treatment in the United States. Clin Ther. 2003;25(9):2464–86.
Bloch EM, Marshall CE, Boyd JS, Shifflett L, Tobian AAR, Gehrie EA, et al. Implementation of secondary bacterial culture testing of platelets to mitigate residual risk of septic transfusion reactions. Transfusion. 2018;58(7):1647–53.
Blumberg N, Heal JM. Mortality risks, costs, and decision making in transfusion medicine. Am J Clin Pathol. 2000;114(6):934–7.
Kacker S, Ness PM, Savage WJ, Frick KD, McCullough J, King KE, et al. The cost-effectiveness of platelet additive solution to prevent allergic transfusion reactions. Transfusion. 2013;53(11):2609–18.
Lopez-Plaza I, Weissfeld J, Triulzi DJ. The cost-effectiveness of reducing donor exposures with single-donor versus pooled random-donor platelets. Transfusion. 1999;39(9):925–32.
McFarland JG, Larson EB, Hillman RS, Slichter SJ. Cost-benefit analysis of a plateletapheresis program. Transfusion. 1986;26(1):91–7.
Custer B, Agapova M, Martinez RH. The cost-effectiveness of pathogen reduction technology as assessed using a multiple risk reduction model. Transfusion. 2010;50(11):2461–73.
Janssen MP, van der Poel CL, Buskens E, Bonneux L, Bonsel GJ, van Hout BA. Costs and benefits of bacterial culturing and pathogen reduction in the Netherlands. Transfusion. 2006;46(6):956–65.
Postma MJ, van Hulst M, De Wolf JT, Botteman M, Staginnus U. Cost-effectiveness of pathogen inactivation for platelet transfusions in the Netherlands. Transfus Med. 2005;15(5):379–87.
Moeremans K, Warie H, Annemans L. Assessment of the economic value of the INTERCEPT blood system in Belgium. Transfus Med. 2006;16(1):17–30.
Agapova M, Lachert E, Brojer E, Letowska M, Grabarczyk P, Custer B. Introducing pathogen reduction technology in Poland: a cost-utility analysis. Transfus Med Hemother. 2015;42(3):158–65.
SaBTO. Pathogen inactivation of platelets—Report of the SaBTO Working Group2014.
Staginnus U, Corash L. Economics of pathogen inactivation technology for platelet concentrates in Japan. Int J Hematol. 2004;80(4):317–24.
Appleby J, Devlin N, Parkin D. NICE’s cost effectiveness threshold. BMJ. 2007;335(7616):358–9.
Hutubessy R, Chisholm D, Edejer TT. Generalized cost-effectiveness analysis for national-level priority-setting in the health sector. Cost Eff Resour Alloc. 2003;1(1):8.
Jackson BR, Busch MP, Stramer SL, AuBuchon JP. The cost-effectiveness of NAT for HIV, HCV, and HBV in whole-blood donations. Transfusion. 2003;43(6):721–9.
Yeh JM, Botteman M, Pashos CL, Postma MJ, Staginnus U. Economics of transfusion. Infusion Therapy Transfus Med-Infusionstherapie und transfusionsmedizin. 2002;29(4):218–25.
Etchason J, Petz L, Keeler E, Calhoun L, Kleinman S, Snider C, Fink A, Brook R. The cost effectiveness of preoperative autologous blood donations. N Engl J Med. 1995;332(11):719–24.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work is supported in part by a grant from the European Blood Alliance (EBA) (grant 2021-01) and in part by structural support from the Foundation for Scientific Research of the Belgian Red Cross. The sponsors had no part in the design of this protocol. The contents of this document do not necessarily reflect the views and policies of the EBA, nor does mentioning of trade names or commercial products constitute endorsement or recommendation of use.
Conflicts of Interest
Relevant financial conflicts of interest directly related to this review: All authors declared not having any relevant direct financial conflict of interest. Relevant financial conflicts of interest not directly related to this review: JL, HVR, HS, BA, EDB, VC and PV are employees of Belgian Red Cross–Flanders, which is responsible for supplying adequate quantities of safe blood products to hospitals in Flanders and Brussels on a continuous basis and is funded by the Ministry of Social Affairs. Belgian Red Cross–Flanders received a grant from the European Blood Alliance to conduct this review. SS is an employee of NHS Blood and Transplant, which is the blood service supplier for England and manufactures platelets, and Chair International Collaboration for Transfusion Medicine Guidelines (ICTMG). SS reports research grant funding for trials using platelets and tranexamic acid. JG and SN declared not having any other financial conflicts of interest. NS received personal fees from the Canadian Blood Services for the International Collaboration for Transfusion Medicine Guidelines (ICTMG). SS received a grant award to conduct trials on use of platelets and tranexamic acid in patients with haematological cancer and a grant award to conduct trials on using platelets in neonates. Relevant intellectual conflicts of interest: JL, HVR, HS, BA, JG, EDB, VC and PV declared not having any intellectual conflict of interest. NS, SN and SS declare involvement in the ICTMG platelet guideline (SS is the chair, SN is the co-chair).
Data Availability
All (secondary) data generated or analysed during this study are included in this published article and its Online Resources.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent to publish
Not applicable.
Code Availability
Not applicable.
Author Contributions
JL: Conceptualization, Investigation, Formal analysis, Writing—Original draft, Visualization. HVR: Conceptualization, Investigation, Formal analysis, Writing—Review & Editing, Visualization, Supervision, Project administration, Funding acquisition. HS: Investigation, Formal analysis, Writing—Review & Editing, Visualization. BA: Conceptualization, Investigation, Writing—Review & Editing, Supervision, Project administration, Funding acquisition. JG: Validation, Writing—Review & Editing. SN: Validation, Writing—Review & Editing. NS: Validation, Writing—Review & Editing. SS: Validation, Writing—Review & Editing. EDB: Conceptualization, Writing—Review & Editing, Supervision. VC: Conceptualization, Writing—Review & Editing, Supervision. PV: Conceptualization, Resources, Writing—Review & Editing, Supervision.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix 1 Summary of the quality and applicability of the included studies, according to the elements of the Philips checklist
Appendix 1 Summary of the quality and applicability of the included studies, according to the elements of the Philips checklist
Study | Element | Assessment |
|---|---|---|
Agapova et al. (2010) [15] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | There is a clear statement of the problem and objective of the evaluation, i.e. to assess the efficiency of selective T. cruzi donor screening strategies to reduce the risk of transfusion-transmitted infection in US blood recipients. The primary decision maker is not reported The Markov model simulates T. cruzi identification in donated blood and transfusion-transmitted disease progression in two hypothetical cohorts of blood recipients. The cycle length is clearly stated (1 year), but no justification is offered. The model perspective (2007 US societal perspective), time horizon (lifetime) and scope are clearly stated and considered appropriate. As such, incremental cost per QALY is a relevantly chosen outcome The sources of the data used to develop the structure are not specified, the causal relationships are not justified and the structural assumptions are not transparent or justified. The options under evaluation are clearly defined, but it is not justified why the strategies are all compared to 'no testing' and to the preceding strategy |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | The model uses data from Blood Systems Inc. (effectiveness of each testing strategy and costs), the Healthcare Cost and Utilization Project, and a PubMed literature search. It is unlikely that the authors performed a systematic literature review, which limits our confidence in the data used in the model. Choices made in the case of multiple data sources are not reported. The quality of the data is not assessed appropriately The choice of baseline data is neither sufficiently described nor justified. Transition probabilities are calculated appropriately, and a half-cycle correction is applied to both the costs and effects. The use of Scandinavian annual mortality data merged with US life tables to estimate long-term mortality is not considered ideal (as health care provision and transfusion practices may differ between Scandinavian countries and the US), but deemed sufficiently appropriate given the probable lack of better data Alternative assumptions are explored using one-way, two-way and probabilistic sensitivity analyses. Costs incorporated are justified and references are provided. Discount rates applied are in accordance with the US Panel on Cost Effectiveness in Health and Medicine The utilities that are incorporated into the model are appropriate and referenced. No justification on the methods of derivation for the utility weights is provided Sufficient detail is provided for some, but certainly not all data incorporated into the model. No information is available on how the literature was searched or how experts/official sources were consulted All types of uncertainty are addressed | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency) and no comparison with previous models is made (external consistency) | |
Agapova et al. (2015) [27] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The objective of the evaluation, to estimate the cost-utility of plasma and platelet pathogen reduction technology as an addition to the current blood safety interventions, is clearly stated, and the objective is consistent with the clearly stated decision problem. The primary decision maker is specified as the Polish Ministry of Health A previously developed decision-analytic model assessing the cost-utility of pathogen reduction technology in Canada [23] was modified to reflect the situation in Poland, but no data sources are specified for these modifications. The perspective of the decision tree embedded within a Markov model is clearly stated (year 2014, Polish healthcare system), but the time horizon is not reported The structural assumptions of the model are clearly described and justified, and reasonable |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Costs of testing and of medical interventions to treat adverse events are stated to be partly modified from the Canadian model and updated to reflect Polish costs in 2013 PLN, but there is no transparency on how this was done. Other costs were obtained via personal communication with Terumo and with 2 doctors from the Institute of Haematology and Transfusion Medicine in Poland, but it is not clear how these sources were consulted. Post-transfusion and annual survival probabilities of Canada, Denmark and Sweden were reduced by 10% to adjust for a potential difference in healthcare quality and health outcomes in Poland, but no clear rationale for the 10% has been provided In accord with the recommendations of the US Panel on Cost-effectiveness in Health and Medicine, future costs and effects are discounted at 3% per year and were allowed to vary independently between 1% and 5% in sensitivity analysis. It is unclear if this is appropriate considering the Polish perspective The utilities incorporated into the model are considered appropriate, but the source for the utility weights is not reported and the methods of derivation are not justified Sufficient detail is provided for some, but certainly not all data incorporated into the model. No information is available on how the literature was searched or how experts/official sources were consulted Methodological, structural and parameter uncertainty have been addressed appropriately. In contrast, heterogeneity is not taken into account | |
Consistency Internal consistency External consistency | There is no evidence that extensive sensitivity analyses have been conducted or that the model has been tested mathematically. The authors state that they were not aware of any existing economic evaluations of blood safety interventions in Poland. Hence, assessing external consistency was not possible | |
Balducci et al. (1993) [16] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The objective of this evaluation, to investigate the cost effectiveness of three transfusion strategies (filtered blood components, unfiltered pooled platelets, single-donor platelets) in the treatment of adult acute myelogenous leukaemia, is clearly stated. The perspective of the model and the primary decision maker are not. Although a Markov model would have been better, the decision-tree seems appropriate, because it covers the relatively short-term impact of the transfusions on mortality (long-term follow-up is not required) and there are discrete paths (e.g. dead/cured). The 5-year time horizon is considered sufficient. The authors report data sources related to the model parameters, but not related to the model structure. The structural assumptions are transparently reported and justified. It is unclear if they are reasonable, as there is insufficient information available on the perspective and the scope of the model. The model does not consider bacterial infections, febrile reactions and bleeding events. Furthermore, PAS is not considered as an alternative option, and it is unclear if the filtered platelets refer to both pooled and single-donor platelets or not. Also, the association with acute myelogenous leukaemia progression is questionable. Overall, our confidence in the structure of the model is low. |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Data on costs and effects came from English language articles, a doctor from the H. Lee Moffitt Cancer Center and the Southwest Florida Blood Bank. No further information (e.g. search strategy, method of collection of expert opinion) is provided. No internal or external quality assessment of the data is performed, which further limits the confidence in the data As the outcome is survival, no utilities were incorporated into the model Monte Carlo sensitivity analysis of 500 samples is performed to address structural uncertainties. Parameter uncertainty and methodological uncertainty have not been addressed. The authors developed two models, i.e. one with and one without the option of bone marrow transplantation, as only a limited number of patients are eligible for transplantation because of age, type of leukaemia, and financial constraints, and only a portion of eligible patients eventually undergo the procedure. Within the models themselves, heterogeneity has not been dealt with | |
Consistency Internal consistency External consistency | Although certain parameters are varied extensively in the Monte Carlo sensitivity analysis, these parameters are only relevant when transfusions are performed due to low platelet increments, and complete internal consistency is therefore not adequately assessed. No comparison with previous models is made (external consistency) | |
Bell et al. (2003) [17] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | This objective, i.e. to assess the economic costs and clinical outcomes associated with the use of the INTERCEPT™ Blood System for apheresis platelets and random-donor pooled platelet concentrations in the United States in patient populations in which platelets are commonly transfused, is clearly stated. The perspective and the primary decision maker are not reported The model expands on that of Lopez-Plaza 1999 (see below) and uses a decision tree for short-term outcomes, followed by a Markov model for long-term survival, which is deemed appropriate. Assumptions made are reported transparently, but for some, justification is lacking The model does not consider platelet refractoriness and adverse events of the pathogen reduction technology itself (i.e. effects caused by the chemicals, and the need for increased platelet use). Also, it does not contain all relevant transfusion-transmissible infections (e.g. CMV, WNV). Use of pooled platelets are not considered as a treatment option. In addition, the standard of care safety measures are only inexplicitly mentioned in the paper The time horizon is not explicitly stated, but can be assumed to be lifetime The pathways no longer reflect the underlying biological process of the disease, as it assumes that HIV leads to AIDS in all patients, which may have been the case in 2003 |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Data for important parameters were identified from the literature (PubMed search) and data on file at Baxter Healthcare corporation and Cerus Corporation. Data sources are reported throughout the paper. However, no systematic review has been conducted Choices made in the case of multiple data sources are not adequately reported. The quality of the data is not assessed appropriately. The choice of baseline data is described, but no justification is provided. The methods used to calculate excess mortality and QALY weights are described and considered appropriate Projected economic costs and health benefits in future years were discounted at 3% per annum, consistent with practice at that time in the US, but were not varied to address methodological uncertainty Structural uncertainty was addressed through an alternative baseline scenario and through probabilistic sensitivity analysis. Heterogeneity and parameter uncertainty were assessed appropriately | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency). The authors report that their ICERs are comparable to previously reported cost-effectiveness findings of accepted blood safety interventions, with reference to previous modelling studies about pathogen inactivation | |
Bloch et al. (2018) [18] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | This study wanted to find out if secondary bacterial culturing could contend with residual risk of bacterial contamination. In accordance with its hospital perspective, costs associated with secondary bacterial culturing and the number of transfusions were included. The outcome, averted transfusion of a positive culture, reflects the perspective and scope of the model, and is consistent with the objective of the evaluation. Additional investigation at the blood collection agency was not considered nor was disposal of any co-components at the collecting facility. In addition, the in-hospital follow-up might be insufficient to capture all transfusion-related adverse events (with impact on quality of life and quality-adjusted life-years) This study did not use a model |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | The effect data and the sources of the cost data are clearly described. It is, however, unclear how the cost per averted transfusion of a positive culture is calculated on the basis of the cost data. Heterogeneity and parameter uncertainty are not taken into account | |
Consistency Internal consistency External consistency | The results of this study were not compared with those of previous models or studies | |
Blumberg and Heal (2000) [19] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The objective of the evaluation, to compare the efficacy and costs of using single-donor apheresis platelets instead of pooled random whole blood-derived platelets, is clearly stated. The primary decision maker is not mentioned. The in-hospital follow-up might be insufficient to capture all transfusion-related deaths due to HIV, HBV or HCV infection. This study did not use a decision tree or Markov model |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | The risks of fatality due to HIV-1, HBV and HCV infection were calculated from hospital data or estimated from recent national studies. It is unclear why the risk of bacterial contamination and CMV infection were not considered. Extrapolation from TTI risk to fatality rate was documented and justified. Cost data were probably provided by the Strong Memorial Hospital, although this was not clear. Heterogeneity was not dealt with and parameter uncertainty was not taken into account | |
Consistency Internal consistency External consistency | The results of this study were not compared with those of previous models or studies | |
Custer et al. (2010) [23] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The authors clearly state that they developed a new health economics model to assess the cost effectiveness of riboflavin-based pathogen reduction technology in mitigating the risk of transfusion-associated infectious and some noninfectious threats, from a Canadian health care system perspective and using a lifetime horizon. The model has a decision analytic format and is a cohort simulation with separate disease-specific Markov submodels to track the progression of each adverse event. The general structure of the model is not supported by references to data sources. However, assumptions and estimations of important parameters in the model (e.g. % of immunocompromised patients) come with references, but no real justifications. The model does not consider platelet refractoriness and does not account for multiple transfusions |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Data sources for disease occurrence, outcomes, and costs come from published literature specific to Canada, but there is no full transparency with regards to the literature search. When data were not available for a specific disease or condition, the authors used data from other countries with preference for US data when available, which is appropriate. They also clearly describe for some, but not all parameters, that when several data sources were available, data were combined No formal quality assessment was performed, but the limitations with regards to the uncertainty on the data are discussed in the Discussion section. The methods and assumptions used to extrapolate short-term results for adverse effects and overall mortality are documented and justified, but no transparency or justification is offered regarding quality of life In accord with the recommendations of the US Panel on Cost Effectiveness in Health and Medicine, future costs and effects are discounted at 3% per year and were allowed to vary independently between 1% and 5% in sensitivity analysis, thereby accounting for methodological uncertainty. Heterogeneity, parameter uncertainty and structural uncertainty are addressed appropriately as well | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency). Findings are compared with other evaluations included in this review [24,25,26, 29] | |
Janssen et al. (2006) [24] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The decision problem and the objective of the evaluation are clear. The primary decision maker, the Dutch Health Authorities, is specified. Although this is explicitly mentioned, one can assume that the model uses a healthcare perspective The sources of data used to develop the decision tree structure are not specified. The model does not take into account possible adverse effects of pathogen reduction technology itself (i.e. effects caused by the chemicals, and the need for increased platelet use). Also, it does not contain all relevant transfusion-transmissible infections (e.g. CMV, WNV). Not all, but most of the structural assumptions are transparent and justified. The lifetime horizon is appropriate |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Model parameters were obtained from the literature and from Dutch Sanquin blood banks. Data sources are reported throughout the article, but no systematic review has been conducted (at least not mentioned) and the data identification method is not transparent. Where choices were made between data sources, these were justified. No formal quality assessment was performed, but limitations with regards to the uncertainty of the data are discussed. The methods and assumptions used to extrapolate short-term results to final outcomes are documented and justified Future costs and effects are discounted at 4% "in accordance with guidelines for cost-effectiveness analyses", but no justification is provided on why this would be an appropriate rate for this model. The utilities that are incorporated into the model are appropriate and referenced. A justification on the methods of derivation for the utility weights is not fully provided Methodological uncertainty and heterogeneity are not dealt with. In contrast, structural and parameter uncertainty are addressed appropriately | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency). Findings are compared to the evaluation of Bell et al. 2003 [17], and are well in line with this model. | |
Kacker et al. (2013) [20] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The objective of this model, i.e. to compare expected health and financial outcomes between potential strategies of preventing mild and severe allergic transfusion reactions resulting from apheresis platelet transfusions, is clearly stated. The primary decision maker is not specified. A clear description of the scope (perspective, technologies involved, population and setting) is given. The outcome, i.e. cost per averted allergic transfusion reaction, is consistent with the hospital perspective, the scope and the overall objective of the model The sources of data used to develop the Markov-based decision tree are not specified. The structural assumptions are transparent, but not justified. The 1-year time horizon is considered appropriate, as there are no long-term effects of an allergic transfusion reaction |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Data were drawn from previous published literature, but there is no transparency regarding the search. Choices made in the case of multiple data sources are not reported. No formal quality assessment was performed, but limitations with regards to the uncertainty of the data are discussed in the Discussion section The choice of baseline data is described and justified. No information is available on how transition probabilities were calculated. A half-cycle correction is not reported. Costs incorporated are justified and sources are described. Discount rates are not reported The process of data incorporation is transparent. Distributions for each parameter are described, but not justified Structural and parameter uncertainty are addressed appropriately, but methodological uncertainty and heterogeneity are not | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency) and no comparison with previous models is made (external consistency) | |
Lopez-Plaza et al. (1999) [21] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The objective of this model is clearly reported: to calculate the incremental health benefits (QALY), direct costs and medical cost savings associated with single-donor platelet transfusion therapy relative to those associated with random donor platelet transfusion therapy. The primary decision maker and the perspective of the model are not specified The sources of the data used to develop the model structure are not reported. The model does not consider all transfusion-transmissible infections and does not take into account the other adverse effects of the single- and random-donor platelets themselves. The structural assumptions are transparently reported, but not justified. Given the lack of disease state transitions, a decision tree model is considered appropriate for this analysis. The lifetime horizon is appropriate |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Data for the important parameters were identified from the literature, but probably no systematic review was conducted. The cost data seem relevant given the objective, but the data identification methods are unclear. No internal or external quality assessment of the data is performed The estimates assigned to the baseline model were those for a 40-year-old female for the HPCT population and those for a 70-year-old male and female for the CABG population. It is unclear why these were chosen. The methods and assumptions used to extrapolate short-term results to final outcomes have been documented and justified Some, but not all, cost data were justified and referenced adequately. For the lifetime direct medical costs for treating viral complications of transfusion therapy, it is stated that discount rates have been obtained from published sources, but no further information is provided The source for the utility weights is referenced, but the methods of derivation are not reported. Sufficient data is provided for some, but certainly not all parameter data The process of data incorporation is transparent Methodological uncertainty was not addressed. In contrast, heterogeneity, structural and parameter uncertainty are taken into account | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency). The findings of the model are compared with another model [34], but in a very superficial way | |
McFarland et al. (1986) [22] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The objective of the evaluation, to perform a cost-benefit analysis of establishing and maintaining an HLA-typed donor pool, is clearly stated. The primary decision maker is not specified. The evaluation did not take into consideration the costs and the benefits from the perspective of the patients' families and the individual volunteer platelet-apheresis donors, and used the net cost of platelets saved as an outcome, which is consistent with the blood centre perspective The 5-year and 10-year economic life projections of the programme are considered appropriate This study did not use a decision tree or Markov model, but employed mathematical linear/exponential regression modelling |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | The choice of baseline data was described, but not justified. Because the programme life was expected to be at least 5 years, the costs per patient for 1 year of support observed in the study were discounted at 6% per year for the 5-year minimum life of the programme, expressed as 1982 present-value costs. In the sensitivity analysis, estimates of HLA-typing fees, donor coordinator salary, apheresis charges, discount rates, programme life, random donor and platelet apheresis fees, and numbers of platelet units transfused were varied within the 95% confidence limits of the projections. Discount rates used in the present value analysis were varied (3, 6, and 12% rates), and programme life estimates were made for 1, 5 and 10 years Heterogeneity was not dealt with | |
Consistency Internal consistency External consistency | The results of this study were not compared with those of previous models or studies | |
Moeremans et al. (2006) [26] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The objective of the evaluation is clearly stated, i.e. to analyse the health and economic consequences of pathogen inactivation using the INTERCEPT™ Blood System in Belgium, taking a perspective directed to the future, including the risk of emergence of a new transfusion-transmissible virus. The primary decision maker is not specified This cost-utility analysis was performed from a societal perspective, and therefore rightfully considered short-term and long-term direct medical costs, productivity-related costs, as well as legal and liability costs The sources of data used to develop the decision tree structure are not specified. The model does not account for CMV infection and increased platelet use Structural assumptions made are transparent. However, no justification is provided for the two main assumptions, i.e. pathogen inactivation is 100% effective and is not associated with major or costly adverse events. The assumption that pathogen inactivation is 100% effective is questionable. Bacterial testing is not included as a feasible option, although it is a very common alternative. No comparison is made between apheresis and random-donor platelets The decision tree model is appropriate, but does not allow to model the timepoint at which the new transfusion-transmissible virus arises The time horizon is not reported, but probably is lifetime, which is appropriate |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Model parameters were obtained from the literature, the Belgian Red Cross and clinical experts. Data sources are reported throughout the article, but no systematic review has been conducted (at least not mentioned) and no information on how experts and official sources were consulted is provided. Where more than one data source is mentioned, it is unclear how these data were synthesized (e.g. average cumulative mortality rate of CML patients, probability of developing chronic hepatitis for HCV and HBV). References for transition probabilities are provided, but it is unclear how these data sources were selected. No formal quality assessment was performed, and limitations with regards to the uncertainty of the data are not discussed either Discount rates have not been described, or justified It is unclear if the utilities that are incorporated into the model are appropriate. Utility weights for HIV and hepatitis are given, but no data sources are provided and it is unclear which country these data apply to. Methodological uncertainty and parameter uncertainty are not dealt with. In contrast, heterogeneity was taken into account by offering separate results for different patient populations. Structural uncertainties have been addressed appropriately via the use of multiple scenarios rather than sensitivity analyses | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency). Findings are compared with the evaluations of Bell et al. 2003 [17] and Postma et al. 2005 [25], and are well in line with these models | |
Postma et al. (2005) [25] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The decision problem and the objective of the evaluation, i.e. to estimate cost effectiveness of pathogen inactivation for platelet transfusions in the Netherlands, are clear. The primary decision maker is not specified. The inclusion of indirect costs into the model, and the outcomes used (treatment and care of transfusion-related viral and bacterial infections and averted deaths due to infections), are consistent with its societal perspective It is clearly stated that the scope is limited to elimination of risks for known bacterial and viral infections and improvements in blood bank processing with regard to elimination of gamma irradiation. The sources of data used to develop the decision tree and Markov model structure are not specified. The model does not consider platelet refractoriness. Furthermore, it does not contain all the relevant transfusion-transmissible infections (e.g. CMV) All structural assumptions are transparent, but not all of them are justified. The assumption that pathogen inactivation is 100% effective is questionable. The lifetime horizon is appropriate |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Data for the important parameters were identified from official sources (e.g. Dutch Central Bureau of Statistics), experts ["We acknowledge the input of W Hoogen Stoevenbeld (Prismant Health Care, Utrecht) for promptly providing additional data on the risk of transfusion-related sepsis"] and the literature (no systematic literature search reported). The authors do not provide information on how experts were consulted, nor do they justify the use of expert opinion in addition to or over literature data, e.g. for the risk of transfusion-related sepsis No formal quality assessment is performed. Limitations with regards to the uncertainty of the data are briefly mentioned in the Discussion section The use of indirect costs is justified, but their calculation is not (and even not reported). No justification is provided for assuming 10% elimination of gamma irradiation at €30 per irradiation. According to the Dutch guidelines for pharmacoeconomic research, future costs (and LYG) were discounted at 4% per annum The annual number of transfusion-related sepsis cases was incorporated as a Poisson distribution, but this was not justified The four principal types of uncertainty have been addressed appropriately | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency). The findings of the model are put into perspective with those of Bell et al. 2003 [17] | |
SaBTO (2014) [28] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The aim of this evaluation is to determine whether the introduction of pathogen inactivation of platelets is an appropriate risk reduction measure to be introduced by the UK Blood Services. Although the primary decision maker is not specified, the SaBTO advises the UK National Health Service Part of this evaluation consisted of determining the cost effectiveness of different pathogen inactivation systems. It is unclear if the model looks at the implementation of pathogen inactivation in addition to the current safety measures. Furthermore, these standard-of-care measures are only inexplicitly mentioned in the report. The technologies of pathogen inactivation are clearly stated and justification is provided. It is clearly stated that the modelling is restricted to the impact on bacterial infection, but no justification is provided. No information is provided on the model structure, perspective or time horizon The structural assumptions are transparent, but for the majority not justified |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | The authors state that "the findings of SaBTO’s review are based on the information and evidence available at the time". A Cochrane systematic review was conducted on pathogen inactivation, but it is by no means clear if and how data from this review were used in the cost-effectiveness analysis It is clear that in addition to literature, expert opinion has been used (e.g. manufacturers), but the methods used to decide which experts and the ways they have been consulted have not been described (nor justified) Only data on the cost of platelet production, the cost of screening and pathogen inactivation, the cost of treatment of infections and the number of life-years lost, and the equity cost are sufficiently described and referenced. Other data (probabilities of contamination, effectiveness of interventions etc.) are not described nor justified Discounting is performed, but the rates are not described nor justified Methodological uncertainties are not addressed and heterogeneity is not dealt with. Structural uncertainties are addressed using sensitivity analyses with regards to the infectivity of variant Creutzfeldt Jakob Disease and the effectiveness of pathogen inactivation. Parameter uncertainty is assessed appropriately using one-way sensitivity analysis | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency) and no comparison with previous models is made (external consistency) | |
Staginnus and Corash (2004) [29] | Structure Statement of decision problem/objective Statement of scope/perspective Rationale for structure Structural assumptions Strategies/comparators Model type Time horizon Disease states Cycle length | The authors clearly state that they developed a literature-based decision-analytic model to assess the economic costs and clinical outcomes associated with the introduction of single-donor apheresis platelets treated with the INTERCEPT™ Blood System in Japan, thereby facilitating the decision-making process for implementing a novel blood safety technology The primary decision maker is not specified, but is probably the Japanese healthcare system. The perspective and the time horizon of the model are not stated clearly The authors say that their decision tree analysis was based on a previous model by Bell et al. 2003 [17], which in its turn refers to Lopez-Plaza et al. 1999 [21], but no further information is given. The model does not consider platelet refractoriness and possible adverse effects of pathogen reduction technology (i.e. caused by the chemicals, need for increased platelet use) For some structural assumptions, no justification is provided Bacterial screening is not considered as one of the feasible treatment options, although this is a very common alternative for pathogen reduction. In addition, the standard of care safety measures are only inexplicitly mentioned in the paper The decision tree model is appropriate, but does not allow to model the timepoint at which the new transfusion-transmissible virus arises The pathways no longer reflect the underlying biological process of the disease, as it assumes that HIV leads to AIDS in all patients, which may have been the case in 2004 |
Data Data identification Data modelling Baseline data Treatment effects Costs Quality-of-life weight (utilities) Data incorporation Assessment of uncertainty Methodological Structural Heterogeneity Parameter | Data are derived from literature and official sources (e.g. Japanese Red Cross). However, no systematic review has been conducted (at least not mentioned). Rightfully so, whenever available, data for Japan were used. Only if these were not available, European or US data were used, as blood transfusion safety practices are very similar among developed countries and only small differences in the data could be expected. Where multiple data sources are mentioned, it is unclear how these were synthesized or if choices were made between them A questionnaire was designed to capture the current Japan Red Cross blood banking procedures and their associated unit costs to evaluate the impact of INTERCEPT™ platelets on the blood banking “value chain”. No other information was provided on how the experts were chosen or consulted. No formal quality assessment is performed, and limitations with regards to the uncertainty on the data are not discussed either Costs incorporated into the model were justified and referenced appropriately. Economic costs and health benefits incurred in future years were discounted at 3% per annum, consistent with current practice Japanese life tables from official population statistics were applied to calculate life-years gained, according to the declining exponential approximation of life expectancy method with consideration of competing mortality from disease-specific and naturally occurring causes Methodological uncertainties are not addressed. In contrast, structural uncertainties were addressed using various scenarios with varying rates of bacterial fatality and risks of emerging pathogens. Heterogeneity was dealt with by providing separate results for different patient groups. Parameter uncertainty was assessed via one-way sensitivity analysis, but the ranges used were not justified. | |
Consistency Internal consistency External consistency | No information is reported on whether the model was tested thoroughly before use (internal consistency) and no comparison with previous models is made (external consistency) |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Laermans, J., Van Remoortel, H., Scheers, H. et al. Cost Effectiveness of Different Platelet Preparation, Storage, Selection and Dosing Methods in Platelet Transfusion: A Systematic Review. PharmacoEconomics Open 7, 679–708 (2023). https://doi.org/10.1007/s41669-023-00427-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-023-00427-w