Abstract
The curative potential of allogeneic hematopoietic cell transplantation (allo-HCT) for acute myeloid leukemia (AML) relies on the graft-versus-leukemia (GVL)-effect. Relapse after allo-HCT occurs in a considerable proportion of patients, and has a dismal prognosis with very limited curative potential, especially for patients with FLT-ITD-mutated AML. Since the first description of sorafenib for treatment of FLT3-ITD-mutated AML, several clinical trials have tried to determine the efficacy of FLT3 inhibitors for preventing and treating AML relapse after allo-HSCT, but many questions regarding differences among compounds and mechanisms of action remain unanswered. This review provides an overview on the established and evolving use of FLT3 inhibitors to prevent or treat relapse of AML in the context of allo-HCT, focusing on the recently discovered immunogenic potential of some FLT3 inhibitors and addressing the possible mechanisms of leukemia drug-escape.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) harboring an activating mutation in FLT3 represents around one third of AML cases and is characterized by high relapse rate and dismal prognosis despite undergoing allogeneic hematopoietic cell transplantation (allo-HCT) [1, 2].
FLT3 is a transmembrane receptor tyrosine kinase physiologically expressed by hematopoietic stem and progenitor cells. The most common mutation is an internal tandem duplication (ITD) within the juxtamembrane domain, which constitutively activates the receptor, promoting proliferation and cell survival mainly through the activation of the PI3K, MAPK (ERK) and STAT5 signaling pathways (Fig. 1). The second type of mutation is a single amino acidic exchange in the tyrosine kinase domain (TKD), resulting in the loss of auto-inhibitory function [3,4,5,6,7].
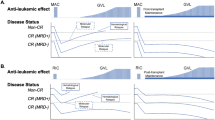
Mechanism of action of type I and type II FLT3 inhibitors and downstream effects. Proposed mechanism through which sorafenib/gilteritinib leads to increased IL-15 transcription. Inhibition of FLT3 receptor tyrosine kinase signaling reduces ATF4 production. Reduced ATF4 levels result in less inhibition of IRF7 phosphorylation and activation. Active p-IRF7 can translocate to the nucleus, where it activates IL-15 transcription. IL-15 activates CD8 T cells and NK cells.
Mutations within FLT3 occur late in leukemogenesis, are strong driver mutations and have been identified as a druggable target in FLT3-mutated AML [8, 9]. Efforts to establish FLT3 tyrosine kinase inhibitors (TKI) as treatment options are now spanning over two decades and did not yield lasting clinical benefits as monotherapy at first [10,11,12]. It was only recently that the multi-kinase inhibitor midostaurin in combination with chemotherapy and giltieritinib as monotherapy demonstrated clinical benefit in newly diagnosed FLT3-mutated AML and in relapsed/refractory disease respectively, leading to their FDA and EMA approval [13, 14].
FLT3 inhibitors are classically divided in first-generation multi-target inhibitors (such as midostaruin, sunitinib and sorafenib) and next-generation selective inhibitors (such as quizartinib, crenolanib and gilteritinib). Furthermore, inhibitors can be classified based on the ability to bind to the active conformation of the receptor (type I inhibitors, such as midostaurin, crenolanib, gilteritinib, sunitinib), which are functional against FLT3-ITD and TKD-mutated forms or to bind only the inactive or ITD-mutated conformation of the target (type II inhibitors, such as sorafenib, quizartinib), which are therefore intrinsically inert toward TKD-mutated receptors [15]. Since one major mechanism of resistance to type II inhibitors is the acquisition of additional FLT3 TKD mutations, the use of type I inhibitors is currently favored by clinicians [16,17,18,19]. Interestingly, some durable remissions were observed in patients with FLT3-ITD-mutated AML treated with sorafenib after allo-HCT. Further analysis on this synergism leads to the discovery of the immuno-stimulatory effect of several FLT3 tyrosine kinase inhibitors (FLT3-TKIs), such as sorafenib, tandutinib, midostaurin, crenolanib, quizartinib, through induction of IL15-production in the AML cells (Fig. 1) [20]. The connection between FLT3 inhibition and IL-15 production in the GVL context was reproduced by the group of Teshima using gilteritinib [21].
This review provides an overview on the established and evolving potential use of FLT3 inhibitors to prevent or treat AML relapse in post-transplantation context and addresses pending questions regarding its immunogenicity and the mechanisms of leukemia relapse during or after treatment.
Treatment of overt relapse
Relapse incidence is highest within the first 2 years after allo-HCT and survival is better if incipient relapse is detected earlier. Therefore, regular monitoring for MRD markers including chimerism is recommended [22, 23]. In overt AML relapse, the reduction of immunosuppression can result in response and even complete remission. Several other strategies exist to “actively” treat AML relapse after allo-HCT. Data on comparison of different strategies for treatment of overt relapse are sparse, but in the last decade, several retrospective studies and clinical trials compared treatment with FLT3-TKI monotherapy with standard chemotherapy, unfortunately none of them focusing on relapse after allo-HCT. A list of the phase II and III clinical trials on FLT3-TKI monotherapy in the context of relapse/refractory leukemia can be found in Table 1.
Sorafenib
Sorafenib, a first-generation multi-target kinase inhibitor approved for treatment of advanced renal and hepatic cell carcinoma, has been studied since more than a decade in FLT3-ITD-mutated AML patients. First results of small retrospective studies and case series of sorafenib monotherapy in relapse/refractory AML were controversial [24,25,26]. Metzelder and colleagues reported a composite complete response (CRc) rate of 38% in 65 patients with FLT3-ITD AML refractory to multiple therapy lines, with even more striking effects in patients relapsing after allo-HCT compared to relapse after chemotherapy only [27]. In a retrospective cohort of 29 FLT3-ITD-positive AML patients, who relapsed after allo-HCT, 6 patients (21%) achieved sustained CR with sorafenib monotherapy [28]. Excluding one patient who received a second allo-HCT, four of these patients are in treatment-free remission for a median of 4.4 years. With a median follow-up after relapse of 7.5 years, these data suggest for the first time that FLT3-ITD inhibition alone can induce long-term disease control and conditional cure in patients relapsing after allo-HCT [28]. These results were confirmed by further case series and retrospective studies in patients with FLT3-ITD AML relapse post allo-HCT, who showed impressive responses to sorafenib in individual patients including long-term survival [27, 29,30,31].
As donor lymphocyte infusions (DLI) and hypomethylating agents are widely used for the treatment of post-transplant AML relapse, some patients received sorafenib in combination with DLI or azacytidine [32]. Treatment of FLT3-ITD-mutated AML relapse post-allo-HCT with sorafenib and DLI was superior to DLI alone and to combination of chemotherapy and DLI in a retrospective analysis [20]. More recently, the triple combination of sorafenib chemotherapy and DLI was shown to be superior in terms of response rate and overall survival compared to the combination of sorafenib and chemotherapy or chemotherapy and DLI (CR 70.7% with triple combination, 50.0% with sorafenib + chemotherapy and 35.3% chemotherapy + DLI, p = 0.007) (1 year OS 53.2% with triple combination, 25.0% with sorafenib + chemotherapy and 23.5% chemotherapy + DLI, p = 0.003) [33]. Interestingly, the combination of sorafenib and DLI did not show a significant increase in incidence of acute and chronic GvHD [33]. Despite the promising data derived from retrospective analysis on the use of sorafenib combined with DLI for hematological relapse of FLT3-ITD AML post-allo-HCT, there is no prospective trial that would justify this approach in all patients and prevention of relapse rather than treatment would be desirable.
Quizartinib
As first on the market next-generation potent FLT3-inhibitor [34], quizartinib was intensively studied in relapse/refractory AML. After determination of feasibility and maximal tolerated dose in two phase I trial, including a total of 16 patients after allo-HCT [35, 36], three phase II trial with different dosages were conducted (Table 1). In all phase II trial, a consistent composite complete response in 47–56% of patients was observed and a median overall survival (OS) of 21–34 weeks was reached. These clinically relevant results were confirmed by a large multicentre randomized controlled phase III clinical trial (QuANTUM-R) on 367 patients. Relapse/refractory patients treated with quizartinib monotherapy showed a higher CRc rate (48% vs 27%) and a higher OS (median 6.2 months vs 4.7 months) compared to salvage chemotherapy group [37]. Unfortunately, even though 61 and 28 patients relapsing after allo-HCT were included in quizartinib and chemotherapy group respectively, no subgroup analysis was conducted and a previous allo-HCT did not show a significant benefit for the treatment with quizartinib. Another main downside of this study is the exclusion of patients previously exposed to FLT3-TKI. Since the introduction of midostaurin as standard of care induction therapy in FLT3-ITD mutant AML, such a TKI-free FLT3-ITD-mutated AML population is not representing the real-world population. Quizartinib was approved in Japan in 2019 for the treatment of relapsed/refractory AML based upon promising initial results. In the same period, though, the FDA rejected approval for quizartinib because of major doubt about the limited survival benefit shown in the QuANTUM-R trial.
Gilteritinb
The highly selective type I next-generation FLT3-inhibitor gilteritinib was analyzed in a phase I–II trial in seven dose escalation cohorts of relapse/refractory AML and showed favorable safety profile and consistent FLT3 inhibition in most patients receiving a daily dose of 80 mg or higher [38]. Based on the promising CRc rates of 41% of FLT3-ITD-mutated AML patients receiving at least 80 mg/day, gilteritinib in the dose of 120 mg/day was compared to salvage chemotherapy in a randomized controlled phase III clinical trial (ADMIRAL) including 371 FLT3-mutated relapse/refractory AML patients [14]. Gilteritinib monotherapy resulted in a significantly higher composite complete remission rate compared to salvage chemotherapy (54.3% vs 21.8%, HR 32.5, 95% CI 22.3–42.6), higher overall survival (median 9.3 months vs 5.6 months, p < 0.001) and event-free survival (median 2.8 months vs 0.7 months, HR 0.79, 95% CI 0.58–1.09). Compared to other inhibitors, gilteritinib had a better safety profile as severe adverse events occurred less frequently in the gilteritinib group compared to the salvage therapy group. Seventy-four patients included in the study underwent gilteritinib regimen for relapse after allo-HCT and, interestingly, relapse in the first 6 months after allo-HCT was associated with a high benefit from gilteritinib therapy compared to salvage chemotherapy (HR for death 0.38, 95% CI 0.20–0.75). Based upon these results, gilteritinib was approved by the FDA for relapsed/refractory AML in 2018. These findings were confirmed in the Japanese subpopulation in an open-label phase I trial [39], and in a recent subgroup analysis of the ADMIRAL trial [40]. Of note, also in the ADMIRAL trial, patients who previously received FLT3-TKI represent only 12.4%, making it difficult to apply to the current population receiving midostaurin as standard treatment.
Based on the high response rates, gilteritinib may be the most promising FLT3-TKI and ongoing trials are testing gilteritinib in combination with venetoclax and hypomethylating agents in relapsed/refractory AML (NCT03404193, NCT03404193). The role of TKI in post-allo-HCT setting is not tested here as the number of patients with post-transplantation relapse is usually very low in these studies: Maiti and colleagues included only 4 transplanted patients in their phase II trial on triple combination therapy with gilteritinib–venetoclax–decitabine, but obtained a promising CRc of 62% in relapse/refractory patients [41].
Midostaurin
Despite the defined role of midostaurin in first-line therapy of FLT3-ITD-mutated AML [13], this first-generation kinase inhibitor has not been intensively studied as salvage therapy in the context of post-transplant relapse.
Maintenance therapy
Based on the promising results in relapse/refractory AML, treatment with FLT3-TKI was tested as maintenance therapy in clinical trials to elucidate its potential in preventing the occurrence of relapse after allo-HCT. Phase II–III trial on maintenance treatment after allo-HCT are listed in Table 2.
Midostaurin
Induction therapy and maintenance with Midostaurin in FLT3-ITD-mutated AML had shown a very low relapse rate [42, 43], though, clinical data on maintenance after allo-HCT are very few. A recent phase II randomized open-label trial including 60 patients, included patients in CR1 after allo-HCT that were then randomized to receive maintenance with midostaurin or not. The study demonstrated safety and feasibility when midostaurin was given for 12 months after allo-HCT. Grade 3 adverse event occurred in not more than 10% of patients and, apart from gastrointestinal adverse events, they were comparable in both treatment arms. Although the study was not powered to detect the efficacy, there was a non-significant trend toward a benefit in relapse-free survival (18-months RFS 89% vs 76%) and overall survival (2-year OS 85% vs 76%) in the midostaurin arm compared to standard treatment alone [44].
Sorafenib
Several early phase studies and case reports have reported evidence for the efficacy of sorafenib maintenance therapy after allo-HCT in patients with FLT3-ITD AML [45,46,47]. The results of a placebo controlled randomized phase II trial (SORMAIN trial) indicated a higher relapse-free survival (24-months RFS 85% vs 53%, p = 0.002) and overall survival (2-year OS: 90.5% vs 66.2%, p = 0.007) in the sorafenib group compared to the placebo group [48]. These results were in agreement with a multicenter open-label randomized phase III trial [49], and by several real-world retrospective studies [50,51,52]. A recent retrospective study reported a higher overall survival and leukemia-free survival in patients receiving sorafenib as maintenance therapy compared to one prophylactic infusion of DLI [53].
The efficacy of sorafenib is connected to side effects. A prospective single-arm pilot study [54] and the work of Morin and colleagues presented at the 62nd annual meeting of the American Society of Hematology showed a rate of up to 90% of drug interruption or dose reduction from “standard dose” of 400 mg bid mainly due to gastrointestinal and hematological (thrombocytopenia, neutropenia) toxicities [55]. Praz et al. suggested therefore a standard dose reduction to 200 mg bid, to be increased based on accurate symptom-guided dosing.
Subgroups analyses to identify variables that correlate with better outcome were conducted in both randomized trials. In the SORMAIN trial, patients who reached a MRD negativity before transplantation showed a higher benefit from sorafenib maintenance, compared to MRD-positive patients [48]. Interestingly, in the study from Xuan and colleagues, sorafenib maintenance showed the strongest benefit in patients who received allo-HCT from matched sibling donor and in patients without acute GVHD, suggesting an immunomodulatory role of maintenance therapy. On the other hand, in a study from Shao and colleagues presented at 63rd annual meeting of American Society of Hematology, the concomitant mutation of CEBPA and TET2 neutralized the positive effect of sorafenib in FLT3-ITD-mutated AML [56].
Based on these studies, the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation recommends post-transplant maintenance therapy with a FLT3 inhibitor, preferably sorafenib, for patients who undergo allo-HCT for FLT3-ITD-mutated AML [57].
Quizartinib
Phase I data on quizartinib show acceptable tolerability and feasibility of FLT3-TKI maintenance after allo-HCT and, even though very preliminary, these data show early evidence of low relapse rate with only one relapse in 13 treated patients (8%) [58].
Gilteritinib and crenolanib
Currently, a prospective phase III randomized, double-blind, multicenter trial (NCT02997202) using gilteritinib versus placebo for patients with FLT3-ITD AML as maintenance after allo-HCT is ongoing [59]. Stratified results per MRD-status on 365 enrolled patients are expected for 2025. Results of the single-arm phase II study (NCT02400255) using crenolanib as maintenance therapy after allo-HCT are not yet published.
Open issues in maintenance therapy
A comparison between sorafenib and midostaurin was conducted in a multicenter retrospective cohort study by Shimony and colleagues [60]. Here, even though only 41 patients were included and most received pre-transplantation FLT3-TKI too, maintenance therapy with sorafenib was superior to midostaurin in terms of OS and RFS (HR for survival 0.25, CI 0.07–0.89).
The optimal duration of maintenance therapy is also subject of debate. In the SORMAIN trial on sorafenib and in the ongoing clinical trials on gilteritinib and crenolanib, the maintenance therapy was conducted for up to 2 years. Midostaurin was administered in the trial for 12 months. Xuan and colleagues reduced the period of sorafenib treatment to 6 months claiming concerning about risk of developing drug resistance. Currently, the Leukemia Working Party recommends a duration of 2 years for maintenance therapy, to be adapted to tolerability [57].
One last frequently debated issue is the need of treatment of MRD positivity. FLT3 inhibitors offer a valid and relatively safe therapy in the context of MRD positivity after transplantation. Both the phase II [48] and the phase III trial [49] showed a benefit of sorafenib maintenance therapy also in MRD-positive patients after allo-HCT, with a reduction of relapse incidence at 2 years of 44% (33.3% vs 77.3% in sorafenib vs control group, HR 0.25, 95% CI 0.06–094) [49]. Since there is no randomized clinical trial to address the question which FLT3-TKI is most effective as maintenance therapy for FLT3-ITD AML, a definitive response cannot be given. However, using a TKI to reduce the risk of relapse is recommended [57].
Preclinical evidence for a role in anti-tumor immunotherapy
As previously discussed in this review, sorafenib showed clinical evidence of synergism with allo-immunity against leukemia cells and enhanced graft-versus-leukemia effect. These synergism-motivated studies in mouse models which showed that FLT3 inhibition combined with T cell infusion can lead to complete elimination of leukemia cells. Mechanistically, FLT3 inhibition reduced the expression of the transcription factor ATF4. ATF4 normally blocks interferon regulatory factor 7 (IRF7) activation and this effect was antagonized by the FLT3 inhibition. Taking away the ATF4-mediated blockade, sorafenib allowed IRF7 activation and caused IL-15 transcription in the leukemia cells which caused an increase of CD8+ CD107a+ IFNγ+ T cells, which was connected to the increased elimination of leukemia cells by activated donor T cells [20] (Fig. 1).
Increased IL-15 was detected in the blood of responder patients and caused increased mitochondrial spare respiratory capacity in T cells, which is consistent with previous reports indicating that IL-15 causes mitochondrial reprogramming in T cells [61, 62]. Sorafenib, however, is a multi-tyrosine kinase inhibitor. To answer the question if also a selective FLT3 inhibitor could enhance GvL-effect, Zhang and colleagues studied IL-15 production and T cell activation in a mouse model of FLT3-ITD-positive AML relapse after allo-HCT treated with gilteritinib with or without T lymphocyte infusion [21]. Upon FLT3 inhibition, an increased production of IL-15 and a reduction of exhaustion T cell marker could be identified. Interestingly, a short-term administration of gilteritinib alone was not able to suppress leukemia growth in the absence of T lymphocytes [21].
Development of resistance
Within few months from initial response, the development of resistance to FLT3 inhibitors can occur and this typically limits the use of FLT3-TKI as monotherapy. The first predicted mechanism of resistance against type II inhibitors is the on-target mutation of TKD at activation loop D835 or at gatekeeper F691 [17]. Accordingly, these and other on-target mutations had been found in patients treated with quizartinib and sorafenib [16, 19, 63, 64]. However, these mutations cannot explain the occurrence of resistance to type I inhibitors and the fact that only a small proportion of patients presents on-target mutations at relapse. Interesting recent next-generation sequencing analysis on AML at relapse after gilteritinib [65], midostaurin [66] and crenolanib [18] revealed the impact of clonal heterogeneity on the development of resistance to selective FLT3 inhibition in AML. One common underlying mechanism is the acquisition of activating mutations on alternative pathways, such as NRAS/KRAS [65], AXL [67], JAK-family [68], PTPN11, KIT, NF1s [66], leading to an alternative way to STAT5 phosphorylation in the same original leukemic clone or alternatively, in a FLT3-ITD independent sub-clone. These findings open the potential of multiple targeted therapies to overcome occurrence of relapse and, together with the broad inhibitory activity against multiple kinases, presumably explain the efficacy of re-challenging with a second FLT3 inhibitor after initial TKI-relapse. Accordingly, gilteritinib recently showed similar responses in patients pre-treated with midostaurin [69]. Activation of alternative pathways, such as KRAS/RAC1/ROS/NLRP3, in leukemia cells [70, 71] or non-hematopoietic cells [72] may also lead to the production of pro-inflammatory IL-1β that promotes leukemia cell proliferation in an autocrine fashion.
Summary and outlook
Based on the results obtained in clinical trials, FLT3-inhibitor maintenance is the recommended therapy for FLT3-ITD AML after allo-HCT. Gilteritinib has shown remarkable efficacy and acceptable toxicity in FLT3-ITD AML patients outside of the allo-HCT setting. However, since the ADMIRAL trial was conducted before the addition of midostaurin to induction therapy became standard of care, gilteritinib’s role in relapsed/refractory disease has to be re-evaluated carefully. For post-allo-HCT maintenance therapy, the Leukemia Working Party recommends sorafenib based to the large amount of available data and the stimulation of GvL effect. The ongoing trials on gilteritinib as maintenance and as combination therapy will clarify the importance of FLT3 inhibitors in this clinical context. In future, more data are needed to further unveil the potential advantages of these multi-kinase inhibitors, to understand and overcome possible relapse mechanisms and to fine-tune the immunogenic capacity through synergism with allo-HCT and combination with DLI.
References
Papaemmanuil E, Dohner H, Campbell PJ. Genomic classification in acute myeloid leukemia. N Engl J Med. 2016;375(9):900–1.
Schlenk RF, Dohner K, Krauter J, Frohling S, Corbacioglu A, Bullinger L, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008;358(18):1909–18.
Grafone T, Palmisano M, Nicci C, Storti S. An overview on the role of FLT3-tyrosine kinase receptor in acute myeloid leukemia: biology and treatment. Oncol Rev. 2012;6(1): e8.
Kottaridis PD, Gale RE, Linch DC. Flt3 mutations and leukaemia. Br J Haematol. 2003;122(4):523–38.
Hayakawa F, Towatari M, Kiyoi H, Tanimoto M, Kitamura T, Saito H, et al. Tandem-duplicated Flt3 constitutively activates STAT5 and MAP kinase and introduces autonomous cell growth in IL-3-dependent cell lines. Oncogene. 2000;19(5):624–31.
Yamamoto Y, Kiyoi H, Nakano Y, Suzuki R, Kodera Y, Miyawaki S, et al. Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies. Blood. 2001;97(8):2434–9.
Kiyoi H, Ohno R, Ueda R, Saito H, Naoe T. Mechanism of constitutive activation of FLT3 with internal tandem duplication in the juxtamembrane domain. Oncogene. 2002;21(16):2555–63.
Welch JS, Ley TJ, Link DC, Miller CA, Larson DE, Koboldt DC, et al. The origin and evolution of mutations in acute myeloid leukemia. Cell. 2012;150(2):264–78.
Kottaridis PD, Gale RE, Langabeer SE, Frew ME, Bowen DT, Linch DC. Studies of FLT3 mutations in paired presentation and relapse samples from patients with acute myeloid leukemia: implications for the role of FLT3 mutations in leukemogenesis, minimal residual disease detection, and possible therapy with FLT3 inhibitors. Blood. 2002;100(7):2393–8.
Stone RM, DeAngelo DJ, Klimek V, Galinsky I, Estey E, Nimer SD, et al. Patients with acute myeloid leukemia and an activating mutation in FLT3 respond to a small-molecule FLT3 tyrosine kinase inhibitor, PKC412. Blood. 2005;105(1):54–60.
Knapper S, Burnett AK, Littlewood T, Kell WJ, Agrawal S, Chopra R, et al. A phase 2 trial of the FLT3 inhibitor lestaurtinib (CEP701) as first-line treatment for older patients with acute myeloid leukemia not considered fit for intensive chemotherapy. Blood. 2006;108(10):3262–70.
Borthakur G, Kantarjian H, Ravandi F, Zhang W, Konopleva M, Wright JJ, et al. Phase I study of sorafenib in patients with refractory or relapsed acute leukemias. Haematologica. 2011;96(1):62–8.
Schlenk RF, Weber D, Fiedler W, Salih HR, Wulf G, Salwender H, et al. Midostaurin added to chemotherapy and continued single-agent maintenance therapy in acute myeloid leukemia with FLT3-ITD. Blood. 2019;133(8):840–51.
Perl AE, Martinelli G, Cortes JE, Neubauer A, Berman E, Paolini S, et al. Gilteritinib or chemotherapy for relapsed or refractory FLT3-mutated AML. N Engl J Med. 2019;381(18):1728–40.
Daver N, Cortes J, Ravandi F, Patel KP, Burger JA, Konopleva M, et al. Secondary mutations as mediators of resistance to targeted therapy in leukemia. Blood. 2015;125(21):3236–45.
Smith CC, Paguirigan A, Jeschke GR, Lin KC, Massi E, Tarver T, et al. Heterogeneous resistance to quizartinib in acute myeloid leukemia revealed by single-cell analysis. Blood. 2017;130(1):48–58.
Smith CC, Wang Q, Chin CS, Salerno S, Damon LE, Levis MJ, et al. Validation of ITD mutations in FLT3 as a therapeutic target in human acute myeloid leukaemia. Nature. 2012;485(7397):260–3.
Zhang H, Savage S, Schultz AR, Bottomly D, White L, Segerdell E, et al. Clinical resistance to crenolanib in acute myeloid leukemia due to diverse molecular mechanisms. Nat Commun. 2019;10(1):244.
Heidel F, Solem FK, Breitenbuecher F, Lipka DB, Kasper S, Thiede MH, et al. Clinical resistance to the kinase inhibitor PKC412 in acute myeloid leukemia by mutation of Asn-676 in the FLT3 tyrosine kinase domain. Blood. 2006;107(1):293–300.
Mathew NR, Baumgartner F, Braun L, David O’Sullivan, Thomas S, Waterhouse M, Müller TA, Hanke K, Taromi S, Apostolova P, Illert AL, Melchinger W, Duquesne S, Schmitt-Graeff A, Osswald L, Yan K-L, Weber A, Tugues S, Spath S, Pfeifer D, Follo M, Claus R, Lübbert M, Rummelt C, Bertz H, Wäsch R, Haag J, Schmidts A, Schultheiss M, Bettinger M, Thimme R, Ullrich E, Tanriver Y, Vuong GL, Arnold R, Hemmati P, Wolf D, Ditschkowski M, Jilg C, Wilhelm K, Leiber C, Gerull S, Halter J, Lengerke C, Pabst T, Schroeder T, Kobbe G, Rösler W, Doostkam S, Meckel S, Stabla K, Metzelder SK, Halbach S, Brummer T, Hu Z, Dengjel J, Hackanson B, Schmid C, Holtick U, Scheid C, Spyridonidis A, Stölzel F, Ordemann F, Müller LP, Sicre-de-Fontbrune F, Ihorst G, Kuball J, Ehlert JE, Feger D, Wagner EV, Cahn JY, Schnell J, Kuchenbauer F, Bunjes D, Chakraverty R, Richardson S, Gill S, Kröger N, Ayuk F, Vago L, Ciceri F, Müller AM, Kondo T, Teshima T, Klaeger S, Kuster B, Kim D, Weisdorf D, van der Velden W, Dörfel D, Bethge W, Hilgendorf I, Hochhaus A, Andrieux G, Börries M, Busch H, Magenau J, Reddy P, Labopin M, Antin HJ, Henden AS, Hill GR, Kennedy GA, Bar M, Sarma A, McLornan D, Mufti G, Oran B, Rezvani K, Sha O, Negrin RS, Nagler A, Prinz M, Burchert A, Neubauer A, Beelen D, Mackensen A, von Bubnoff N, Herr W, Becher B, Socié G, Caligiuri MA, Ruggiero E, Bonini C, Häcker G, Duyster J, Finke J, Pearce E, Blazar BR, Zeiser R. Sorafenib promotes graft-versus-leukemia activity in mice and humans through IL-15 production in FLT3-ITD mutant leukemia cells. Nat Med. 2018;24:282–91.
Zhang Z, Hasegawa Y, Hashimoto D, Senjo H, Kikuchi R, Chen X, Yoneda K, Sekiguchi T, Kawase T, Tsuzuki H, Ishio T, Ara T, Ohigashi H, Nakagawa M, Teshima T. Gilteritinib enhances graft-versus-leukemia effects against FLT3-ITD mutant leukemia after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2022. https://doi.org/10.1038/s41409-022-01619-4 (Epub ahead of print).
Liang EC, Chen C, Lu R, Mannis GN, Muffly L. Measurable residual disease status and FLT3 inhibitor therapy in patients with FLT3-ITD mutated AML following allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2021;56(12):3091–3.
Blatte TJ, Schmalbrock LK, Skambraks S, Lux S, Cocciardi S, Dolnik A, et al. getITD for FLT3-ITD-based MRD monitoring in AML. Leukemia. 2019;33(10):2535–9.
Sharma M, Ravandi F, Bayraktar UD, Chiattone A, Bashir Q, Giralt S, et al. Treatment of FLT3-ITD-positive acute myeloid leukemia relapsing after allogeneic stem cell transplantation with sorafenib. Biol Blood Marrow Transplant. 2011;17(12):1874–7.
Winkler J, Rech D, Kallert S, Rech J, Meidenbauer N, Roesler W, et al. Sorafenib induces sustained molecular remission in FLT3-ITD positive AML with relapse after second allogeneic stem cell transplantation without exacerbation of acute GVHD: a case report. Leuk Res. 2010;34(10):e270–2.
Sora F, Chiusolo P, Metafuni E, Bellesi S, Giammarco S, Laurenti L, et al. Sorafenib for refractory FMS-like tyrosine kinase receptor-3 (FLT3/ITD+) acute myeloid leukemia after allogenic stem cell transplantation. Leuk Res. 2011;35(3):422–3.
Metzelder SK, Schroeder T, Finck A, Scholl S, Fey M, Götze K, et al. High activity of sorafenib in FLT3-ITD-positive acute myeloid leukemia synergizes with allo-immune effects to induce sustained responses. Leukemia. 2012;26:2353–9.
Metzelder S, Schroeder T, Lübbert M, et al. Long-term survival of sorafenib-treated FLT3-ITD-positive acute myeloid leukaemia patients relapsing after allogeneic stem cell transplantation. Eur J Cancer. 2017;86:233–9.
De Freitas T, Marktel S, Piemontese S, Carrabba MG, Tresoldi C, Messina C, Lupo C, Stanghellini MT, Assanelli A, Corti C, Bernardi M, Peccatori J, Vago L, Ciceri F. High rate of hematological responses to sorafenib in FLT3-ITD acute myeloid leukemia relapsed after allogeneic hematopoietic stem cell transplantation. Eur J Haematol. 2016;96:629–36.
Tschan-Plessl A, Halter JP, Heim D, Medinger M, Passweg JR, Gerull S. Synergistic effect of sorafenib and cGvHD in patients with high-risk FLT3-ITD+AML allows long-term disease control after allogeneic transplantation. Ann Hematol. 2015;94:1899–905.
Krüger WH, Hirt C, Kiefer T, Neumann T, Busemann C, Dölken G. Molecular remission of FLT3-ITD (+) positive AML relapse after allo-SCT by acute GVHD in addition to sorafenib. Bone Marrow Transplant. 2012;47:137–8.
Rautenberg C, Nachtkamp K, Dienst A, Schmidt PV, Heyn C, Kondakci M, Germing U, Haas R, Kobbe G, Schroeder T. Sorafenib and Azacitidine as salvage therapy for relapse of FLT3-ITD mutated AML after allo-SCT. Eur J Haematol. 2017;98:348–54.
Xuan L, Wang Y, Chen J, Jiang E, Gao L, Wu B, et al. Sorafenib therapy is associated with improved outcomes for FMS-like tyrosine kinase 3 internal tandem duplication acute myeloid leukemia relapsing after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2019;25(8):1674–81.
Kampa-Schittenhelm KM, Heinrich MC, Akmut F, Dohner H, Dohner K, Schittenhelm MM. Quizartinib (AC220) is a potent second generation class III tyrosine kinase inhibitor that displays a distinct inhibition profile against mutant-FLT3, -PDGFRA and -KIT isoforms. Mol Cancer. 2013;12:19.
Cortes JE, Kantarjian H, Foran JM, Ghirdaladze D, Zodelava M, Borthakur G, et al. Phase I study of quizartinib administered daily to patients with relapsed or refractory acute myeloid leukemia irrespective of FMS-like tyrosine kinase 3-internal tandem duplication status. J Clin Oncol. 2013;31(29):3681–7.
Usuki K, Handa H, Choi I, Yamauchi T, Iida H, Hata T, et al. Safety and pharmacokinetics of quizartinib in Japanese patients with relapsed or refractory acute myeloid leukemia in a phase 1 study. Int J Hematol. 2019;110(6):654–64.
Cortes JE, Khaled S, Martinelli G, Perl AE, Ganguly S, Russell N, et al. Quizartinib versus salvage chemotherapy in relapsed or refractory FLT3-ITD acute myeloid leukaemia (QuANTUM-R): a multicentre, randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2019;20(7):984–97.
Perl AE, Altman JK, Cortes J, Smith C, Litzow M, Baer MR, et al. Selective inhibition of FLT3 by gilteritinib in relapsed or refractory acute myeloid leukaemia: a multicentre, first-in-human, open-label, phase 1–2 study. Lancet Oncol. 2017;18(8):1061–75.
Usuki K, Sakura T, Kobayashi Y, Miyamoto T, Iida H, Morita S, et al. Clinical profile of gilteritinib in Japanese patients with relapsed/refractory acute myeloid leukemia: an open-label phase 1 study. Cancer Sci. 2018;109(10):3235–44.
Hosono N, Yokoyama H, Aotsuka N, Ando K, Iida H, Ishikawa T, et al. Gilteritinib versus chemotherapy in Japanese patients with FLT3-mutated relapsed/refractory acute myeloid leukemia. Int J Clin Oncol. 2021;26(11):2131–41.
Maiti A, DiNardo CD, Daver NG, Rausch CR, Ravandi F, Kadia TM, et al. Triplet therapy with venetoclax, FLT3 inhibitor and decitabine for FLT3-mutated acute myeloid leukemia. Blood Cancer J. 2021;11(2):25.
Schlenk RF, Weber D, Fiedler W, et al. Midostaurin added to chemotherapy and continued single-agent maintenance therapy in acute myeloid leukemia with FLT3-ITD. Blood. 2019;133(8):840–51.
Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med. 2017;377(5):454–64.
Maziarz RT, Levis M, Patnaik MM, Scott BL, Mohan SR, Deol A, et al. Midostaurin after allogeneic stem cell transplant in patients with FLT3-internal tandem duplication-positive acute myeloid leukemia. Bone Marrow Transplant. 2021;56(5):1180–9.
Chen YB, Li S, Lane AA, Connolly C, Del Rio C, Valles B, Curtis M, Ballen K, Cutler C, Dey BR, El-Jawahri A, Fathi AT, Ho VT, Joyce A, McAfee S, Rudek M, Rajkhowa T, Verselis S, Antin JH, Spitzer TR, Levis M, Soiffer R. Phase I trial of maintenance sorafenib after allogeneic hematopoietic stem cell transplantation for FMS-like tyrosine kinase 3 internal tandem duplication acute myeloid leukemia. Biol Blood Marrow Transplant. 2014;20:2042–8.
Antar A, Kharfan-Dabaja MA, Mahfouz R, Bazarbachi A. Sorafenib maintenance appears safe and improves clinical outcomes in FLT3-ITD acute myeloid leukemia after allogeneic hematopoietic cell transplantation. Clin Lymphoma Myeloma Leuk. 2015;15:298–302.
Tarlock K, Chang B, Cooper T, Gross T, Gupta S, Neudorf S, Adlard K, Ho PA, McGoldrick S, Watt T, Templeman T, Sisler I, Garee A, Thomson B, Woolfrey A, Estey E, Meshinchi S, Pollard JA. Sorafenib treatment following hematopoietic stem cell transplant in pediatric FLT3/ITD acute myeloid leukemia. Pediatr Blood Cancer. 2015;62:1048–54.
Burchert A, Bug G, Finke J, Stelljes M, Rollig C, Wäsch R, et al. Sorafenib as maintenance therapy post allogeneic stem cell transplantation for FLT3-ITD positive AML: results from the randomized, double-blind, placebo-controlled multicentre sormain trial. Blood. 2018; ASH meeting 2018 (abstract number 661).
Xuan L, Wang Y, Huang F, Fan Z, Xu Y, Sun J, et al. Sorafenib maintenance in patients with FLT3-ITD acute myeloid leukaemia undergoing allogeneic haematopoietic stem-cell transplantation: an open-label, multicentre, randomised phase 3 trial. Lancet Oncol. 2020;21(9):1201–12.
Bazarbachi A, Labopin M, Battipaglia G, Djabali A, Forcade E, Arcese W, et al. Allogeneic stem cell transplantation for FLT3-mutated acute myeloid leukemia: in vivo T-cell depletion and posttransplant sorafenib maintenance improve survival. A retrospective acute leukemia working party-European Society for Blood and Marrow Transplant Study. Clin Hematol Int. 2019;1(1):58–74.
Battipaglia G, Ruggeri A, Massoud R, El Cheikh J, Jestin M, Antar A, et al. Efficacy and feasibility of sorafenib as a maintenance agent after allogeneic hematopoietic stem cell transplantation for Fms-like tyrosine kinase 3-mutated acute myeloid leukemia. Cancer. 2017;123(15):2867–74.
Brunner AM, Li S, Fathi AT, Wadleigh M, Ho VT, Collier K, Connolly C, Ballen KK, Cutler CS, Dey BR, El-Jawahri A, Nikiforow S, McAfee SL, Koreth J, Deangelo DJ, Alyea EP, Antin JH, Spitzer TR, Stone RM, Soiffer RJ, Chen YB. Haematopoietic cell transplantation with and without sorafenib maintenance for patients with FLT3-ITD acute myeloid leukaemia in first complete remission. Br J Haematol. 2016;175:496–504.
Shi J, Cao L, Luo Y, Zhao Y, Tan Y, Yu J, et al. Maintenance sorafenib is superior to prophylactic donor lymphocyte infusion at improving the prognosis of acute myeloid leukemia with FMS-like tyrosine kinase 3 internal tandem duplication after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2021;56(1):293–6.
Pratz KW, Rudek MA, Smith BD, Karp J, Gojo I, Dezern A, et al. A prospective study of peritransplant sorafenib for patients with FLT3-ITD acute myeloid leukemia undergoing allogeneic transplantation. Biol Blood Marrow Transplant. 2020;26(2):300–6.
Morin S, Giannotti F, Mamez A-C, Masouridi-Levrat S, Simonetta F, Chalandon Y. Real-life experience of sorafenib maintenance after allogeneic hematopoietic stem cell transplantation for FLT3-ITD AML reveals high rates of toxicity-related treatment interruption. Blood. 2020;136(Supplement 1):5–6.
Shao R, Liu Q. Impact of concomitant genetic abnormalities on sorafenib therapy in FLT3-ITD positive acute myeloid leukemia undergoing allo-HSCT. Blood. 2021;138(Supplement 1):3468.
Bazarbachi A, Bug G, Baron F, Brissot E, Ciceri F, Dalle IA, et al. Clinical practice recommendation on hematopoietic stem cell transplantation for acute myeloid leukemia patients with FLT3-internal tandem duplication: a position statement from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2020;105(6):1507–16.
Sandmaier BM, et al. Results of a phase 1 study of quizartinib as maintenance therapy in subjects with acute myeloid leukemia in remission following allogeneic hematopoietic stem cell transplant. Am J Hematol. 2018;93:222–31.
NCT02997202. A trial of the FMS-like tyrosine kinase 3 (FLT3) inhibitor gilteritinib administered as maintenance therapy following allogeneic transplant for patients with FLT3/internal tandem duplication (ITD) acute myeloid leukemia (AML). ClinicalTrialsgov. 2017.
Shimony S, Yeshurun M, Wolach O, Ram R, Rozovski U, Shargian L, et al. Post-transplantation maintenance with sorafenib or midostaurin for FLT3 positive AML patients—a multicenter retrospective observational study. Leuk Lymphoma. 2021;62(10):2475–81.
Buck MD, O’Sullivan D, Klein Geltink RI, Curtis JD, Chang CH, Sanin DE, Qiu J, Kretz O, Braas D, van der Windt GJ, Chen Q, Huang SC, O’Neill CM, Edelson BT, Pearce EJ, Sesaki H, Huber TB, Rambold AS, Pearce EL. Mitochondrial dynamics controls T cell fate through metabolic programming. Cell. 2016;166:63–76.
van der Windt GJ, Everts B, Chang CH, Curtis JD, Freitas TC, Amiel E, Pearce EJ, Pearce EL. Mitochondrial respiratory capacity is a critical regulator of CD8+ T cell memory development. Immunity. 2012;36:68–78.
Man CH, Fung TK, Ho C, Han HH, Chow HC, Ma AC, et al. Sorafenib treatment of FLT3-ITD(+) acute myeloid leukemia: favorable initial outcome and mechanisms of subsequent nonresponsiveness associated with the emergence of a D835 mutation. Blood. 2012;119(22):5133–43.
von Bubnoff N, Rummelt C, Menzel H, Sigl M, Peschel C, Duyster J. Identification of a secondary FLT3/A848P mutation in a patient with FLT3-ITD-positive blast phase CMML and response to sunitinib and sorafenib. Leukemia. 2010;24(8):1523–5.
McMahon CM, Ferng T, Canaani J, Wang ES, Morrissette JJD, Eastburn DJ, et al. Clonal selection with RAS pathway activation mediates secondary clinical resistance to selective FLT3 inhibition in acute myeloid leukemia. Cancer Discov. 2019;9(8):1050–63.
Schmalbrock LK, Dolnik A, Cocciardi S, Strang E, Theis F, Jahn N, et al. Clonal evolution of acute myeloid leukemia with FLT3-ITD mutation under treatment with midostaurin. Blood. 2021;137(22):3093–104.
Dumas PY, Naudin C, Martin-Lanneree S, Izac B, Casetti L, Mansier O, et al. Hematopoietic niche drives FLT3-ITD acute myeloid leukemia resistance to quizartinib via STAT5-and hypoxia-dependent upregulation of AXL. Haematologica. 2019;104(10):2017–27.
Rummelt C, Gorantla SP, Meggendorfer M, Charlet A, Endres C, Dohner K, et al. Activating JAK-mutations confer resistance to FLT3 kinase inhibitors in FLT3-ITD positive AML in vitro and in vivo. Leukemia. 2021;35(7):2017–29.
Numan Y, Abdel Rahman Z, Grenet J, Boisclair S, Bewersdorf JP, Collins C, et al. Gilteritinib clinical activity in relapsed/refractory FLT3 mutated acute myeloid leukemia previously treated with FLT3 inhibitors. Am J Hematol. 2022;97(3):322–8.
Hamarsheh S, Osswald L, Saller BS, Unger S, De Feo D, Vinnakota JM, Konantz M, Uhl FM, Becker H, Lübbert M, Shoumariyeh K, Schürch C, Andrieux G, Venhoff N, Schmitt-Graeff A, Duquesne S, Pfeifer D, Cooper MA, Lengerke C, Boerries M, Duyster J, Niemeyer CM, Erlacher M, Blazar BR, Becher B, Groß O, Brummer T, Zeiser R. Oncogenic KrasG12D causes myeloproliferation via NLRP3 inflammasome activation. Nat Commun. 2020;11:1659.
Hamarsheh S, Zeiser R. NLRP3 inflammasome activation in cancer: a double-edged sword. Front Immunol. 2020;11:1444.
Osswald L, Hamarsheh S, Uhl FM, Andrieux G, Klein C, Dierks C, Duquesne S, Braun LM, Schmitt-Graeff A, Duyster J, Boerries M, Brummer T, Zeiser R. Oncogenic KrasG12D activation in the nonhematopoietic bone marrow microenvironment causes myelodysplastic syndrome in mice. Mol Cancer Res. 2021. https://doi.org/10.1158/541-7786.MCR-20-0275 (Epub ahead of print).
Acknowledgements
R.Z. was supported by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation)—SFB-1479—Project ID: 441891347.
Funding
Open Access funding enabled and organized by Projekt DEAL. R.Z. was supported by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation)—SFB-1479—Project ID: 441891347.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F.B. has no conflict of interest to declare. R.Z. received honoraria from Novartis, Sanofi and Mallinckrodt outside of the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Biavasco, F., Zeiser, R. FLT3-inhibitor therapy for prevention and treatment of relapse after allogeneic hematopoietic cell transplantation. Int J Hematol 116, 341–350 (2022). https://doi.org/10.1007/s12185-022-03352-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-022-03352-6