Abstract
Purpose of Review
Patellofemoral instability involves complex, three-dimensional pathological anatomy. However, current clinical evaluation and diagnosis relies on attempting to capture the pathology through numerous two-dimensional measurements. This current review focuses on recent advancements in patellofemoral imaging and three-dimensional modeling.
Recent Findings
Several studies have demonstrated the utility of dynamic imaging modalities. Specifically, radiographic patellar tracking correlates with symptomatic instability, and quadriceps activation and weightbearing alter patellar kinematics. Further advancements include the study of three-dimensional models. Automation of commonly utilized measurements such as tibial tubercle–trochlear groove (TT-TG) distance has the potential to resolve issues with inter-rater reliability and fluctuation with knee flexion or tibial rotation. Future directions include development of robust computational models (e.g., finite element analysis) capable of incorporating patient-specific data for surgical planning purposes.
Summary
While several studies have utilized novel dynamic imaging and modeling techniques to enhance our understanding of patellofemoral joint mechanics, these methods have yet to find a definitive clinical utility. Further investigation is required to develop practical implementation into clinical workflow.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mason JJ, Leszko F, Johnson T, Komistek RD. Patellofemoral joint forces. J Biomech. 2008;41(11):2337–48. https://doi.org/10.1016/j.jbiomech.2008.04.039.
Amis AA. Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthroscopy Rev. 2007;15(2).
Dietrich TJ, Fucentese SF, Pfirrmann CW. Imaging of individual anatomical risk factors for patellar instability. Seminars in musculoskeletal radiology: Thieme Medical Publishers; 2016. p. 065-73.
van Huyssteen AL, Hendrix MR, Barnett AJ, Wakeley CJ, Eldridge JD. Cartilage-bone mismatch in the dysplastic trochlea. An MRI study. J Bone Joint Surg Br. 2006;88(5):688–91. https://doi.org/10.1302/0301-620x.88b5.16866.
Huddleston HP, Redondo ML, Cregar WM, Christian DR, Hannon CP, Yanke AB. The effect of aberrant rotation on radiographic patellar height measurement using Canton-Deschamps Index: a cadaveric analysis. J Knee Surg. 2021. https://doi.org/10.1055/s-0041-1731720.
Aarvold A, Pope A, Sakthivel VK, Ayer RV. MRI performed on dedicated knee coils is inaccurate for the measurement of tibial tubercle trochlear groove distance. Skeletal Radiol. 2014;43(3):345–9. https://doi.org/10.1007/s00256-013-1790-5.
Ye Q, Yu T, Wu Y, Ding X, Gong X. Patellar instability: the reliability of magnetic resonance imaging measurement parameters. BMC Musculoskelet Disord. 2019;20(1):317. https://doi.org/10.1186/s12891-019-2697-7.
Kazley JM, Banerjee S. Classifications in brief: the Dejour classification of trochlear dysplasia. Clin Orthop Relat Res. 2019;477(10):2380–6. https://doi.org/10.1097/CORR.0000000000000886.
Lippacher S, Dejour D, Elsharkawi M, Dornacher D, Ring C, Dreyhaupt J, Reichel H, Nelitz M. Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med. 2012;40(4):837–43. https://doi.org/10.1177/0363546511433028.
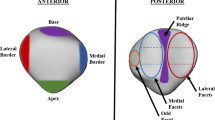
• Pennock AT, Chang A, Doan J, Bomar JD, Edmonds EW. 3D knee trochlear morphology assessment by magnetic resonance imaging in patients with normal and dysplastic trochleae. Journal of Pediatric Orthopaedics. 2020;40(3):114–9 Sucessfully generated and measured three-dimensional parameters of trochlear models, finding significant differences from healthy controls particularly in the proximal trochlea.
Grimm NL, Levy BJ, Jimenez AE, Crepeau AE, Pace JL. Traumatic patellar dislocations in childhood and adolescents. Orthopedic Clinics. 2020;51(4):481–91.
Yu Z, Yao J, Wang X, Xin X, Zhang K, Cai H, Fan Y, Yang B. Research methods and progress of patellofemoral joint kinematics: a review. J Healthcare Eng. 2019;2019:9159267. https://doi.org/10.1155/2019/9159267.
Hirschmann A, Buck FM, Fucentese SF, Pfirrmann CWA. Upright CT of the knee: the effect of weight-bearing on joint alignment. Eur Radiol. 2015;25(11):3398–404. https://doi.org/10.1007/s00330-015-3756-6.
•• Becher C, Fleischer B, Rase M, Schumacher T, Ettinger M, Ostermeier S, et al. Effects of upright weight bearing and the knee flexion angle on patellofemoral indices using magnetic resonance imaging in patients with patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2405–13. https://doi.org/10.1007/s00167-015-3829-8Upright weightbearing significantly increased patellar tilt, height, and bisect offset in full extension.
Marzo J, Kluczynski M, Notino A, Bisson L. Comparison of a novel weightbearing cone beam computed tomography scanner versus a conventional computed tomography scanner for measuring patellar instability. Orthop J Sports Med. 2016;4(12):2325967116673560. https://doi.org/10.1177/2325967116673560.
•• Frings J, Dust T, Krause M, Ohlmeier M, Frosch K-H, Adam G, et al. Objective assessment of patellar maltracking with 3 T dynamic magnetic resonance imaging: feasibility of a robust and reliable measuring technique. Sci Rep. 2020;10(1):16770. https://doi.org/10.1038/s41598-020-72332-9Demonstrated reliability of dynamic MRI technique for evaluation of patellar maltracking and correlation with traditional anatomic factors (e.g. tibial tubercle-trochlear groove (TT-TG) distance, patellar height).
•• Tanaka MJ, Elias JJ, Williams AA, Demehri S, Cosgarea AJ. Characterization of patellar maltracking using dynamic kinematic CT imaging in patients with patellar instability. Knee Surg, Sports Traumatol, Arthrosc. 2016;24(11):3634–41. https://doi.org/10.1007/s00167-016-4216-9Identified an objective measurement of patellar maltracking. Radiographic J-sign of 2 quadrants correlated reliably with patellar instability symptoms.
Burke CJ, Kaplan D, Block T, Chang G, Jazrawi L, Campbell K, Alaia M. Clinical utility of continuous radial magnetic resonance imaging acquisition at 3 T in real-time patellofemoral kinematic assessment: a feasibility study. Arthrosc J Arthrosc Relat Surg. 2018;34(3):726–33. https://doi.org/10.1016/j.arthro.2017.09.020.
Carlson VR, Sheehan FT, Shen A, Yao L, Jackson JN, Boden BP. The relationship of static tibial tubercle–trochlear groove measurement and dynamic patellar tracking. Am J Sports Med. 2017;45(8):1856–63. https://doi.org/10.1177/0363546517700119.
Tanaka MJ, Elias JJ, Williams AA, Carrino JA, Cosgarea AJ. Correlation between changes in tibial tuberosity–trochlear groove distance and patellar position during active knee extension on dynamic kinematic computed tomographic imaging. Arthrosc J Arthrosc Relat Surg. 2015;31(9):1748–55. https://doi.org/10.1016/j.arthro.2015.03.015.
Williams AA, Elias JJ, Tanaka MJ, Thawait GK, Demehri S, Carrino JA, Cosgarea AJ. The relationship between tibial tuberosity–trochlear groove distance and abnormal patellar tracking in patients with unilateral patellar instability. Arthrosc J Arthrosc Relat Surg. 2016;32(1):55–61. https://doi.org/10.1016/j.arthro.2015.06.037.
Gobbi RG, Demange MK, de Ávila LFR, Araújo Filho JDAB, Moreno RA, Gutierrez MA, et al. Patellar tracking after isolated medial patellofemoral ligament reconstruction: dynamic evaluation using computed tomography. Knee Surg, Sports Traumatol, Arthrosc. 2017;25(10):3197–205. https://doi.org/10.1007/s00167-016-4284-x.
Haj-Mirzaian A, Thawait GK, Tanaka MJ, Demehri S. Diagnosis and characterization of patellofemoral instability: review of available imaging modalities. Sports Med Arthrosc Rev. 2017;25(2):64–71.
Demehri S, Thawait GK, Williams AA, Kompel A, Elias JJ, Carrino JA, Cosgarea AJ. Imaging characteristics of contralateral asymptomatic patellofemoral joints in patients with unilateral instability. Radiology. 2014;273(3):821–30. https://doi.org/10.1148/radiol.14140295.
Lansdown DA, Ma CB. Clinical utility of advanced imaging of the knee. J Orthop Res. 2020;38(3):473–82. https://doi.org/10.1002/jor.24462.
• Esfandiarpour F, Lebrun CM, Dhillon S, Boulanger P. In-vivo patellar tracking in individuals with patellofemoral pain and healthy individuals. J Orthop Res. 2018;36(8):2193–201. https://doi.org/10.1002/jor.23887Demonstrated via biplanar fluoroscopy that patients with patellofemoral pain had increased patellar tilt and range in weightbearing extension and deep lunge tasks compared to normal controls with minimal change.
Gustafson JA, Elias JJ, Fitzgerald GK, Tashman S, Debski RE, Farrokhi S. Combining advanced computational and imaging techniques as a quantitative tool to estimate patellofemoral joint stress during downhill gait: a feasibility study. Gait Posture. 2021;84:31–7. https://doi.org/10.1016/j.gaitpost.2020.11.016.
Weber AE, Nathani A, Dines JS, Allen AA, Shubin-Stein BE, Arendt EA, Bedi A. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98(5):417–27. https://doi.org/10.2106/jbjs.O.00354.
Dai Z-Z, Sha L, Zhang Z-M, Liang Z-P, Li H, Li H. Comparing the tibial tuberosity–trochlear groove distance between CT and MRI in skeletally immature patients with and without patellar instability. Orthop J Sports Med. 2021;9(1):232596712097366. https://doi.org/10.1177/2325967120973665.
Camp CL, Heidenreich MJ, Dahm DL, Bond JR, Collins MS, Krych AJ. A simple method of measuring tibial tubercle to trochlear groove distance on MRI: description of a novel and reliable technique. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):879–84. https://doi.org/10.1007/s00167-014-3405-7.
Suomalainen J-S, Regalado G, Joukainen A, Kääriäinen T, Könönen M, Manninen H, et al. Effects of knee flexion and extension on the tibial tuberosity–trochlear groove (TT–TG) distance in adolescents. J Exp Orthop. 2018;5(1). https://doi.org/10.1186/s40634-018-0149-1.
Marquez-Lara A, Andersen J, Lenchik L, Ferguson CM, Gupta P. Variability in patellofemoral alignment measurements on MRI: influence of knee position. Am J Roentgenol. 2017;208(5):1097–102. https://doi.org/10.2214/ajr.16.17007.
Worden A, Kaar S, Owen J, Cutuk A. Radiographic and anatomic evaluation of tibial tubercle to trochlear groove distance. J Knee Surg. 2016;29(7):589–93. https://doi.org/10.1055/s-0035-1569478.
• Chen H, Kluijtmans L, Bakker M, Dunning H, Kang Y, van de Groes S, et al. A robust and semi-automatic quantitative measurement of patellofemoral instability based on four dimensional computed tomography. Med Eng Phys. 2020;78:29–38. https://doi.org/10.1016/j.medengphy.2020.01.012Developed an automated method for calculation of TT-TG and patella center-trochlear groove (PC-TG) in a dynamic knee model. This required a manual segmentation step.
Lenchik L, Heacock L, Weaver AA, Boutin RD, Cook TS, Itri J, Filippi CG, Gullapalli RP, Lee J, Zagurovskaya M, Retson T, Godwin K, Nicholson J, Narayana PA. Automated segmentation of tissues using CT and MRI: a systematic review. Acad Radiol. 2019;26(12):1695–706. https://doi.org/10.1016/j.acra.2019.07.006.
Cheng R, Alexandridi NA, Smith RM, Shen A, Gandler W, McCreedy E, McAuliffe MJ, Sheehan FT. Fully automated patellofemoral MRI segmentation using holistically nested networks: implications for evaluating patellofemoral osteoarthritis, pain, injury, pathology, and adolescent development. Magn Reson Med. 2020;83(1):139–53. https://doi.org/10.1002/mrm.27920.
Lecun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521(7553):436–44. https://doi.org/10.1038/nature14539.
Lundervold AS, Lundervold A. An overview of deep learning in medical imaging focusing on MRI. Zeitschrift für Medizinische Physik. 2019;29(2):102–27. https://doi.org/10.1016/j.zemedi.2018.11.002.
Litjens G, Kooi T, Bejnordi BE, Setio AAA, Ciompi F, Ghafoorian M, van der Laak JAWM, van Ginneken B, Sánchez CI. A survey on deep learning in medical image analysis. Med Image Anal. 2017;42:60–88. https://doi.org/10.1016/j.media.2017.07.005.
Ali AA, Shalhoub SS, Cyr AJ, Fitzpatrick CK, Maletsky LP, Rullkoetter PJ, Shelburne KB. Validation of predicted patellofemoral mechanics in a finite element model of the healthy and cruciate-deficient knee. J Biomech. 2016;49(2):302–9. https://doi.org/10.1016/j.jbiomech.2015.12.020.
Guan W, Sun Y, Qi X, Hu Y, Duan C, Tao H, et al. Spinal biomechanics modeling and finite element analysis of surgical instrument interaction. Comput Assist Surg (Abingdon). 2019;24(supp1):151–9. https://doi.org/10.1080/24699322.2018.1560086.
Zheng M, Zou Z, Bartolo PJ, Peach C, Ren L. Finite element models of the human shoulder complex: a review of their clinical implications and modelling techniques. Int J Numer Method Biomed Eng. 2017;33(2). https://doi.org/10.1002/cnm.2777.
Shu L, Sato T, Hua X, Sugita N. Comparison of kinematics and contact mechanics in normal knee and total knee replacements: a computational investigation. Ann Biomed Eng. 2021;49:2491–502. https://doi.org/10.1007/s10439-021-02812-0.
Loi I, Stanev D, Moustakas K. Total knee replacement: subject-specific modeling, finite element analysis, and evaluation of dynamic activities. Front Bioeng Biotechnol. 2021;9:648356. https://doi.org/10.3389/fbioe.2021.648356.
Ding K, Yang W, Wang H, Zhan S, Hu P, Bai J, Ren C, Zhang Q, Zhu Y, Chen W. Finite element analysis of biomechanical effects of residual varus/valgus malunion after femoral fracture on knee joint. Int Orthop. 2021;45(7):1827–35. https://doi.org/10.1007/s00264-021-05039-9.
Peng Y, Zhang G, Zhang S, Ji X, Li J, Du C, et al. Biomechanical study of transsacral-transiliac screw fixation versus lumbopelvic fixation and bilateral triangular fixation for “H”- and “U”-type sacrum fractures with traumatic spondylopelvic dissociation: a finite element analysis study. J Orthop Surg Res. 2021;16(1):428. https://doi.org/10.1186/s13018-021-02581-5.
Kwak DK, Bang SH, Kim WH, Lee SJ, Lee S, Yoo JH. Biomechanics of subtrochanteric fracture fixation using short cephalomedullary nails: a finite element analysis. PLoS One. 2021;16(7):e0253862. https://doi.org/10.1371/journal.pone.0253862.
Lewis GS, Mischler D, Wee H, Reid JS, Varga P. Finite element analysis of fracture fixation. Curr Osteoporos Rep. 2021;19:403–16. https://doi.org/10.1007/s11914-021-00690-y.
Minns RJ, Steven FS. The collagen fibril organization in human articular cartilage. J Anat. 1977;123(Pt 2):437–57.
Fernandez JW, Hunter PJ. An anatomically based patient-specific finite element model of patella articulation: towards a diagnostic tool. Biomech Model Mechanobiol. 2005;4(1):20–38. https://doi.org/10.1007/s10237-005-0072-0.
Guess TM, Thiagarajan G, Kia M, Mishra M. A subject specific multibody model of the knee with menisci. Med Eng Phys. 2010;32(5):505–15. https://doi.org/10.1016/j.medengphy.2010.02.020.
Baldwin MA, Clary C, Maletsky LP, Rullkoetter PJ. Verification of predicted specimen-specific natural and implanted patellofemoral kinematics during simulated deep knee bend. J Biomech. 2009;42(14):2341–8. https://doi.org/10.1016/j.jbiomech.2009.06.028.
Pal S, Besier TF, Gold GE, Fredericson M, Delp SL, Beaupre GS. Patellofemoral cartilage stresses are most sensitive to variations in vastus medialis muscle forces. Comput Methods Biomech Biomed Eng. 2019;22(2):206–16. https://doi.org/10.1080/10255842.2018.1544629.
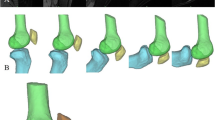
•• Kaiser D, Trummler L, Götschi T, Waibel FWA, Snedeker JG, Fucentese SF. Patellofemoral instability in trochleodysplastic knee joints and the quantitative influence of simulated trochleoplasty – a finite element simulation. Clin Biomech (Bristol). 2021;81:105216. https://doi.org/10.1016/j.clinbiomech.2020.105216Demonstrated feasibility of surgical simulation (trochleoplasty) for a patellofemoral finite element analysis model.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Advances in Patellofemoral Surgery
Rights and permissions
About this article
Cite this article
Dandu, N., Knapik, D.M., Trasolini, N.A. et al. Future Directions in Patellofemoral Imaging and 3D Modeling. Curr Rev Musculoskelet Med 15, 82–89 (2022). https://doi.org/10.1007/s12178-022-09746-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-022-09746-7