Abstract
Purpose of Review
This review provides an overview of well-established and newly developed cartilage repair techniques for cartilage defects in the patellofemoral joint (PFJ). An algorithm will be presented for approaching cartilage defects considering the distinct anatomy of both the patellar and trochlear articular surfaces.
Recent Findings
Recent studies on cartilage repair in the PFJ have demonstrated improved outcomes in an attempt to delay or obviate the need for arthroplasty, and improve symptoms in young patients. While autologous chondrocyte implantation shows good and excellent outcomes for chondral lesions, osteochondral defects are adequately addressed with osteochondral allograft transplantation. In case of patellar malalignment, concomitant tibial tubercle osteotomy can significantly improve outcomes. Particulated cartilage and bone marrow aspirate concentrate are potential new alternative treatments for cartilage repair, currently in early clinical studies.
Summary
Due to the frequency of concomitant anatomic abnormalities in the PFJ, a thorough clinical examination combined with careful indication for each procedure in each individual patient combined with meticulous surgical technique is central to achieve satisfying outcomes. Additional comparative studies of cartilage repair procedures, as well as investigation of newer techniques, are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The management of articular cartilage defects remains a challenging clinical problem for orthopedic surgeons. Articular cartilage is a highly organized tissue with complex biomechanical properties and substantial durability. However, it has poor intrinsic capacity for healing, and defects can lead to considerable functional impairment, subsequent joint degeneration, and development of osteoarthritis (OA) [1]. In the United States (US) alone, OA is a condition that affects up to 27 million people with an estimated economic cost of 89 billion US dollars annually [2].
The patellofemoral joint (PFJ) is frequently involved in symptomatic cartilage disease of the knee [3]. A recent meta-analysis revealed that, based on magnetic resonance imaging (MRI), up to 52% of patients with knee pain or symptomatic OA of the knee are diagnosed with cartilage lesions in the PFJ [4•]. Moreover, patellofemoral OA has been associated with symptoms of pain, stiffness, and functional limitations [5]. The pathomechanism of patellofemoral OA is multifactorial, including chronic repetitive microtrauma due to suboptimal extensor mechanism alignment, and acute macrotrauma, most commonly patellar dislocations, which are associated with cartilage defects in up to 95% of patients [6, 7••].
Chondral lesions on the patellar and trochlear articular surfaces are particularly challenging to manage due to the complex biomechanical environment and substantial load transmission through the PFJ during weight-bearing activity [8].
First-line conservative treatment of cartilage lesions, in general, aims to relieve inflammation and controlling pain to regain functional capacity. This can be achieved with nonsteroidal anti-inflammatory medications, intra-articular corticosteroid injections, and hyaluronic acid viscosupplementation [8]. In addition to muscle strengthening to improve absorption of physiological loads across the knee, weight loss and activity modification to avoid aggravating pain and functional limitation may improve symptoms [9, 10]. Conservative treatment of patients with anterior knee pain should be attempted for at least 3 months before considering surgical intervention, as most patients will experience pain relief with physical therapy and can therefore avoid surgical treatment [11, 12].
Surgical treatment options for focal cartilage lesions in the knee include debridement/chondroplasty, bone marrow stimulation, autologous chondrocyte implantation (ACI), osteochondral autograft transfer (OAT), osteochondral allograft transplantation (OCA), and newer techniques such as particulated cartilage procedures (autograft and juvenile allograft). Choosing a surgical treatment is based on morphological factors of the chondral lesion such as the location within the knee joint (femoral condyles vs. patellofemoral), location on the involved articular surface (i.e., inferior vs. superior patellar pole), size, depth (involvement of the subchondral bone), containment (contained vs. not contained), as well as on patient characteristics like age, body mass index (BMI), limb and extensor mechanism alignment, and activity level.
Also, adequate treatment of concomitant pathologies is crucial to the success of any cartilage repair in the knee. This review will concentrate solely on cartilage lesions in the PFJ, and therefore, tibial tubercle osteotomy (TTO) will be discussed briefly.
First described for the treatment of patellar instability [13], anteromedialization of the tibial tubercle has also been found to unload the PFJ [14]. The procedure can improve patellofemoral contact mechanics in patients with patellofemoral malalignment by transferring contact forces from distal to proximal and from lateral to medial on the patellar articular surface [15•]. Hence, this procedure is especially valuable in patients with chondral lesions on the inferior pole or lateral facet of the patella [12]. Due to its significant positive impact on clinical outcomes, TTO is frequently performed concomitantly with patellofemoral cartilage repair in patients with PF maltracking [7••, 16,17,18,19, 20••].
This article provides a review of the current state of cartilage repair in the PFJ, focusing on well-established, as well as emerging techniques meeting the distinct requirements of cartilage repair in the PFJ. Moreover, we will provide an algorithm to adequately address patellofemoral cartilage defects.
Chondroplasty
Chondroplasty, also referred to as cartilage debridement, is one of the most performed procedures involving cartilage [24]. The goal of chondroplasty is to transform an irregular and unstable cartilage lesion into a more regular and stable construct. It is typically indicated for partial or full-thickness chondral lesions smaller than 1–2 cm2 but can also be performed in larger lesions preparing the site for a subsequent cartilage repair procedure such as ACI [25]. In the senior author’s practice, most patients undergo chondroplasty during the cartilage biopsy in the first stage of an elective ACI for the PFJ and/or tibiofemoral joint (TF).
It appears of importance to create a regular lesion with stable vertical walls. However, the negative effects on cartilage viability beyond the area of resection remain controversial, and therefore, overly aggressive debridement should be avoided [26,27,28,29,30]. Surgeon’s attention is critical to neither transform a contained into an uncontained lesion nor to needlessly expose the subchondral bone [31].
Reports of clinical outcomes for chondroplasty in the PFJ remain limited. Anderson et al. [32•] retrospectively studied 86 patients who were submitted to isolated chondroplasty for chondral lesions in the knee with a mean size of 3.3 cm2 and ICRS grades 2–4. The majority of these patients had lesions in the PFJ (58.5%). The authors found that patients with lower preoperative scores gained more benefit from chondroplasty, but no correlation between anatomic location and amount of improvement could be observed. Federico and Ryder [33] reviewed the records of 36 patients who underwent arthroscopic debridement for chondral lesions of the patella. While 57.9% of patients with traumatic chondromalacia had good or excellent results, only 41.1% with atraumatic chondromalacia showed good or excellent results after chondroplasty.
Bone Marrow Stimulation
Bone marrow stimulation refers to any technique that promotes the migration of pluripotent mesenchymal stem cells from the subchondral bone to the chondral defect surface, thereby promoting fibrocartilage repair. The most popular techniques are the Pridie drilling technique, using K wires, and the microfracture technique described and popularized by Steadman and colleagues, which uses angulated awls [34, 35].
While full thickness and contained chondral lesions of up to 4 cm2 are an acceptable indication for performing microfracture in the TF, a lower threshold (2 cm2) should be considered for the PFJ. This is due to the distinctive biomechanics and higher sheer stresses in this joint, which would affect durability of the formed fibrocartilage. Furthermore, superior outcomes were observed in patients younger than 40 years, BMI under 30 kg/m2, and duration of symptoms less than 12 months. Importantly, microfracture should be avoided in uncontained chondral lesions [36].
Surgical principles remain the same regardless of the chosen technique and are paramount for success. It is essential to perform a thorough debridement all the way down to the subchondral bone, including the layer of calcified cartilage, with stable, verticals walls to create adequate containment. Next, the perforations must be perpendicular to the bony surface, at least 3 mm deep, and spaced 3 to 4 mm apart from each other (Fig. 1). This will cause bleeding, clot formation, and the migration of the pluripotent mesenchymal stem cells into the cartilage defect. As a result, fibrocartilage with type I collagen will be produced that has, however, inferior biomechanical properties compared to the type II collagen typical for native hyaline cartilage. While lesions in the trochlea can be easily addressed by arthroscopy, patellar defects are more challenging to approach. A small arthrotomy may be necessary for lesion visualization and proper instrument angulation. Additionally, counter pressure on the anterior aspect of the patella may be needed during bone marrow stimulation due to greater mobility and harder bone of the patella.
Kreuz et al. [37] evaluated 85 patients who underwent microfracture and compared the outcomes of different anatomic locations within the knee. The authors concluded that microfracture results in short-term improvement followed by a sharp decline in outcomes after 2 years of follow-up. Interestingly, the functional outcomes in patients with patellofemoral chondral lesions were worse regardless of follow-up. Mithoefer et al. [36] showed that the failure rate was up to 6% in the first 2 years, with an increase of up to 31% after 5 years of follow-up. Minas et al. [38] demonstrated a 3-fold increase in failure rate of ACI after a previous marrow stimulant procedure compared to primary ACI (26 vs. 8%), showing that microfracture can negatively affect the outcomes of subsequent procedures. Consequently, the senior author performs a bone marrow procedure only in small chondral lesions (< 2 cm2) of the PFJ (and mostly limited to the trochlea), thus maximizing the likelihood of a successful outcome without the need for subsequent procedures.
Recently, bone marrow aspirate concentrate (BMAC) has emerged as an alternative treatment option. Though its application is still under investigation, BMAC has the advantage of not damaging the local subchondral bone while allowing higher numbers of mesenchymal stem cells to be brought into the defect. The bone marrow clot is implanted into the defect under a membrane cover to stabilize the reparative tissue. [46•]. BMAC can also serve as a biological augmentation for other procedures such as OAT and OCA (Fig. 2). Hopefully, our understanding of the clinical benefits of BMAC will increase with future results of ongoing studies [46•, 47].
Autologous Chondrocyte Implantation
ACI is one of the senior author’s most performed procedures for chondral lesions in the PFJ. It allows the treatment of larger defects and matching of the complex contour of the patellar and trochlear articular surfaces. With more than 25 years of experience, ACI technology has evolved but the two-stage technique principles remain the same [48]. The first stage involves the arthroscopic harvesting of 100–300 mg of full-thickness articular cartilage from non-weight-bearing areas of the femoral condyle, or the superior and lateral margin of the intercondylar notch. In vitro, the cartilage matrix is processed and the chondrocytes are cultured for at least 2 weeks. During the second stage, the chondral defect is debrided and the cultured chondrocytes are implanted. The debridement must be performed carefully, avoiding damage to the subchondral plate and creating stable vertical walls. Then, the chondrocyte-seeded collagen membrane is placed in the defect and secured with either fibrin glue alone in case of excellent containment or fixed to the surrounding cartilage with 6-0 absorbable sutures. (Fig. 2).
The original technique, also referred to as first-generation ACI, utilized a periosteal patch that was harvested from the patient’s proximal tibia [49]. As a result of overgrowth issues and inferior outcomes, periosteal patches were progressively replaced by collagen membranes—bilayered synthetic biodegradable scaffolds for ingrowth of chondrocytes—which formed the second-generation ACI [50, 51]. Aside from the containment function, scaffolds have the potential of in vivo chondroinduction and chondroconduction [52]. In the current third-generation ACI, also known as matrix-induced autologous chondrocyte implantation (MACI), the chondrocytes are, again, cultured in vitro but replicated inside a three-dimensional scaffold membrane [53••]. While comprising the same scaffold associated potentials, the application of MACI also simplifies the surgery by omitting both the chondrocyte injection underneath a membrane and the watertight sealing to ensure chondrocyte containment within the lesion. While studies have demonstrated reduced rates of re-operation in membrane ACI compared with periosteal ACI, further comparative studies are needed to show superiority among these techniques [54, 55•, 56].
ACI is indicated in full-thickness chondral lesions larger than 3–4 cm2 and can be performed in the TF and PFJ. Preoperative assessment of the subchondral bone on MR-imaging is of critical importance. Patients with subchondral plate alterations may require concomitant bone grafting (“sandwich” technique), or osteochondral transplantation in order to address the subchondral bone. ACI should be avoided in patients with previous bone marrow stimulation procedures and significant subchondral changes such as cystic degeneration and extensive subchondral edema [38, 50].
As in other cartilage repair techniques, it is important to achieve good containment of the chondral defect prior to ACI. In patellar lesions, however, this can be more challenging to accomplish due to the unique anatomy of its articular surface. To resolve this issue, ACI can be performed in conjunction with OAT to ensure proper containment [57]. Contraindications for ACI include inflammatory arthritis, obesity, and smoking. Although considered a contraindication for primary treatment, bipolar lesions can be addressed with ACI as a salvage procedure exhibiting encouraging results [58••, 59••, 60].
In contrast to other cartilage procedures, ACI for the PFJ has been extensively studied in the literature. Initial reports of the outcome after ACI in the PFJ were disappointing [49]. Improved ACI techniques and the treatment of concomitant patellofemoral malalignment, along with better understanding of the patellofemoral biomechanics, led to enhanced outcomes in recent years [61•, 62,63,64, 65•, 66]. Gomoll et al. [6] evaluated 110 patients with patellofemoral ACI in a multi-center study across the US. A total of 84% of patients had good or excellent results after a minimum of 4-year follow-up. Similar results were obtained by von Keudell et al. [21••], showing that 83% of patients had good or excellent functional outcomes after ACI to isolated chondral lesions of the patella with a failure rate of 10% after 15 years of follow-up. As previously mentioned, lateral facet or inferior pole patellar lesions should be addressed with ACI in combination with an anteromedializing TTO to achieve improved outcomes [17, 19, 67•].
ACI sandwich technique refers to the use of two membranes with impaction grafting of the subchondral bone deficit. It has shown excellent results in the treatment of osteochondral defects on the femoral condyles [68, 69], but further studies must investigate its eligibility as primary option in the PFJ.
Lately, arthroscopic techniques for ACI have emerged showing encouraging results. Ebert et al. [70•] reported 90% of good or excellent outcomes after arthroscopic MACI with 5 years of follow-up. In contrast, Biant et al. [71•] demonstrated a 16-fold increase in cellular viability when ACI was performed using a mini-arthrotomy compared with an arthroscopic approach, suggesting that the arthroscopic procedure has the potential to negatively affect chondrocyte viability.
In a recent systematic review, Andriolo et al. [22••] evaluated 58 studies and found an overall failure rate of 14.9% for ACI across the knee joint, most of them occurring in the first 5 years without differences between ACI and MACI techniques. The authors criticized the heterogeneous description of failure among all studies and underlined the importance of a coherent definition of failure. Another systematic review looked at MACI outcomes in a 5-year follow-up period and found a significantly higher failure rate in the TF compared to the PFJ (12.4 vs. 4.7%) [23•] (Table 1)
.
ACI remains a costly treatment option for patients with chondral defects in the knee. Though, the procedure cost-effectiveness seems to be inside the range of other cartilage procedures, considering the substantial delay of other more aggressive and expensive procedures such as partial of total knee arthroplasty [72, 73•, 74•].
Osteochondral Autograft Transfer (OAT)
This technique describes the harvesting of 10–15 mm deep osteochondral cylinders from healthy, non-weight-bearing areas of the knee, typically the medial or lateral margins of the trochlea, posterior femoral condyles, or intercondylar notch, and transferring them to the defect site of the ipsilateral knee (Fig. 3). While OAT has the advantage of transferring hyaline cartilage in a one-stage procedure with good bony integration and no risk of immunologic complications, donor site morbidity remains a concern in OAT procedures. This limits the indication for OAT to only small cartilage lesions up to 2–3 cm2 in size [75]. In a biomechanical study, Garretson et al. [76] found that the medial trochlea and distal lateral trochlea had the lowest contact loads and hence could provide desirable cylinder grafts for the PFJ.
Precise graft fitting and creating of a smooth articular surface in the PFJ are essential to achieving satisfactory results in patients after OAT. In fact, graft prominence of more than 1 mm has shown to be associated with less favorable outcomes, and patients frequently describe persistent catching sensations months after the surgery [77, 78, 79•].
This is particularly challenging in the PFJ as a result of two issues: The unique anatomy of the patellar and trochlear surfaces complicates forming a smooth articular surface; every donor graft will have a thinner cartilage layer than the surrounding patella and thus, results in local cartilage bone interface mismatch [80].
Some authors reported up to 92% good to excellent results in patients with chondral lesions on the femoral condyle, while lesions in the PFJ showed 79% good to excellent results [81]. Especially patellar lesions have been reported to be associated with less favorable results with up to 100% failure rate after 1 year follow-up, which is thought to be due to the previously described anatomic characteristics of the PFJ [39•, 82]. Yet, other authors believe that patellofemoral malalignment plays an important role in the outcome of OAT to the patella. They found significant improvement in clinical outcomes and 100% graft integration after 12 months follow-up in patients with small (< 2.5 cm2) full-thickness chondral lesion of the patella without malalignment of the PFJ [40••]. Recently, Yabumoto et al. [79•] stated that if high congruity is achieved through meticulous implantation of donor grafts perpendicular to the articular surface, favorable results can be obtained for chondral lesions in the PFJ.
Osteochondral Allograft Transplantation
Osteochondral Allograft Transplantation (OCA) is possibly the most challenging cartilage procedure in the PFJ. As described for OAT, precise fitting of the harvested plug and creating a smooth surface is key to the success of the procedure. The same principle applies to OCA, but the process of donor graft matching is complicated by the anatomic complexity and variability of the PFJ. Proper assessment of preoperative imaging studies for PFJ allograft matching is yet to be determined [83, 84].
With stricter guidelines imposed by the FDA for allograft tissue acquisition and storage, the risk of disease transmission decreased and OCA has become increasingly popular as a primary or salvage procedure [24, 85]. Fresh osteochondral allografts are harvested within 24 h of donor’s death and are preserved at a temperature of 4 °C [86]. Current recommendations advise a storage time of up to 28 days, but ideal shelf life remains controversial [87, 88•]. This storage technique has shown adequate chondrocyte viability and is routinely used for OCA [86, 89].
OCA is performed via an arthrotomy with a size and side-matched donor plug to precisely press fit into the prepared defect (Fig. 4). Despite the fact that allograft immunogenicity is related to graft volume, no differences were observed in survival rates for different graft sizes [90••]. Nevertheless, reducing the thickness of the graft’s subchondral bone is thought to reduce the potential risk of immunoreaction [83]. Additionally, pulse lavage washing of the graft is performed in an attempt to decrease marrow contents [91, 92].
OCA is indicated as a primary procedure in large full-thickness cartilage lesions, typically greater than 2 cm2, with abnormal subchondral bone [83], but increasingly also for the primary treatment of pure chondral lesions. Besides the prospect of addressing uncontained defects, OCA has the advantage of being a single-stage procedure while avoiding potential donor site morbidity compared with OAT. Moreover, it is a potential option for the treatment of bipolar lesions, but with inferior results when compared to outcomes in single lesions, similar to other cartilage repair options such as ACI [43•]. It can also serve as a salvage procedure in patients after failed cartilage repair and in patients with post-traumatic osteochondral defects after knee fractures that are too young for arthroplasty [86, 89, 93, 94]. Relative contraindications for OCA include smoking and obesity as they have shown to negatively affect clinical outcomes [87, 95•]. Extensor mechanism malalignment, ligamentous instability, or other intra-articular pathologies should be simultaneously addressed if needed to achieve improved outcomes.
There is a paucity in the current literature of randomized controlled trials for OCA, and only few studies have reported outcomes for patellofemoral OCA, albeit with good results [96]. Cameron et al. [42••] evaluated 29 knees with trochlear OCA with a mean follow-up of 7 years. Graft survivorship was 100% at 5 years and 91.7% at 10 years with improvement of all functional outcomes and an overall satisfaction rate of 89%. Gracitelli et al. [41••] studied 28 knees with OCA for isolated patellar cartilage lesions with 9.7 years of mean follow-up time. Patellar allograft survivorship was 78.1% at 5 and 10 years, decreasing to 55.8% at 15 years with an overall satisfaction rate of 89%. The obtained results are in conformity with outcomes reported by previous studies [97, 98].
OCA failure rate has been shown to be higher in the PFJ than in the TF. In a systematic review, Assenmacher et al. [99•] reported failure rates of 50 and 24% for OCA after a mean follow-up of 12.3 years in the PFJ and TF, respectively. Also, the reoperation rate was higher in the PFJ group when compared to the TF group (83 vs. 34%).
In terms of indication for OCA, the senior author distinguishes between chondral lesions affecting the patellar or trochlear articular surface. In the patella, OCA is typically performed after previously failed repair of large chondral lesions over 2 cm2 to provide pain relief and delay arthroplasty in young patients. In the trochlea, OCA can either be a primary treatment option for osteochondral lesions over 2 cm2 or serve as a salvage procedure after failed cartilage repair. Additionally, BMAC augmentation is frequently performed to enhance graft integration [46•, 95•] (Fig. 5).
Particulated Cartilage Procedures
This relatively new treatment option includes particulated articular cartilage using autograft or juvenile allografts (DeNovo, Zimmer, Warsaw, IN) from donors aged 0–13 years [100•]. Analogous to OAT, articular cartilage is harvested from non-weight-bearing areas of the ipsilateral knee for the autograft procedure. Once the cartilage is mechanically minced, it is re-implanted into the chondral lesion and sealed with fibrin glue. A preclinical study demonstrated that particulated autograft loaded on composite scaffold produced hyaline-like cartilage [101]; one clinical study showed encouraging results for addressing lesions on the femoral condyle and trochlea [102].
Particulated juvenile allograft is mechanically minced into 1–2 mm pieces and stored in vials containing enough material to cover lesions up to 2.5 cm2. Similar to autologous particulated cartilage, the chondral lesion is filled with particulated allograft up to 1 mm below the surrounding shoulders of healthy cartilage and finally secured with fibrin glue (Fig. 6). Indications include focal chondral lesions between 1 and 6 cm2 and ICRS grade 3 or higher in patients preferably younger than 55 years and a BMI less than 35 kg/m2 [100•].
There is a limited body of literature reporting clinical outcomes for particulated juvenile allograft transplantation. However, several authors demonstrated favorable results in patients with focal chondral lesions on the patella and trochlea [44•, 45•, 103], with good to excellent defect fill in short and mid-term results [45•, 104•]. Particulated juvenile articular cartilage has also been found to produce a mixture of hyaline and fibrocartilage with a dominance of type II collagen after 2 years follow-up [45•] (Table 2).
Postoperative Rehabilitation
Postoperative protocols differ between institutions and remain a topic of great discussion. Although a standard postoperative rehabilitation protocol for PFJ cartilage repair is presented, each case should be carefully evaluated and the protocol adjusted as needed.
Generally, we recommend cryotherapy, elevation, and a brace for pain control during the immediate postoperative period. After 2 or 3 days, weight-bearing as tolerated is allowed in a locked brace, and continuous progressive passive motion is started. Range of motion (ROM) is encouraged to prevent arthrofibrosis with no restrictions. Therefore, with assist of continuous passive motion (CPM), we advance ROM gain to 90° of flexion as fast as patients tolerate it, at least 5° a day. In case of concomitant TTO, partial weight-bearing is recommended for 4–6 weeks. Return to sports is not advisable until 6 to 12 months after surgery based on senior author’s experience. There are no differences on the protocol for patellar or trochlear lesions.
Conclusion
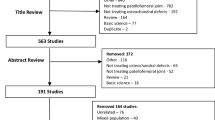
Cartilage repair in the PFJ has demonstrated increasingly good outcomes in patients with patellofemoral cartilage defects after conservative treatment has failed. The algorithm presented in Fig. 7
intends to serve as a simplified guide for the surgical management of chondral lesions in the PFJ. It is of utmost importance to discuss with the patient current functional limitations in sports and activities of daily living, to elucidate the patient’s goals and expectations, and to go over the rehabilitation and recovery time. Unrealistic expectations are common and will lead to disappointment. Careful evaluation of the knee and lower extremity through physical examination and imaging studies is crucial. This will allow planning a comprehensive treatment approach for the cartilage repair procedure, as well as any additional pathology that needs to be addressed in a staged or concomitant fashion.
The anatomic complexity and variability of the PFJ is a great challenge to all cartilage procedures. The increased attention to, and correction of, pathologic co-morbidities such as patellar instability and maltracking has led to a substantial improvement in results. While early outcomes of cartilage repair in the PFJ were disappointing, current comprehensive treatment approaches demonstrate outcomes that are comparable or only slightly inferior to cartilage repair in the TF.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bedi A, Feeley BT, Williams RJ 3rd. Management of articular cartilage defects of the knee. J Bone Joint Surg Am. 2010;92(4):994–1009. https://doi.org/10.2106/JBJS.I.00895.
Bitton R. The economic burden of osteoarthritis. Am J Manag Care. 2009;15(8 Suppl):S230–5.
Duncan RC, Hay EM, Saklatvala J, Croft PR. Prevalence of radiographic osteoarthritis—it all depends on your point of view. Rheumatology (Oxford). 2006;45(6):757–60. https://doi.org/10.1093/rheumatology/kei270.
• Hart HF, Stefanik JJ, Wyndow N, Machotka Z, Crossley KM. The prevalence of radiographic and MRI-defined patellofemoral osteoarthritis and structural pathology: a systematic review and meta-analysis. Br J Sports Med. 2017;51(16):1195–208. https://doi.org/10.1136/bjsports-2017-097515. This is new meta-analysis showing the extensive patellofemoral OA incidence.
Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P. Does isolated patellofemoral osteoarthritis matter? Osteoarthr Cartil. 2009;17(9):1151–5. https://doi.org/10.1016/j.joca.2009.03.016.
Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19(7):717–21.
•• Gomoll AH, Gillogly SD, Cole BJ, Farr J, Arnold R, Hussey K, et al. Autologous chondrocyte implantation in the patella: a multicenter experience. Am J Sports Med. 2014;42(5):1074–81. https://doi.org/10.1177/0363546514523927. This is a multicenter study showing good ACI outcomes for the PFJ and its applicability on bipolar lesions.
Strauss EJ, Galos DK. The evaluation and management of cartilage lesions affecting the patellofemoral joint. Curr Rev Musculoskelet Med. 2013;6(2):141–9. https://doi.org/10.1007/s12178-013-9157-z.
Strauss EJ, Fonseca LE, Shah MR, Yorum T. Management of focal cartilage defects in the knee—is ACI the answer? Bull NYU Hosp Jt Dis. 2011;69(1):63–72.
Chiu JK, Wong YM, Yung PS, Ng GY. The effects of quadriceps strengthening on pain, function, and patellofemoral joint contact area in persons with patellofemoral pain. Am J Phys Med Rehabil. 2012;91(2):98–106. https://doi.org/10.1097/PHM.0b013e318228c505.
Werner S. Anterior knee pain: an update of physical therapy. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2286–94. https://doi.org/10.1007/s00167-014-3150-y.
Mosier BA, Arendt EA, Dahm DL, Dejour D, Gomoll AH. Management of patellofemoral arthritis: from cartilage restoration to arthroplasty. Instr Course Lect. 2017;66:531–42.
Fulkerson JP. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res. 1983;(177):176-81.
Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18(5):490–6; discussion 6-7. https://doi.org/10.1177/036354659001800508.
• Sherman SL, Erickson BJ, Cvetanovich GL, Chalmers PN, Farr J 2nd, Bach BR Jr, et al. Tibial tuberosity osteotomy: indications, techniques, and outcomes. Am J Sports Med. 2014;42(8):2006–17. https://doi.org/10.1177/0363546513507423. This study is a recent review of TTO procedure
Pascual-Garrido C, Slabaugh MA, L'Heureux DR, Friel NA, Cole BJ. Recommendations and treatment outcomes for patellofemoral articular cartilage defects with autologous chondrocyte implantation: prospective evaluation at average 4-year follow-up. Am J Sports Med. 2009;37(Suppl 1):33S–41S. https://doi.org/10.1177/0363546509349605.
Henderson IJ, Lavigne P. Periosteal autologous chondrocyte implantation for patellar chondral defect in patients with normal and abnormal patellar tracking. Knee. 2006;13(4):274–9. https://doi.org/10.1016/j.knee.2006.04.006.
Farr J. Autologous chondrocyte implantation improves patellofemoral cartilage treatment outcomes. Clin Orthop Relat Res. 2007;463:187–94.
Trinh TQ, Harris JD, Siston RA, Flanigan DC. Improved outcomes with combined autologous chondrocyte implantation and patellofemoral osteotomy versus isolated autologous chondrocyte implantation. Arthroscopy. 2013;29(3):566–74. https://doi.org/10.1016/j.arthro.2012.10.008.
•• Ebert JR, Schneider A, Fallon M, Wood DJ, Janes GCA. Comparison of 2-year outcomes in patients undergoing tibiofemoral or patellofemoral matrix-induced autologous chondrocyte implantation. Am J Sports Med. 2017:363546517724761. https://doi.org/10.1177/0363546517724761. This study shows the importance of maltracking correction for ACI improved outcomes in the PFJ.
•• von Keudell A, Han R, Bryant T, Minas T. Autologous chondrocyte implantation to isolated patella cartilage defects. Cartilage. 2017;8(2):146–54. https://doi.org/10.1177/1947603516654944. Recent study showing good long-term outcomes after patellar ACI.
•• Andriolo L, Merli G, Filardo G, Marcacci M, Kon E. Failure of autologous chondrocyte implantation. Sports Med Arthrosc. 2017;25(1):10–8. https://doi.org/10.1097/JSA.0000000000000137. This systematic review shows an ACI overall failure rate of 14.5%.
• Schuette HB, Kraeutler MJ, McCarty EC. Matrix-assisted autologous chondrocyte transplantation in the knee: a systematic review of mid- to long-term clinical outcomes. Orthop J Sports Med. 2017;5(6):2325967117709250. https://doi.org/10.1177/2325967117709250. This systematic review compares the MACI failure rates of PFJ and TFJ.
Montgomery SR, Foster BD, Ngo SS, Terrell RD, Wang JC, Petrigliano FA, et al. Trends in the surgical treatment of articular cartilage defects of the knee in the United States. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2070–5. https://doi.org/10.1007/s00167-013-2614-9.
Grieshober JA, Stanton M, Gambardella R. Debridement of articular cartilage: the natural course. Sports Med Arthrosc. 2016;24(2):56–62. https://doi.org/10.1097/JSA.0000000000000108.
Kaplan LD, Chu CR, Bradley JP, Fu FH, Studer RK. Recovery of chondrocyte metabolic activity after thermal exposure. Am J Sports Med. 2003;31(3):392–8. https://doi.org/10.1177/03635465030310031101.
Lotto ML, Wright EJ, Appleby D, Zelicof SB, Lemos MJ, Lubowitz JH. Ex vivo comparison of mechanical versus thermal chondroplasty: assessment of tissue effect at the surgical endpoint. Arthroscopy. 2008;24(4):410–5. https://doi.org/10.1016/j.arthro.2007.09.018.
Kosy JD, Schranz PJ, Toms AD, Eyres KS, Mandalia VI. The use of radiofrequency energy for arthroscopic chondroplasty in the knee. Arthroscopy. 2011;27(5):695–703. https://doi.org/10.1016/j.arthro.2010.11.058.
Rocco P, Lorenzo DB, Guglielmo T, Michele P, Nicola M, Vincenzo D. Radiofrequency energy in the arthroscopic treatment of knee chondral lesions: a systematic review. Br Med Bull. 2016;117(1):149–56. https://doi.org/10.1093/bmb/ldw004.
Spahn G, Hofmann GO, von Engelhardt LV. Mechanical debridement versus radiofrequency in knee chondroplasty with concomitant medial meniscectomy: 10-year results from a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1560–8. https://doi.org/10.1007/s00167-015-3810-6.
Galloway MT, Noyes FR. Cystic degeneration of the patella after arthroscopic chondroplasty and subchondral bone perforation. Arthroscopy. 1992;8(3):366–9.
• Anderson DE, Rose MB, Wille AJ, Wiedrick J, Crawford DC. Arthroscopic mechanical chondroplasty of the knee is beneficial for treatment of focal cartilage lesions in the absence of concurrent pathology. Orthop J Sports Med. 2017;5(5):2325967117707213. https://doi.org/10.1177/2325967117707213. This study assess factors related with chondroplasty improved outcomes.
Federico DJ, Reider B. Results of isolated patellar debridement for patellofemoral pain in patients with normal patellar alignment. Am J Sports Med. 1997;25(5):663–9. https://doi.org/10.1177/036354659702500513.
Steadman JR, Rodkey WG, Rodrigo JJ. Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. 2001;(391 Suppl):S362–9.
Steadman JR, Rodkey WG, Briggs KK. Microfracture to treat full-thickness chondral defects: surgical technique, rehabilitation, and outcomes. J Knee Surg. 2002;15(3):170–6.
Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37(10):2053–63. https://doi.org/10.1177/0363546508328414.
Kreuz PC, Steinwachs MR, Erggelet C, Krause SJ, Konrad G, Uhl M, et al. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthr Cartil. 2006;14(11):1119–25. https://doi.org/10.1016/j.joca.2006.05.003.
Minas T, Gomoll AH, Rosenberger R, Royce RO, Bryant T. Increased failure rate of autologous chondrocyte implantation after previous treatment with marrow stimulation techniques. Am J Sports Med. 2009;37(5):902–8. https://doi.org/10.1177/0363546508330137.
• Baltzer AW, Ostapczuk MS, Terheiden HP, Merk HR. Good short- to medium-term results after osteochondral autograft transplantation (OAT) in middle-aged patients with focal, non-traumatic osteochondral lesions of the knee. Orthop Traumatol Surg Res. 2016;102(7):879–84. https://doi.org/10.1016/j.otsr.2016.06.004. This study shows that patellar OAT improved outcomes are associated with a poor preoperative WOMAC.
•• Astur DC, Arliani GG, Binz M, Astur N, Kaleka CC, Amaro JT, et al. Autologous osteochondral transplantation for treating patellar chondral injuries: evaluation, treatment, and outcomes of a two-year follow-up study. J Bone Joint Surg Am. 2014;96(10):816–23. https://doi.org/10.2106/JBJS.M.00312. Recent study with a larger sample than previous OAT studies for patellar defects. Shows good outcomes in the first two years of follow up for lesions smaller than 2.5 cm2.
•• Gracitelli GC, Meric G, Pulido PA, Gortz S, De Young AJ, Bugbee WD. Fresh osteochondral allograft transplantation for isolated patellar cartilage injury. Am J Sports Med. 2015;43(4):879–84. https://doi.org/10.1177/0363546514564144. This study demonstrates good outcomes for patellar OCA
•• Cameron JI, Pulido PA, McCauley JC, Bugbee WD. Osteochondral allograft transplantation of the femoral trochlea. Am J Sports Med. 2016;44(3):633–8. https://doi.org/10.1177/0363546515620193. This study demonstrates good outcomes for trochlear OCA.
• Meric G, Gracitelli GC, Gortz S, De Young AJ, Bugbee WD. Fresh osteochondral allograft transplantation for bipolar reciprocal osteochondral lesions of the knee. Am J Sports Med. 2015;43(3):709–14. https://doi.org/10.1177/0363546514562549. This study shows that OCA is a useful salvage treatment option for reciprocal bipolar cartilage lesions of the knee. High reoperation and failure rates were observed.
• Buckwalter JA, Bowman GN, Albright JP, Wolf BR, Bollier M. Clinical outcomes of patellar chondral lesions treated with juvenile particulated cartilage allografts. Iowa Orthop J. 2014;34:44–9. This study demonstrates good functional outcomes of particulated juvenile allograft.
• Farr J, Tabet SK, Margerrison E, Cole BJ. Clinical, radiographic, and histological outcomes after cartilage repair with Particulated juvenile articular cartilage: a 2-year prospective study. Am J Sports Med. 2014;42(6):1417–25. https://doi.org/10.1177/0363546514528671. This study demonstrates good short-term outcomes of particulated juvenile allograft.
• Moatshe G, Morris ER, Cinque ME, Pascual-Garrido C, Chahla J, Engebretsen L, et al. Biological treatment of the knee with platelet-rich plasma or bone marrow aspirate concentrates. Acta Orthop. 2017:1–5. https://doi.org/10.1080/17453674.2017.1368899. This review presents the literature on the most commonly employed biologic agents for the different knee.
Holton J, Imam M, Ward J, Snow M. The basic science of bone marrow aspirate concentrate in chondral injuries. Orthop Rev (Pavia). 2016;8(3):6659. https://doi.org/10.4081/or.2016.6659.
Welch T, Mandelbaum B, Tom M. Autologous chondrocyte implantation: past, present, and future. Sports Med Arthrosc. 2016;24(2):85–91. https://doi.org/10.1097/JSA.0000000000000115.
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331(14):889–95. https://doi.org/10.1056/NEJM199410063311401.
Jungmann PM, Salzmann GM, Schmal H, Pestka JM, Sudkamp NP, Niemeyer P. Autologous chondrocyte implantation for treatment of cartilage defects of the knee: what predicts the need for reintervention? Am J Sports Med. 2012;40(1):58–67. https://doi.org/10.1177/0363546511423522.
Niemeyer P, Salzmann G, Feucht M, Pestka J, Porichis S, Ogon P, et al. First-generation versus second-generation autologous chondrocyte implantation for treatment of cartilage defects of the knee: a matched-pair analysis on long-term clinical outcome. Int Orthop. 2014;38(10):2065–70. https://doi.org/10.1007/s00264-014-2368-0.
Filardo G, Kon E, Roffi A, Di Martino A, Marcacci M. Scaffold-based repair for cartilage healing: a systematic review and technical note. Arthroscopy. 2013;29(1):174–86. https://doi.org/10.1016/j.arthro.2012.05.891.
•• Hinckel BB, Gomoll AH. Autologous chondrocytes and next-generation matrix-based autologous chondrocyte implantation. Clin Sports Med. 2017;36(3):525–48. https://doi.org/10.1016/j.csm.2017.02.008. This study discusses MACI's technique and outcomes.
Niemeyer P, Lenz P, Kreuz PC, Salzmann GM, Sudkamp NP, Schmal H, et al. Chondrocyte-seeded type I/III collagen membrane for autologous chondrocyte transplantation: prospective 2-year results in patients with cartilage defects of the knee joint. Arthroscopy. 2010;26(8):1074–82. https://doi.org/10.1016/j.arthro.2009.12.028.
• Gille J, Behrens P, Schulz AP, Oheim R, Kienast B. Matrix-associated autologous chondrocyte implantation: a clinical follow-up at 15 years. Cartilage. 2016;7(4):309–15. https://doi.org/10.1177/1947603516638901. MACI long-term follow-up study shows improved results in functional scores.
Gomoll AH, Ambra LF, Phan A, Mastrocola M, Shah N. Cell-seeded autologous chondrocyte implantation: a simplified implantation technique that maintains high clinical outcomes. Am J Sports Med. 2017;45(5):1028–36. https://doi.org/10.1177/0363546516681000.
Duif C, Koutah MA, Ackermann O, Spyrou G, von Engelhardt LV, Kaya D, et al. Combination of autologous chondrocyte implantation (ACI) and osteochondral autograft transfer system (OATS) for surgical repair of larger cartilage defects of the knee joint. A review illustrated by a case report. Technol Health Care. 2015;23(5):531–7. https://doi.org/10.3233/THC-151003.
Minas T, Gomoll AH, Solhpour S, Rosenberger R, Probst C, Bryant T. Autologous chondrocyte implantation for joint preservation in patients with early osteoarthritis. Clin Orthop Relat Res. 2010;468(1):147–57. https://doi.org/10.1007/s11999-009-0998-0.
•• Minas T, Von Keudell A, Bryant T, Gomoll AH. The John Insall award: a minimum 10-year outcome study of autologous chondrocyte implantation. Clin Orthop Relat Res. 2014;472(1):41–51. https://doi.org/10.1007/s11999-013-3146-9. Study with a large sample showing good outcomes for ACI with a long follow up and factors related to inferior outcomes.
Ossendorf C, Steinwachs MR, Kreuz PC, Osterhoff G, Lahm A, Ducommun PP, et al. Autologous chondrocyte implantation (ACI) for the treatment of large and complex cartilage lesions of the knee. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:11. https://doi.org/10.1186/1758-2555-3-11.
Minas T, Bryant T. The role of autologous chondrocyte implantation in the patellofemoral joint. Clin Orthop Relat Res. 2005;(436):30–9.
Mandelbaum B, Browne JE, Fu F, Micheli LJ, Moseley JB Jr, Erggelet C, et al. Treatment outcomes of autologous chondrocyte implantation for full-thickness articular cartilage defects of the trochlea. Am J Sports Med. 2007;35(6):915–21. https://doi.org/10.1177/0363546507299528.
Gobbi A, Kon E, Berruto M, Filardo G, Delcogliano M, Boldrini L, et al. Patellofemoral full-thickness chondral defects treated with second-generation autologous chondrocyte implantation: results at 5 years’ follow-up. Am J Sports Med. 2009;37(6):1083–92. https://doi.org/10.1177/0363546509331419.
Vanlauwe JJ, Claes T, Van Assche D, Bellemans J, Luyten FP. Characterized chondrocyte implantation in the patellofemoral joint: an up to 4-year follow-up of a prospective cohort of 38 patients. Am J Sports Med. 2012;40(8):1799–807. https://doi.org/10.1177/0363546512452712.
• Filardo G, Kon E, Andriolo L, Di Martino A, Zaffagnini S, Marcacci M. Treatment of “patellofemoral” cartilage lesions with matrix-assisted autologous chondrocyte transplantation: a comparison of patellar and trochlear lesions. Am J Sports Med. 2014;42(3):626–34. https://doi.org/10.1177/0363546513510884. This study shows superior outcomes after MACI for patellar lesions when compared to trochlear lesions.
Nawaz SZ, Bentley G, Briggs TW, Carrington RW, Skinner JA, Gallagher KR, et al. Autologous chondrocyte implantation in the knee: mid-term to long-term results. J Bone Joint Surg Am. 2014;96(10):824–30. https://doi.org/10.2106/JBJS.L.01695.
• Gillogly SD, Arnold RM. Autologous chondrocyte implantation and anteromedialization for isolated patellar articular cartilage lesions: 5- to 11-year follow-up. Am J Sports Med. 2014;42(4):912–20. https://doi.org/10.1177/0363546513519077. This study demonstrates good outcomes with patellar ACI associated with TTO.
Peterson L, Minas T, Brittberg M, Lindahl A. Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: results at two to ten years. J Bone Joint Surg Am. 2003;85-A(Suppl 2):17–24.
Vijayan S, Bartlett W, Bentley G, Carrington RW, Skinner JA, Pollock RC, et al. Autologous chondrocyte implantation for osteochondral lesions in the knee using a bilayer collagen membrane and bone graft: a two- to eight-year follow-up study. J Bone Joint Surg Br. 2012;94(4):488–92. https://doi.org/10.1302/0301-620X.94B4.27117.
• Ebert JR, Fallon M, Wood DJ, Prospective Clinical JGCA. Radiological evaluation at 5 years after arthroscopic matrix-induced autologous chondrocyte implantation. Am J Sports Med. 2017;45(1):59–69. https://doi.org/10.1177/0363546516663493. This study shows good outcomes after arthroscopic ACI.
• Biant LC, Simons M, Gillespie T, McNicholas MJ. Cell viability in arthroscopic versus open autologous chondrocyte implantation. Am J Sports Med. 2017;45(1):77–81. https://doi.org/10.1177/0363546516664338. This study demonstrates that chondrocyte viability remains a problem for arthroscopic ACI.
Pareek A, Carey JL, Reardon PJ, Peterson L, Stuart MJ, Krych AJ. Long-term outcomes after autologous chondrocyte implantation: a systematic review at mean follow-up of 11.4 years. Cartilage. 2016;7(4):298–308. https://doi.org/10.1177/1947603516630786.
• Mistry H, Connock M, Pink J, Shyangdan D, Clar C, Royle P, et al. Autologous chondrocyte implantation in the knee: systematic review and economic evaluation. Health Technol Assess. 2017;21(6):1–294. https://doi.org/10.3310/hta21060. This study shows that ACI cost effectiveness is comparable to other procedures.
• Ogura T, Mosier BA, Bryant T, Minas T. A 20-year follow-up after first-generation autologous chondrocyte implantation. Am J Sports Med. 2017;45(12):2751–61. https://doi.org/10.1177/0363546517716631. This study demonstrates a survival rate of 63%. for the first-generation ACI after 20 years.
Ambra LF, de Girolamo L, Mosier B, Gomoll AH. Review: interventions for cartilage disease: current state-of-the-art and emerging technologies. Arthritis Rheumatol. 2017;69(7):1363–73. https://doi.org/10.1002/art.40094.
Garretson RB 3rd, Katolik LI, Verma N, Beck PR, Bach BR, Cole BJ. Contact pressure at osteochondral donor sites in the patellofemoral joint. Am J Sports Med. 2004;32(4):967–74.
McCoy B, Miniaci A. Osteochondral autograft transplantation/mosaicplasty. J Knee Surg. 2012;25(2):99–108.
Nakagawa Y, Suzuki T, Kuroki H, Kobayashi M, Okamoto Y, Nakamura T. The effect of surface incongruity of grafted plugs in osteochondral grafting: a report of five cases. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):591–6. https://doi.org/10.1007/s00167-006-0253-0.
• Yabumoto H, Nakagawa Y, Mukai S, Saji T. Osteochondral autograft transplantation for isolated patellofemoral osteoarthritis. Knee. 2017;24:1498–503. https://doi.org/10.1016/j.knee.2017.07.016. This study shows the importance of an accurate graft implantation for improved OAT outcomes in the PFJ.
Gomoll AH, Minas T, Farr J, Cole BJ. Treatment of chondral defects in the patellofemoral joint. J Knee Surg. 2006;19(4):285–95.
Hangody L, Rathonyi GK, Duska Z, Vasarhelyi G, Fules P, Modis L. Autologous osteochondral mosaicplasty. Surgical technique. J Bone Joint Surg Am. 2004;86-A(Suppl 1):65–72.
Bentley G, Biant LC, Carrington RW, Akmal M, Goldberg A, Williams AM, et al. A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br. 2003;85(2):223–30.
Zouzias IC, Bugbee WD. Osteochondral allograft transplantation in the knee. Sports Med Arthrosc. 2016;24(2):79–84. https://doi.org/10.1097/JSA.0000000000000109.
Determann JR, Fleischli JE, D'Alessandro DF, Piasecki DP. Patellofemoral osteochondral allografts: can we improve the matching process? J Knee Surg. 2017;30(8):835–41. https://doi.org/10.1055/s-0037-1598107.
McCormick F, Harris JD, Abrams GD, Frank R, Gupta A, Hussey K, et al. Trends in the surgical treatment of articular cartilage lesions in the United States: an analysis of a large private-payer database over a period of 8 years. Arthroscopy. 2014;30(2):222–6. https://doi.org/10.1016/j.arthro.2013.11.001.
Torrie AM, Kesler WW, Elkin J, Gallo RA. Osteochondral allograft. Curr Rev Musculoskelet Med. 2015;8(4):413–22. https://doi.org/10.1007/s12178-015-9298-3.
Nuelle CW, Nuelle JA, Cook JL, Stannard JP. Patient factors, donor age, and graft storage duration affect osteochondral allograft outcomes in knees with or without comorbidities. J Knee Surg. 2017;30(2):179–84. https://doi.org/10.1055/s-0036-1584183.
• Schmidt KJ, Tirico LE, McCauley JC, Bugbee WD. Fresh osteochondral allograft transplantation: is graft storage time associated with clinical outcomes and graft survivorship? Am J Sports Med. 2017;45(10):2260–6. https://doi.org/10.1177/0363546517704846. This study demonstrates that longer period of graft storage appears to be safe.
Tschon M, Veronesi F, Giannini S, Fini M. Fresh osteochondral allotransplants: outcomes, failures and future developments. Injury. 2017;48(7):1287–95. https://doi.org/10.1016/j.injury.2017.05.006.
•• Hunt HE, Sadr K, Deyoung AJ, Gortz S, Bugbee WD. The role of immunologic response in fresh osteochondral allografting of the knee. Am J Sports Med. 2014;42(4):886–91. https://doi.org/10.1177/0363546513518733. This study shows that antibody development is related the graft size on an OCA. However no clinical outcomes differences were found.
Meyer MA, McCarthy MA, Gitelis ME, Poland SG, Urita A, Chubinskaya S, et al. Effectiveness of lavage techniques in removing immunogenic elements from osteochondral allografts. Cartilage. 2017;8(4):369–73. https://doi.org/10.1177/1947603516681132.
Sun Y, Jiang W, Cory E, Caffrey JP, Hsu FH, Chen AC, et al. Pulsed lavage cleansing of osteochondral grafts depends on lavage duration, flow intensity, and graft storage condition. PLoS One. 2017;12(5):e0176934. https://doi.org/10.1371/journal.pone.0176934.
Gracitelli GC, Meric G, Pulido PA, McCauley JC, Bugbee WD. Osteochondral allograft transplantation for knee lesions after failure of cartilage repair surgery. Cartilage. 2015;6(2):98–105. https://doi.org/10.1177/1947603514566298.
Gracitelli GC, Tirico LE, McCauley JC, Pulido PA, Bugbee WD. Fresh osteochondral allograft transplantation for fractures of the knee. Cartilage. 2017;8(2):155–61. https://doi.org/10.1177/1947603516657640.
• Oladeji LO, Stannard JP, Cook CR, Kfuri M, Crist BD, Smith MJ, et al. Effects of autogenous bone marrow aspirate concentrate on radiographic integration of femoral condylar osteochondral allografts. Am J Sports Med. 2017;45(12):2797–803. https://doi.org/10.1177/0363546517715725. This study demonstrates a higher graft integration rate seen on radiographies with the use of BMAC as a biologic augmentation for OCA.
Gracitelli GC, Moraes VY, Franciozi CE, Luzo MV, Belloti JC. Surgical interventions (microfracture, drilling, mosaicplasty, and allograft transplantation) for treating isolated cartilage defects of the knee in adults. Cochrane Database Syst Rev. 2016;9:CD010675. https://doi.org/10.1002/14651858.CD010675.pub2.
Jamali AA, Emmerson BC, Chung C, Convery FR, Bugbee WD. Fresh osteochondral allografts: results in the patellofemoral joint. Clin Orthop Relat Res. 2005;437:176–85.
Torga Spak R, Teitge RA. Fresh osteochondral allografts for patellofemoral arthritis: long-term followup. Clin Orthop Relat Res. 2006;444:193–200. https://doi.org/10.1097/01.blo.0000201152.98830.ed.
• Assenmacher AT, Pareek A, Reardon PJ, Macalena JA, Stuart MJ, Krych AJ. Long-term outcomes after osteochondral allograft: a systematic review at long-term follow-up of 12.3 years. Arthroscopy. 2016;32(10):2160–8. https://doi.org/10.1016/j.arthro.2016.04.020. This is a recent systematic review of long-term OCA outcomes.
• Riboh JC, Cole BJ, Farr J. Particulated articular cartilage for symptomatic chondral defects of the knee. Curr Rev Musculoskelet Med. 2015;8(4):429–35. https://doi.org/10.1007/s12178-015-9300-0. Recent review on particulated cartilage procedures.
Marmotti A, Bruzzone M, Bonasia DE, Castoldi F, Von Degerfeld MM, Bignardi C, et al. Autologous cartilage fragments in a composite scaffold for one stage osteochondral repair in a goat model. Eur Cell Mater. 2013;26:15–31. discussion −2.
Cole BJ, Farr J, Winalski CS, Hosea T, Richmond J, Mandelbaum B, et al. Outcomes after a single-stage procedure for cell-based cartilage repair: a prospective clinical safety trial with 2-year follow-up. Am J Sports Med. 2011;39(6):1170–9. https://doi.org/10.1177/0363546511399382.
Tompkins M, Hamann JC, Diduch DR, Bonner KF, Hart JM, Gwathmey FW, et al. Preliminary results of a novel single-stage cartilage restoration technique: particulated juvenile articular cartilage allograft for chondral defects of the patella. Arthroscopy. 2013;29(10):1661–70. https://doi.org/10.1016/j.arthro.2013.05.021.
• Grawe B, Burge A, Nguyen J, Strickland S, Warren R, Rodeo S, et al. Cartilage regeneration in full-thickness patellar chondral defects treated with Particulated juvenile articular allograft cartilage: an MRI analysis. Cartilage. 2017;8(4):374–83. https://doi.org/10.1177/1947603517710308. This recent study demonstrates good particulated juvenile allograft integration on MRI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Andreas H. Gomoll reports grants from JRF during the conduct of study and personal fees from NUTECH outside of the submitted work.
Alexandre Barbieri Mestriner and Jakob Ackermann declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the topical collection on Advances in Patellofemoral Surgery
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mestriner, A.B., Ackermann, J. & Gomoll, A.H. Patellofemoral Cartilage Repair. Curr Rev Musculoskelet Med 11, 188–200 (2018). https://doi.org/10.1007/s12178-018-9474-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-018-9474-3