Abstract
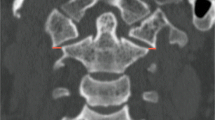
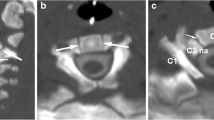
Fractures of the second cervical vertebra (C2, axis) are common in adult spine surgery. Those fractures occurring in younger adult patients are often associated with high-energy mechanism trauma, resulting in a “Hangman’s Fracture.” Management of these fractures is often successful with nonoperative means, though surgery may be needed in those fractures with greater displacement and injury to the C2-C3 disc. Older patients are more likely to sustain fractures of the odontoid process. The evidence supporting surgical management of these fractures is evolving, as there may be a mortality benefit to surgery. Regardless of treatment, longer-term mortality rates are high in this patient population, which should be discussed with the patient and family at the time of injury. Pediatric patients may suffer fractures of the axis, though differentiation of normal and pathologic findings is necessary and more difficult with the skeletally immature spine.








Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;23:38–40.
Lui TN, Lee ST, Wong CW, et al. C1-C2 fracture-dislocations in children and adolescents. J Trauma. 1996;40:408–11.
Platzer P, Jaindl M, Thalhammer G, et al. Cervical spine injuries in pediatric patients. J Trauma. 2007;62:389–96. discussion 94-6.
Viccellio P, Simon H, Pressman BD, et al. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108, E20.
Avellino AM, Mann FA, Grady MS, et al. The misdiagnosis of acute cervical spine injuries and fractures in infants and children: the 12-year experience of a level I pediatric and adult trauma center. Childs Nerv Syst. 2005;21:122–7.
Pieretti-Vanmarcke R, Velmahos GC, Nance ML, et al. Clinical clearance of the cervical spine in blunt trauma patients younger than 3 years: a multi-center study of the American Association for the Surgery of Trauma. J Trauma. 2009;67:543–9. discussion 9-50.
Lustrin ES, Karakas SP, Ortiz AO, et al. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003;23:539–60.
Sherk HH, Nicholson JT, Chung SM. Fractures of the odontoid process in young children. J Bone Joint Surg Am. 1978;60:921–4.
Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–74.
Barker L, Anderson J, Chesnut R, Nesbit G, Tjauw T, Hart R. Reliability and reproducibility of dens fracture classification with use of plain radiography and reformatted computer-aided tomography. J Bone Joint Surg Am. 2006;88:106–12.
Pearson AM, Martin BI, Lindsey M, Mirza SK. C2 vertebral fractures in the medicare population: incidence, outcomes, and costs. J Bone Joint Surg Am. 2016;98:449–56. C2 Fracture incidence is rising, though rate of surgery remains steady. There may be a mortality benefit to surgery in the Medicare population.
Smith HE, Kerr SM, Fehlings MG, et al. Trends in epidemiology and management of type II odontoid fractures: 20-year experience at a model system spine injury tertiary referral center. J Spinal Disord Tech. 2010;23:501–5.
Chapman J, Smith JS, Kopjar B, et al. The AOSpine North America Geriatric Odontoid Fracture Mortality Study: a retrospective review of mortality outcomes for operative versus nonoperative treatment of 322 patients with long-term follow-up. Spine (Phila Pa 1976). 2013;38:1098–104. A retrospective cohort study examining mortality after geriatric odontoid fractures. At maximum follow-up, there is some evidence to support a mortality benefit to surgery over nonoperative treatment.
Fehlings MG, Arun R, Vaccaro AR, Arnold PM, Chapman JR, Kopjar B. Predictors of treatment outcomes in geriatric patients with odontoid fractures: AOSpine North America multi-centre prospective GOF study. Spine (Phila Pa 1976). 2013;38:881–6. A prospective study of geriatric odontoid fractures found improved patient reported outcomes for younger patients and those treated with surgery at their initial hospitalization.
Bransford RJ, Stevens DW, Uyeji S, Bellabarba C, Chapman JR. Halo vest treatment of cervical spine injuries: a success and survivorship analysis. Spine (Phila Pa 1976). 2009;34:1561–6.
Longo UG, Denaro L, Campi S, Maffulli N, Denaro V. Upper cervical spine injuries: indications and limits of the conservative management in Halo vest. A systematic review of efficacy and safety. Injury. 2010;41:1127–35.
Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59:350–6. discussion 6-8.
Polin RS, Szabo T, Bogaev CA, Replogle RE, Jane JA. Nonoperative management of Types II and III odontoid fractures: the Philadelphia collar versus the halo vest. Neurosurgery. 1996;38:450–6. discussion 6-7.
Smith HE, Kerr SM, Maltenfort M, et al. Early complications of surgical versus conservative treatment of isolated type II odontoid fractures in octogenarians: a retrospective cohort study. J Spinal Disord Tech. 2008;21:535–9.
Patel A, Zakaria R, Al-Mahfoudh R, et al. Conservative management of type II and III odontoid fractures in the elderly at a regional spine centre: a prospective and retrospective cohort study. Br J Neurosurg. 2015;29:249–53.
Koech F, Ackland HM, Varma DK, Williamson OD, Malham GM. Nonoperative management of type II odontoid fractures in the elderly. Spine (Phila Pa 1976). 2008;33:2881–6.
Smith JS, Kepler CK, Kopjar B, et al. Effect of type II odontoid fracture nonunion on outcome among elderly patients treated without surgery: based on the AOSpine North America geriatric odontoid fracture study. Spine (Phila Pa 1976). 2013;38:2240–6. Odontoid nonunions may be treated effectively, without an adverse effect on patient reported outcomes. However, the majority of patients sustaining a nonunion underwent delayed surgery.
Bachs A, Barraquer-Bordas L, Barraquer-Ferre L, Canadell JM, Modolell A. Delayed myelopathy following atlanto-axial dislocation by separated odontoid process. Brain. 1955;78:537–53.
Kirankumar MV, Behari S, Salunke P, Banerji D, Chhabra DK, Jain VK. Surgical management of remote, isolated type II odontoid fractures with atlantoaxial dislocation causing cervical compressive myelopathy. Neurosurgery. 2005;56:1004–12. discussion -12.
Shamji MF, Alotaibi N, Ghare A, Fehlings MG. Chronic hypertrophic nonunion of the Type II odontoid fracture causing cervical myelopathy: case report and review of literature. Surg Neurol Int. 2016;7:S53–6.
Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93:227–36.
Platzer P, Thalhammer G, Ostermann R, Wieland T, Vecsei V, Gaebler C. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine (Phila Pa 1976). 2007;32:1714–20.
Joaquim AF, Patel AA. Surgical treatment of Type II odontoid fractures: anterior odontoid screw fixation or posterior cervical instrumented fusion? Neurosurg Focus. 2015;38, E11.
Wright NM. Translaminar rigid screw fixation of the axis. Technical note. J Neurosurg Spine. 2005;3:409–14.
Claybrooks R, Kayanja M, Milks R, Benzel E. Atlantoaxial fusion: a biomechanical analysis of two C1-C2 fusion techniques. Spine J. 2007;7:682–8.
Schoenfeld AJ, Bono CM, Reichmann WM, et al. Type II odontoid fractures of the cervical spine: do treatment type and medical comorbidities affect mortality in elderly patients? Spine (Phila Pa 1976). 2011;36:879–85.
Woods BI, Hohl JB, Braly B, Donaldson 3rd W, Kang J, Lee JY. Mortality in elderly patients following operative and nonoperative management of odontoid fractures. J Spinal Disord Tech. 2014;27:321–6. Geriatric patients sustaining an odontoid fracture have 1- and 5-year mortality, regardless of surgical or nonoperative management.
Fagin AM, Cipolle MD, Barraco RD, et al. Odontoid fractures in the elderly: should we operate? J Trauma. 2010;68:583–6.
Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg (Br). 1981;63-B:319–27.
Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985;67:217–26.
Starr JK, Eismont FJ. Atypical Hangman’s fractures. Spine (Phila Pa 1976). 1993;18:1954–7.
Muller EJ, Wick M, Muhr G. Traumatic spondylolisthesis of the axis: treatment rationale based on the stability of the different fracture types. Eur Spine J. 2000;9:123–8.
Coric D, Wilson JA, Kelly Jr DL. Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg. 1996;85:550–4.
Govender S, Charles RW. Traumatic spondylolisthesis of the axis. Injury. 1987;18:333–5.
Grady MS, Howard MA, Jane JA, Persing JA. Use of the Philadelphia collar as an alternative to the halo vest in patients with C-2, C-3 fractures. Neurosurgery. 1986;18:151–6.
Suchomel P, Hradil J, Barsa P, et al. [Surgical treatment of fracture of the ring of axis—“hangman’s fracture”]. Acta Chir Orthop Traumatol Cech. 2006;73:321–8.
Vaccaro AR, Madigan L, Bauerle WB, Blescia A, Cotler JM. Early halo immobilization of displaced traumatic spondylolisthesis of the axis. Spine (Phila Pa 1976). 2002;27:2229–33.
Chittiboina P, Wylen E, Ogden A, Mukherjee DP, Vannemreddy P, Nanda A. Traumatic spondylolisthesis of the axis: a biomechanical comparison of clinically relevant anterior and posterior fusion techniques. J Neurosurg Spine. 2009;11:379–87.
Duggal N, Chamberlain RH, Perez-Garza LE, Espinoza-Larios A, Sonntag VK, Crawford NR. Hangman’s fracture: a biomechanical comparison of stabilization techniques. Spine (Phila Pa 1976). 2007;32:182–7.
Schleicher P, Scholz M, Pingel A, Kandziora F. Traumatic spondylolisthesis of the axis vertebra in adults. Global Spine J. 2015;5:346–58.
Buchholz AL, Morgan SL, Robinson LC, Frankel BM. Minimally invasive percutaneous screw fixation of traumatic spondylolisthesis of the axis. J Neurosurg Spine. 2015;22:459–65.
Ryken TC, Hadley MN, Aarabi B, et al. Management of isolated fractures of the axis in adults. Neurosurgery. 2013;72 Suppl 2:132–50.
McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994;19:1741–4.
Ding T, Maltenfort M, Yang H, et al. Correlation of C2 fractures and vertebral artery injury. Spine (Phila Pa 1976). 2010;35:E520–4.
Durand D, Wu X, Kalra VB, Abbed KM, Malhotra A. Predictors of vertebral artery injury in isolated C2 fractures based on fracture morphology using CT angiography. Spine (Phila Pa 1976). 2015;40:E713–8. Fracture communition and involvement of the foramen transversarium are associated with vertebral artery injuries at the level of C2. Angiography may be indicated in patients with these fracture findings on plain computed tomography.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Megan E. Gornet declares that she has no conflict of interest.
Michael P. Kelly reports grants paid directly to his institution from the Cervical Spine Research Society, AO Spine, Barnes Jewish Foundation, Fox Family Foundation, Orthopedic Research Education Foundation, Cerapedics, and PCORI, outside the submitted work.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cervical Injuries and Treatment
Rights and permissions
About this article
Cite this article
Gornet, M.E., Kelly, M.P. Fractures of the axis: a review of pediatric, adult, and geriatric injuries. Curr Rev Musculoskelet Med 9, 505–512 (2016). https://doi.org/10.1007/s12178-016-9368-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-016-9368-1