Abstract
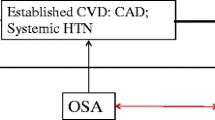
The inter-relationships of sleep disordered breathing (SDB) and heart failure (HF) are becoming increasingly well-characterized. The pathways linking the 2 entities are likely bidirectional and key underlying pathophysiological mechanisms at play include autonomic nervous system fluctuations, intermittent hypoxia, intrathoracic cardiac mechanical influences, rostral fluid shifts and upregulation of systemic inflammation and oxidative stress. Given the increased morbidity and mortality which accompanies heart failure, the recognition and treatment of factors such as sleep disordered breathing is paramount in order to mitigate these untoward downstream health consequences. Recently, the management of HF requires combining several treatments including pharmacotherapy, electrophysiologic therapy, and cardiac surgery to target the various complex facets of HF. Despite the development of HF treatments, HF remains to pose a great challenge to the general cardiologist. Herein we review several interventional studies highlighting the effects of treating SDB on HF morbidity and mortality with a notable predominance of literature focusing on HF reduced ejection fraction (HF-REF) as well as emerging data describing SDB treatment effects in HF preserved EF (HF-PEF). These data are compelling yet with intrinsic limitations, which underscore the need for appropriately powered clinical trials employing rigorous clinical trials methodology to examine the effect of SDB treatment on HF progression and associated adverse outcomes.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Lloyd-Jones D, Adams RJ, Brown TM, Writing Group M; American Heart Association Statistics C, Stroke Statistics S, et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–215.
Gandhi PU, Pinney S. Management of chronic heart failure: biomarkers, monitors, and disease management programs. Ann Global Health. 2014;80:46–54.
Heidenreich PA, Zhao X, Hernandez AF, et al. Patient and hospital characteristics associated with traditional measures of inpatient quality of care for patients with heart failure. Am Heart J. 2012;163:239–45.e233.
Khayat R, Abraham W, Patt B, et al. Central sleep apnea is a predictor of cardiac readmission in hospitalized patients with systolic heart failure. J Card Fail. 2012;18:534–40.
McMurray JJ, Adamopoulos S, Anker SD, Bax JJ, Baumgartner H, Ceconi C, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2012;14:803–69.
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guidelines for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;62:e147–239.
Alpert MA, Omran J, Mehra A, et al. Impact of obesity and weight loss on cardiac performance and morphology in adults. Prog Cardiovasc Dis. 2014;56:391–400.
Somers VK, White DP, Amin R, American Heart Association Council for High Blood Pressure Research Professional Education Committee Central Oregon Community College, American Heart Association Stroke council, American Heart Association Council on Cardiovascular Nursing, American College of Cardiology Foundation, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation scientific statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation. 2008;118:1080–111.
Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the Sleep Heart Health study. Circulation. 2010;122:352–60.
Mehra R, Benjamin EJ, Shahar E, Sleep Heart Health Study, et al. Association of nocturnal arrhythmias with sleep-disordered breathing: the Sleep Heart Health study. Am J Respir Crit Care Med. 2006;173:910–6.
Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132.
Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14.
Schulz R, Blau A, Borgel J, working group Kreislauf und Schlaf of the German Sleep Study, et al. Sleep apnoea in heart failure. Eur Respir J. 2007;29:1201–5.
Oldenburg O, Lamp B, Faber L, et al. Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail. 2007;9:251–7.
Chan J, Sanderson J, Chan W, et al. Prevalence of sleep-disordered breathing in diastolic heart failure. Chest. 1997;111:1488–93.
Berry RB, Budhiraja R, Gottlieb DJ, American Academy of Sleep Medicine, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597–619.
Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep. 2009;22:667–89.
Smith PL, Wise RA, Gold AR, et al. Upper airway pressure-flow relationships in obstructive sleep apnea. J Appl Physiol. 1988;64:789–95.
Nopmaneejumruslers C, Kaneko Y, Hajek V, et al. Cheyne-Stokes respiration in stroke: relationship to hypocapnia and occult cardiac dysfunction. Am J Respir Crit Care Med. 2005;171:1048–52.
Bradley TD, Floras JS. Sleep apnea and heart failure: Part II: central sleep apnea. Circulation. 2003;107:1822–6.
Lanfranchi PA, Somers VK, Braghiroli A, et al. Central sleep apnea in left ventricular dysfunction: prevalence and implications for arrhythmic risk. Circulation. 2003;107:727–32.
Javaheri S. A mechanism of central sleep apnea in patients with heart failure. N Engl J Med. 1999;341:949–54.
Somers VK, Mark AL, Zavala DC, et al. Contrasting effects of hypoxia and hypercapnia on ventilation and sympathetic activity in humans. J Appl Physiol. 1989;67:2101–6.
Kusuoka H, Weisfeldt ML, Zweier JL, et al. Mechanism of early contractile failure during hypoxia in intact ferret heart: evidence for modulation of maximal ca2+-activated force by inorganic phosphate. Circ Res. 1986;59:270–82.
Stoohs R, Guilleminault C. Cardiovascular changes associated with obstructive sleep apnea syndrome. J Appl Physiol. 1992;72:583–9.
Parati G, Esler M. The human sympathetic nervous system: its relevance in hypertension and heart failure. Eur Heart J. 2012;33:1058–66.
Seif F, Patel SR, Walia HK, et al. Obstructive sleep apnea and diurnal nondipping hemodynamic indices in patients at increased cardiovascular risk. J Hypertens. 2014;32:267–75.
Floras JS. Sympathetic nervous system activation in human heart failure: clinical implications of an updated model. J Am Coll Cardiol. 2009;54:375–85.
Kusunose K, Zhang Y, Mazgalev TN, et al. Impact of vagal nerve stimulation on left atrial structure and function in a canine high-rate pacing model. Circ Heart Fail. 2014;7:320–6.
White LH, Bradley TD. Role of nocturnal rostral fluid shift in the pathogenesis of obstructive and central sleep apnoea. J Physiol. 2013;591:1179–93.
Redolfi S, Yumino D, Ruttanaumpawan P, et al. Relationship between overnight rostral fluid shift and obstructive sleep apnea in nonobese men. Am J Respir Crit Care Med. 2009;179:241–6.
Yumino D, Wang H, Floras JS, et al. Prevalence and physiological predictors of sleep apnea in patients with heart failure and systolic dysfunction. J Card Fail. 2009;15:279–85.
Nadeem R, Molnar J, Madbouly EM, et al. Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med. 2013;9:1003–12.
Xie X, Pan L, Ren D, et al. Effects of continuous positive airway pressure therapy on systemic inflammation in obstructive sleep apnea: a meta-analysis. Sleep Med. 2013;14:1139–50.
Hall TS, Herrscher TE, Jarolim P, et al. Myeloid-related protein-8/14 and c-reactive protein in individuals evaluated for obstructive sleep apnea. Sleep Med. 2014;15:762–8.
Cavalera M, Wang J, Frangogiannis NG. Obesity, metabolic dysfunction, and cardiac fibrosis: pathophysiological pathways, molecular mechanisms, and therapeutic opportunities. Translational research. J Lab Clin Med. 2014. doi:10.1016/j.trsl.2014.05.001.
Somers VK, Dyken ME, Skinner JL. Autonomic and hemodynamic responses and interactions during the Mueller maneuver in humans. J Auton Nerv Syst. 1993;44:253–9.
Mehra R, Redline S. Arrhythmia risk associated with sleep disordered breathing in chronic heart failure. Curr Heart Fail Rep. 2014;11:88–97.
Yoshihisa A, Suzuki S, Yamaki T, et al. Impact of adaptive servo-ventilation on cardiovascular function and prognosis in heart failure patients with preserved left ventricular ejection fraction and sleep-disordered breathing. Eur J Heart Fail. 2013;15:543–50.
Franklin KA, Eriksson P, Sahlin C, et al. Reversal of central sleep apnea with oxygen. Chest. 1997;111:163–9.
Hanly PJ, Millar TW, Steljes DG, et al. The effect of oxygen on respiration and sleep in patients with congestive heart failure. Ann Int Med. 1989;111:777–82.
Shigemitsu M, Nishio K, Kusuyama T, et al. Nocturnal oxygen therapy prevents progress of congestive heart failure with central sleep apnea. Int J Cardiol. 2007;115:354–60.
Staniforth AD, Kinnear WJ, Starling R, et al. Effect of oxygen on sleep quality, cognitive function and sympathetic activity in patients with chronic heart failure and Cheyne-Stokes respiration. Eur Heart J. 1998;19:922–8.
Javaheri S, Ahmed M, Parker TJ, et al. Effects of nasal o2 on sleep-related disordered breathing in ambulatory patients with stable heart failure. Sleep. 1999;22:1101–6.
Gottlieb DJ, Punjabi NM, Mehra R, et al. CPAP vs oxygen in obstructive sleep apnea. N Engl J Med. 2014;370:2276–85. A multicenter randomized controlled clinical trial which demonstrated that, unlike continuous positive airway pressure, supplemental oxygen was not effective in significantly improving the primary outcome, ie, reducing mean arterial blood pressure compared with control.
Wellman A, Malhotra A, Jordan AS, et al. Effect of oxygen in obstructive sleep apnea: role of loop gain. Respir Physiol Neurobiol. 2008;162:144–51.
Sakakibara M, Sakata Y, Usui K, et al. Effectiveness of short-term treatment with nocturnal oxygen therapy for central sleep apnea in patients with congestive heart failure. J Cardiol. 2005;46:53–61.
Sasayama S, Izumi T, Matsuzaki M, et al. Improvement of quality of life with nocturnal oxygen therapy in heart failure patients with central sleep apnea. Circ J. 2009;73:1255–62.
Sasayama S, Izumi T, Seino Y, Group C-HS, et al. Effects of nocturnal oxygen therapy on outcome measures in patients with chronic heart failure and Cheyne-Stokes respiration. Circ J. 2006;70:1–7.
Toyama T, Seki R, Kasama S, et al. Effectiveness of nocturnal home oxygen therapy to improve exercise capacity, cardiac function and cardiac sympathetic nerve activity in patients with chronic heart failure and central sleep apnea. Circ J. 2009;73:299–304.
Bradley TD, Logan AG, Kimoff RJ, Series F, Morrison D, Ferguson K, et al. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med. 2005;353:2025–33.
Arzt M, Floras JS, Logan AG, et al. Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian continuous Positive Airway Pressure for patients with central sleep apnea and heart failure trial (CANPAP). Circulation. 2007;115:3173–80.
Kohnlein T, Welte T, Tan LB, et al. Assisted ventilation for heart failure patients with Cheyne-Stokes respiration. Eur Respir J. 2002;20:934–41.
Arias MA, Garcia-Rio F, Alonso-Fernandez A, et al. Obstructive sleep apnea syndrome affects left ventricular diastolic function: effects of nasal continuous positive airway pressure in men. Circulation. 2005;112:375–83.
Marin JM, Carrizo SJ, Vicente E, et al. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53.
Arzt M, Wensel R, Montalvan S, et al. Effects of dynamic bi-level positive airway pressure support on central sleep apnea in men with heart failure. Chest. 2008;134:61–6.
Oliveira W, Campos O, Cintra F, et al. Impact of continuous positive airway pressure treatment on left atrial volume and function in patients with obstructive sleep apnoea assessed by real-time three-dimensional echocardiography. Heart. 2009;95:1872–8.
Kasai T, Usui Y, Yoshioka T, et al. Effect of flow-triggered adaptive servo-ventilation compared with continuous positive airway pressure in patients with chronic heart failure with coexisting obstructive sleep apnea and Cheyne-Stokes respiration. Circ Heart Fail. 2010;3:140–8.
Jilek C, Krenn M, Sebah D, et al. Prognostic impact of sleep disordered breathing and its treatment in heart failure: an observational study. Eur J Heart Fail. 2011;13:68–75.
Oldenburg O, Bitter T, Lehmann R, et al. Adaptive servoventilation improves cardiac function and respiratory stability. Clin Res Cardiol. 2011;100:107–15.
Takama N, Kurabayashi M. Effect of adaptive servo-ventilation on 1-year prognosis in heart failure patients. Circ J. 2012;76:661–7.
Kahwash R, Kikta D, Khayat R. Recognition and management of sleep-disordered breathing in chronic heart failure. Curr Heart Fail Rep. 2011;8:72–9.
Dohi T, Kasai T, Narui K, et al. Bi-level positive airway pressure ventilation for treating heart failure with central sleep apnea that is unresponsive to continuous positive airway pressure. Circ J. 2008;72:1100–5.
Kasai T, Narui K, Dohi T, et al. Efficacy of nasal bi-level positive airway pressure in congestive heart failure patients with Cheyne-Stokes respiration and central sleep apnea. Circ J. 2005;69:913–21.
Sharma BK, Bakker JP, McSharry DG, et al. Adaptive servoventilation for treatment of sleep-disordered breathing in heart failure: a systematic review and meta-analysis. Chest. 2012;142:1211–21.
Woehrle H, Oldenburg O, Arzt M, et al. Determining the prevalence and predictors of sleep disordered breathing in patients with chronic heart failure: rationale and design of the SCHLA-HF registry. BMC Cardiovasc Disord. 2014;14:46.
Javaheri S. Acetazolamide improves central sleep apnea in heart failure: a double-blind, prospective study. Am J Respir Crit Care Med. 2006;173:234–7.
Javaheri S, Parker TJ, Wexler L, et al. Effect of theophylline on sleep-disordered breathing in heart failure. N Engl J Med. 1996;335:562–7.
Nakayama H, Smith CA, Rodman JR, et al. Effect of ventilatory drive on carbon dioxide sensitivity below eupnea during sleep. Am J Respir Crit Care Med. 2002;165:1251–60.
Ponikowski P, Javaheri S, Michalkiewicz D, et al. Transvenous phrenic nerve stimulation for the treatment of central sleep apnoea in heart failure. Eur Heart J. 2012;33:889–94. This article describes phrenic nerve stimulation as a potential novel therapeutic approach.
Luthje L, Renner B, Kessels R, et al. Cardiac resynchronization therapy and atrial overdrive pacing for the treatment of central sleep apnoea. Eur J Heart Fail. 2009;11:273–80.
Stanchina ML, Ellison K, Malhotra A, et al. The impact of cardiac resynchronization therapy on obstructive sleep apnea in heart failure patients: a pilot study. Chest. 2007;132:433–9.
Compliance with Ethics Guidelines
Conflict of Interest
Reena Mehra is on the advisory board for CareCore and is employed at and received travel reimbursement from the Cleveland Clinic. Mehra received a grant from the NIH/NHLBI. Kenya Kusunose declares that he has no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Heart Failure Prevention
Rights and permissions
About this article
Cite this article
Kusunose, K., Mehra, R. Targeting Sleep Disordered Breathing to Prevent Heart Failure: What is the Evidence?. Curr Cardiovasc Risk Rep 8, 403 (2014). https://doi.org/10.1007/s12170-014-0403-8
Published:
DOI: https://doi.org/10.1007/s12170-014-0403-8