Abstract
Purpose of Review
The bidirectional relationships that have been demonstrated between heart failure (HF) and central sleep apnea (CSA) demand further exploration with respect to the implications that each condition has for the other. This review discusses the body of literature that has accumulated on these relationships and how CSA and its potential treatment may affect outcomes in patients with CSA.
Recent Findings
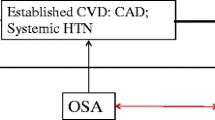
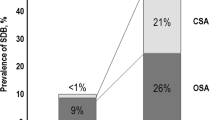
Obstructive sleep apnea (OSA) can exacerbate hypertension, type 2 diabetes, obesity, and atherosclerosis, which are known predicates of HF. Conversely, patients with HF more frequently exhibit OSA partly due to respiratory control system instability. These same mechanisms are responsible for the frequent association of HF with CSA with or without a Hunter-Cheyne-Stokes breathing (HCSB) pattern. Just as is the case with OSA, patients with HF complicated by CSA exhibit more severe cardiac dysfunction leading to increased mortality; the increase in severity of HF can in turn worsen the degree of sleep disordered breathing (SDB). Thus, a bidirectional relationship exists between HF and both phenotypes of SDB; moreover, an individual patient may exhibit a combination of these phenotypes.
Summary
Both types of SDB remain significantly underdiagnosed in patients with HF and hence undertreated. Appropriate screening for, and treatment of, OSA is clearly a significant factor in the comprehensive management of HF, while the relevance of CSA remains controversial. Given the unexpected results of the Treatment of Sleep-Disordered Breathing with Predominant Central Sleep Apnea by Adaptive Servo Ventilation in Patients with Heart Failure trial, it is now of paramount importance that additional analysis of these data be expeditiously reported. It is also critical that ongoing and proposed prospective studies of this issue proceed without delay.



Similar content being viewed by others
Abbreviations
- ADHF:
-
Acutely decompensated HF
- AFib:
-
Atrial fibrillation
- AHI:
-
Apnea-hypopnea index
- ASV:
-
Adaptive servo-ventilation
- BNP:
-
Brain natriuretic peptide
- BP:
-
Blood pressure
- CAI:
-
Central apnea index
- CSA:
-
Central sleep apnea
- CVD:
-
Cardiovascular disease
- EDS:
-
Excessive daytime sleepiness
- EPAP:
-
Expiratory positive airway pressure
- HCM:
-
Hypertrophic cardiomyopathy
- HCSB:
-
Hunter-Cheyne-Stokes breathing
- HF:
-
Heart failure
- HRQOL:
-
Health-related quality of life
- HSAT:
-
Home sleep apnea testing
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- HTN:
-
Hypertension
- IPAP:
-
Inspiratory positive airway pressure
- IPS:
-
Inspiratory pressure support
- LV:
-
Left ventricle
- LVEF:
-
Left ventricular ejection fraction
- MLHFQ:
-
Minnesota living with HF questionnaire
- MSNA:
-
Muscle sympathetic nerve activity
- NREM:
-
Non-rapid eye movement sleep
- NYHA:
-
New York Heart Association
- OSA:
-
Obstructive sleep apnea
- PAP:
-
Positive airway pressure
- PND:
-
Paroxysmal nocturnal dyspnea
- RCT:
-
Randomized controlled trial
- REI:
-
Respiratory event index
- SA:
-
Sleep apnea
- SDB:
-
Sleep disordered breathing
- S/T:
-
Spontaneous/timed
- T2DM:
-
Type 2 diabetes mellitus
- UA:
-
Upper airway
- VT:
-
Ventricular tachyarrhythmia
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14.
Roger VL. Epidemiology of heart failure. Circ Res. 2013;113:646–59.
Mitchell NS, Catenacci VA, Wyatt HR, Hill JO. Obesity: overview of an epidemic. Psychiatr Clin North Am. 2011;34:717–32.
Somers VK, White DP, Amin R, et al. American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology; American Heart Association Stroke Council; American Heart Association Council on Cardiovascular Nursing; American College of Cardiology Foundation: sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation. 2008;118:1080–111.
Poirier P, Giles TD, Bray GA, Hong Y, et al. American Heart Association, and obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism: obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918.
Khayat R, Small R, Rathman L, et al. Sleep-disordered breathing in heart failure: identifying and treating an important but often unrecognized comorbidity in heart failure patients. J Card Fail. 2013;19:431–44.
Javaheri S, Javaheri S, Javaheri A. Sleep apnea, heart failure, and pulmonary hypertension. Curr Heart Fail Rep. 2013;10:315–20.
Javaheri S, Caref EB, Chen E, Tong KB, Abraham WT. Sleep apnea testing and outcomes in a large cohort of Medicare beneficiaries with newly diagnosed heart failure. Am J Respir Crit Care Med. 2011;183:539–46.
Yumino D, Redolfi S, Ruttanaumpawan P, et al. Nocturnal rostral fluid shift: a unifying concept for the pathogenesis of obstructive and central sleep apnea in men with heart failure. Circulation. 2010;121:1598–605.
Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–8.
Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31:1079–85.
Hudgel DW, Chapman KR, Faulks C, Hendricks C. Changes in inspiratory muscle electrical activity and upper airway resistance during periodic breathing induced by hypoxia during sleep. Am Rev Respir Dis. 1987;135:899–906.
Berry RB, Brooks R, Gamaldo CE et al; for the American Academy of Sleep Medicine: The AASM manual for the scoring sleep and associated events: rules, terminology and technical specifications, version 2.4. www.aasmnet.org Darien, Illinois: American Academy of. Sleep Medicine, 2017.
Sahlin C, Svanborg E, Stenlund H, Franklin KA. Cheyne-Stokes respiration and supine dependency. Eur Respir J. 2005;25:829–33.
Longobardo GS, Gothe B, Goldman MD, Cherniack NS. Sleep apnea considered as a control system instability. Respir Physiol. 1982;50:311–33.
Badr MS, Grossman JE, Weber SA. Treatment of refractory sleep apnea with supplemental carbon dioxide. Am J Respir Crit Care Med. 1994;150:561–4.
White DP. Central sleep apnea. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of. sleep medicine. 3rd ed. Philadelphia: PA: W. B. Saunders; 2000. p. 827–39.
Tkacova R, Niroumand M, Lorenzi-Filho G, Bradley TD. Overnight shift from obstructive to central apneas in patients with heart failure: role of PCO2 and circulatory delay. Circulation. 2001;103:238–43.
Aurora RN, Chowdhuri S, Ramar K, et al. The treatment of central sleep apnea syndromes in adults: practice parameters with an evidence-based literature review and meta-analyses. Sleep. 2012;35:17–40.
• Donovan LM, Kapur VK. Prevalence and characteristics of central compared to obstructive sleep apnea: analyses from the Sleep Heart Health Study cohort. Sleep. 2016;39:1353–9. One of many important results of the long-running Sleep Heart Health Study, in this case contrasting attributes of the two major phenotypes of sleep disordered breathing.
Solin P, Bergin P, Richardson M, Kaye DM, Walters EH, Naughton MT. Influence of pulmonary capillary wedge pressure on central apnea in heart failure. Circulation. 1999;99:1574–9.
Gottlieb DJ, Yenokyan G, Newman AB, O’Connor GT, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–60.
Taranto L, Montemurro JS, Floras PJ, et al. Inverse relationship of subjective daytime sleepiness to sympathetic activity in patients with heart failure and obstructive sleep apnea. Chest. 2012;142:1222–8.
Yancy CW, Jessup M, Bozkurt B, et al. American College of Cardiology Foundation, and American Heart Association Task Force on Practice Guidelines: 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–239.
McKelvie RS, Moe GW, Cheung A, Costigan J, et al. The 2011 Canadian Cardiovascular Society heart failure management guidelines update: focus on sleep apnea, renal dysfunction, mechanical circulatory support, and palliative care. Can J Cardiol. 2011;27:319–38.
Chahal CAA, Somers VK. Risk factors. Sleep apnoea, atrial fibrillation, and heart failure—quo vadis? Nat Rev Cardiol. 2015;12:263–4.
Bitter T, Westerheide N, Hossain SM, Prinz C, Horstkotte D, Oldenburg O. Symptoms of sleep apnoea in chronic heart failure—results from a prospective cohort study in 1,500 patients. Sleep Breath Schlaf Atm. 2012;16:781–91.
Sin SS, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD. Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med. 1999;160:1101–6.
Sharma B, Owens R, Malhotra A. Sleep in congestive heart failure. Med Clin North Am. 2010;94:447–64.
Chan J, Sanderson J, Chan W, et al. Prevalence of sleep-disordered breathing in diastolic heart failure. Chest. 1997;111:1488–93.
• Arzt M, Woehrle H, Oldenburg O, Schla HF Investigators, et al. Prevalence and predictors of sleep-disordered breathing in patients with stable chronic heart failure: the Schla HF registry. JACC Heart Fail. 2016;4:116–25. Identification of sleep disordered breathing is known to be difficult in many patients with heart failure. This recent study points out some important factors to consider in screening patient with heart failure for possible diagnostic sleep testing. These factors were male gender, age, obesity, and the severity of left ventricular dysfunction and symptoms.
Javaheri S, Parker TJ, Liming JD, et al. Sleep apnea in 81 ambulatory male patients with stable heart failure. Types and their prevalences, consequences, and presentations. Circulation. 1998;97:2154–9.
Herrscher TE, Akre H, Øverland B, Sandvik L, Westheim AS. High prevalence of sleep apnea in heart failure outpatients: even in patients with preserved systolic function. J Card Fail. 2011;17:420–5.
Noda A, Miyata S, Yasuda Y. Therapeutic strategies for sleep apnea in hypertension and heart failure. Pulm Med. 2013;2013:814169.
Sekizuka H, Osada N, Miyake F. Sleep disordered breathing in heart failure patients with reduced versus preserved ejection fraction. Heart Lung Circ. 2013;22:104–9.
Findley LJ, Zwillich CW, Ancoli-Israel S, Kripke D, Tisi G, Moser KM. Cheyne-Stokes breathing during sleep in patients with left ventricular heart failure. South Med J. 1985;78:11–5.
Lanfranchi PA, Braghiroli A, Bosimini E, et al. Prognostic value of nocturnal Cheyne-Stokes respiration in chronic heart failure. Circulation. 1999;99:1435–40.
Hanly PJ, Zuberi-Khokhar NS. Increased mortality associated with Cheyne-Stokes respiration in patients with congestive heart failure. Am J Respir Crit Care Med. 1996;153:272–6.
Javaheri S, Parker TJ, Liming JD, et al. Sleep apnea in 81 ambulatory male patients with stable heart failure. Types and their prevalences, consequences, and presentations. Circulation. 1998;97:2154–9.
Johansson P, Alehagen U, Svanborg E, Dahlstrom U, Brostrom A. Clinical characteristics and mortality risk in relation to obstructive and central sleep apnoea in community-dwelling elderly individuals: a 7-year follow-up. Age Ageing. 2012;41:468–74.
Naughton MT, Benard DC, Liu PP, Rutherford R, Rankin F, Bradley TD. Effects of nasal CPAP on sympathetic activity in patients with heart failure and central sleep apnea. Am J Respir Crit Care Med. 1995;152:473–9.
Mansfield D, Kaye DM, Brunner La Rocca H, Solin P, Esler MD, Naughton MT. Raised sympathetic nerve activity in heart failure and central sleep apnea is due to heart failure severity. Circulation. 2003;107:1396–400.
Lanfranchi PA, Braghiroli A, Bosimini E, et al. Prognostic value of nocturnal Cheyne-Stokes respiration in chronic heart failure. Circulation. 1999;99:1435–40.
Hanly PJ, Zuberi-Khokhar NS. Increased mortality associated with Cheyne-Stokes respiration in patients with congestive heart failure. Am J Respir Crit Care Med. 1996;153:272–6.
Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25.
Oldenburg O, Wellmann B, Buchholz A, et al. Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur Heart J. 2016;37:1695–703.
Mac Donald M, Fang J, Pittman SD S, White DP, Malhotra A. The current prevalence of sleep disordered breathing in congestive heart failure patients treated with beta-blockers. J Clin Sleep Med. 2008;4:38–42.
Ljunggren M, Byberg L, Theorell-Haglöw J, Lindahl B, Michaëlsson K, Lindberg E. Increased risk of heart failure in women with symptoms of sleep-disordered breathing. Sleep Med. 2016;17:32–7.
Roca GQ, Redline S, Claggett B, et al. Sex-specific association of sleep apnea severity with subclinical myocardial Injury, ventricular hypertrophy, and heart failure risk in a community-dwelling cohort: the atherosclerosis risk in communities-Sleep Heart Health Study. Circulation. 2015;132:1329–37.
Hla KM, Young T, Hagen EW, et al. Coronary heart disease incidence in sleep disordered breathing: the Wisconsin Sleep Cohort Study. Sleep. 2015;38:677–84.
Carmona-Bernal C, Ruiz-García A, Villa-Gil M, et al. Quality of life in patients with congestive heart failure and central sleep apnea. Sleep Med. 2008;9:646–51.
Won C, Guilleminault C. Gender differences in sleep disordered breathing: implications for therapy. Expert Rev Respir Med. 2015;9:221–31.
Olafiranye O, Akinboboye O, Mitchell JE, Ogedegbe G, Jean-Louis G. Obstructive sleep apnea and cardiovascular disease in blacks: a call to action from the Association of Black Cardiologists. Am Heart J. 2013;165:468–76.
Khayat R, Abraham W, Patt B, Brinkman V, Wannemacher J, Porter K, et al. Central sleep apnea is a predictor of cardiac readmission in hospitalized patients with systolic heart failure. J Card Fail. 2012;18:534–40.
Pedrosa RP, Drager LF, Genta PR, et al. Obstructive sleep apnea is common and independently associated with atrial fibrillation in patients with hypertrophic cardiomyopathy. Chest. 2010;137:1078–84.
Jordan AS, Wellman W, Edwards JK, et al. Respiratory control stability and upper airway collapsibility in men and women with obstructive sleep apnea. J Appl Physiol. 2005;99:2020–7.
Shiota S, Ryan CM, Chiu K-L, et al. Alterations in upper airway cross-sectional area in response to lower body positive pressure in healthy subjects. Thorax. 2007;62:868–72.
Chiu K-L, Ryan CM, Shiota S, et al. Fluid shift by lower body positive pressure increases pharyngeal resistance in healthy subjects. Am J Respir Crit Care Med. 2006;174:1378–83.
Su M-C, Chiu K-L, Ruttanaumpawan P, et al. Lower body positive pressure increases upper airway collapsibility in healthy subjects. Respir Physiol Neurobiol. 2008;161:306–12.
Redolfi S, Yumino D, Ruttanaumpawan P, et al. Relationship between overnight rostral fluid shift and obstructive sleep apnea in nonobese men. Am J Respir Crit Care Med. 2009;179:241–6.
• Kasai T, Motwani SS, Yumino D, et al. Contrasting effects of lower body positive pressure on upper airways resistance and partial pressure of carbon dioxide in men with heart failure and obstructive or central sleep apnea. J Am Coll Cardiol. 2013;61:1157–66. Points out the importance of fluid overload and fluid shifts in the pathogenesis of obstructive sleep apnea in heart failure.
Floras JS, Bradley TD. Sleep apnoea in acute heart failure: fluid in flux. Eur Heart J. 2015;36:1428–30.
Ryan CM, Floras JS, Logan AG, et al. Shift in sleep apnoea type in heart failure patients in the CANPAP trial. Eur Respir J. 2010;35:592–7.
Jilek C, Krenn M, Sebah D, et al. Prognostic impact of sleep disordered breathing and its treatment in heart failure: an observational study. Eur J Heart Fail. 2011;13:68–75.
Lavie L. Oxidative stress--a unifying paradigm in obstructive sleep apnea and comorbidities. Prog Cardiovasc Dis. 2009;51:303–12.
Foster GE, Poulin MJ, Hanly PJ. Intermittent hypoxia and vascular function: implications for obstructive sleep apnoea. Exp Physiol. 2007;92:51–65.
GF DB. Nervous kidney. Interaction between renal sympathetic nerves and the renin-angiotensin system in the control of renal function. Hypertension. 2000;36:1083–8.
Fletcher EC, Orolinova N, Bader M. Blood pressure response to chronic episodic hypoxia: the renin-angiotensin system. J Appl Physiol. 2002;92:627–33.
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62.
Doonan RJ, Scheffler P, Lalli M, et al. Increased arterial stiffness in obstructive sleep apnea: a systematic review. Hypertens Res. 2011;34:23–32.
Foster GE, Poulin MJ, Hanly PJ. Intermittent hypoxia and vascular function: implications for obstructive sleep apnoea. Exp Physiol. 2007;92:51–65.
Romero-Corral A, Somers VK, Pellikka PA, et al. Decreased right and left ventricular myocardial performance in obstructive sleep apnea. Chest. 2007;132:1863–70.
Buda AJ, Pinsky MR, Ingels NB, Daughters GT, Stinson EB, Alderman EL. Effect of intrathoracic pressure on left ventricular performance. N Engl J Med. 1979;301:453–9.
Bradley TD, Hall MJ, Ando S, Floras JS. Hemodynamic effects of simulated obstructive apneas in humans with and without heart failure. Chest. 2001;119:1827–35.
Arias MA, García-Río F, Alonso-Fernández A, Mediano O, Martínez I, Villamor J. Obstructive sleep apnea syndrome affects left ventricular diastolic function: effects of nasal continuous positive airway pressure in men. Circulation. 2005;112:375–83.
Punjabi NM, Sorkin JD, Katzel LI, Goldberg AP, Schwartz AR, Smith PL. Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med. 2002;165:677–82.
Broussard JL, Ehrmann DA, Van Cauter E, Tasali E, Brady MJ. Impaired insulin signaling in human adipocytes after experimental sleep restriction; a randomized, crossover study. Ann Intern Med. 2012;157:549–57.
Reichmuth KJ, Austin D, Skatrud JB, Young T. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med. 2005;172:1590–5.
Dursunoglu D, Dursunoglu N, Evrengül H, et al. Impact of obstructive sleep apnoea on left ventricular mass and global function. Eur Respir J. 2005;26:283–8.
Carmona-Bernal C, Quintana-Gallego E, Villa-Gil M, Sánchez-Armengol A, Martinez Martinez A, Capote F. Brain natriuretic peptide in patients with congestive heart failure and central sleep apnea. Chest. 2005;127:1667–73.
Javaheri S, Corbett WS. Association of low PaCO2 with central sleep apnea and ventricular arrhythmias in ambulatory patients with stable heart failure. Ann Intern Med. 1998;128:204–7.
Naughton MT, Benard DC, Liu PP, Rutherford R, Rankin F, Bradley TD. Effects of nasal CPAP on sympathetic activity in patients with heart failure and central sleep apnea. Am J Respir Crit Care Med. 1995;152:473–9.
Van de Borne P, Oren R, Abouassaly C, et al. Effect of Cheyne-Stokes respiration on muscle sympathetic nerve activity in severe congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1998;81:432–6.
Packer M, Coats AJ, Fowler MB, Carvedilol Prospective Randomized Cumulative Survival Study Group, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344:1651–8.
Pepperell JC, Maskell NA, Jones DR, et al. A randomized controlled trial of adaptive ventilation for Cheyne-Stokes breathing in heart failure. Am J Respir Crit Care Med. 2003;168:1109–14.
Ushijima R, Joho S, Akabane T, et al. Differing effects of adaptive servo-ventilation and continuous positive airway pressure on muscle sympathetic nerve activity in patients with heart failure. Circ J. 2014;78:1387–95.
Kourouklis SP, Vagiakis E, Paraskevaidis IA, et al. Effective sleep apnoea treatment improves cardiac function in patients with chronic heart failure. Int J Cardiol. 2013;168:157–62.
Koyama T, Watanabe H, Tamura Y, et al. Adaptive servo-ventilation therapy improves cardiac sympathetic nerve activity in patients with heart failure. Eur J Heart Fail. 2013;15:902–9.
Kasai T, Kasagi S, Maeno K, et al. Adaptive servo-ventilation in cardiac function and neurohormonal status in patients with heart failure and central sleep apnea nonresponsive to continuous positive airway pressure. J Am Coll Cardiol HF. 2013;1:58–63.
Hetland A, Haugaa KH, Olseng M, et al. Three-month treatment with adaptive servoventilation improves cardiac function and physical activity in patients with chronic heart failure and Cheyne-Stokes respiration: a prospective randomized controlled trial. Cardiol. 2013;126:81–90.
Corrà U, Pistono M, Mezzani A, et al. Sleep and exertional periodic breathing in chronic heart failure: prognostic importance and interdependence. Circulation. 2006;113:44–50.
Luo Q, Zhang H-L, Tao X-C, Yang Y-J, Liu Z-H. Impact of untreated sleep apnea on prognosis of patients with congestive heart failure. Int J Cardiol. 2009;3:420–2.
Javaheri S, Shukla R, Zeigler H, et al. Central sleep apnea, right ventricular dysfunction and low diastolic blood pressure are predictors of mortality in systolic heart failure. J Am Coll Cardiol. 2007;49:2028–34.
Bradley TD, Logan AG, Kimoff RJ, CANPAP Investigators, et al. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med. 2005;353:2025–33.
Arzt M, Floras JS, Logan AG, CANPAP Investigators, et al. Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure Trial (CANPAP). Circulation. 2007;115:3173–80.
Khayat RN, Abraham WT. Current treatment approaches and trials in central sleep apnea. Int J Cardiol. 2016;206(Suppl):S22–7.
Naughton MT. Cheyne-Stokes respiration: friend or foe? Thorax. 2012;67:357–60.
Costa LE, Uchôa CHG, Harmon RR, Bortolotto LA, Lorenzi-Filho G. aDrager LF: potential underdiagnosis of obstructive sleep apnoea in the cardiology outpatient setting. Heart Br Card Soc. 2015;101:1288–92.
Fuchs FD, Martinez D. Obstructive sleep apnoea should be deemed a cardiovascular disease. Heart Br Card Soc. 2015;101:1261–2.
Kimoff RJ. When to suspect sleep apnea and what to do about it. Can J Cardiol. 2015;31:945–8.
Smith LA, Chong DW, Vennelle M, Denvir MA, Newby DE, Douglas NJ. Diagnosis of sleep-disordered breathing in patients with chronic heart failure: evaluation of a portable limited sleep study system. J Sleep Res. 2007;16:428–35.
Skinner MA, Choudhury MS, Homan SD, Cowan JO, Wilkins GT, Taylor DR. Accuracy of monitoring for sleep-related breathing disorders in the coronary care unit. Chest. 2005;127:66–71.
Tamura A, Kawano Y, Naono S, Kotoku M, Kadota J. Relationship between beta-blocker treatment and the severity of central sleep apnea in chronic heart failure. Chest. 2007;131:130–5.
Bucca CB, Brussino L, Battisti A, Mutani R, Rolla G, Mangiardi L, et al. Diuretics in obstructive sleep apnea with diastolic heart failure. Chest. 2007;132:440–6.
Kahwash R, Kikta D, Khayat R. Recognition and management of sleep-disordered breathing in chronic heart failure. Curr Heart Fail Rep. 2011;8:72–9.
Lenique F, Habis M, Lofaso F, Dubois-Randé JL, Harf A, Brochard L. Ventilatory and hemodynamic effects of continuous positive airway pressure in left heart failure. Am J Respir Crit Care Med. 1997;155:500–5.
Sun H, Shi J, Li M, Chen X. Impact of continuous positive airway pressure treatment on left ventricular ejection fraction in patients with obstructive sleep apnea: a meta-analysis of randomized controlled trials. PLoS One. 2013;8:e62298.
Kaneko Y, Floras JS, Usui K, et al. Cardiovascular effects of continuous positive airway pressure in patients with heart failure and obstructive sleep apnea. N Engl J Med. 2003;348:1233–41.
Mansfield DR, Gollogly NC, Kaye DM, Richardson M, Bergin P, Naughton MT. Controlled trial of continuous positive airway pressure in obstructive sleep apnea and heart failure. Am J Respir Crit Care Med. 2004;169:361–6.
Aggarwal S, Nadeem R, Loomba RS, Nida M, Vieira D. The effects of continuous positive airways pressure therapy on cardiovascular end points in patients with sleep-disordered breathing and heart failure: a meta-analysis of randomized controlled trials. Clin Cardiol. 2014;37:57–65.
Yoshinaga K, Burwash IG, Leech JA, et al. The effects of continuous positive airway pressure on myocardial energetics in patients with heart failure and obstructive sleep apnea. J Am Coll Cardiol. 2007;49:450–8.
Khayat RN, Abraham WT, Patt B, Pu M, Jarjoura D. In-hospital treatment of obstructive sleep apnea during decompensation of heart failure. Chest. 2009;136:991–7.
Peter JV, Moran I, Phillips-Hughes J, Graham P, Bersten AD. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet. 2006;367:1155–63.
Plaisance P, Pirracchio R, Berton C, Vicaut E, Payen D. A randomized study of out-of-hospital continuous positive airway pressure for acute cardiogenic pulmonary oedema: physiological and clinical effects. Eur Heart J. 2007;28:2895–901.
Kauta SR, Keenan BT, Goldberg L, Schwab RJ. Diagnosis and treatment of sleep disordered breathing in hospitalized cardiac patients: a reduction in 30-day hospital readmission rates. J Clin Sleep Med. 2014;10:1051–9.
Javaheri S, Shukla R, Wexler L. Association of smoking, sleep apnea, and plasma alkalosis with nocturnal ventricular arrhythmias in men with systolic heart failure. Chest. 2012;141:1449–56.
Javaheri S, Sands SA, Edwards BA. Acetazolamide attenuates Hunter-Cheyne-Stokes breathing but augments the hypercapnic ventilatory response in patients with heart failure. Ann Am Thorac Soc. 2014;11:80–6.
Javaheri S, Sands SA, Edwards BA. Acetazolamide attenuates Hunter-Cheyne-Stokes breathing but augments the hypercapnic ventilatory response in patients with heart failure. Ann Am Thorac Soc. 2014;11:80–6.
Heidrun F, Kiwull-Schöne H, Teppema LJ, Kiwull PJ. Low-dose acetazolamide does affect respiratory muscle function in spontaneously breathing anesthetized rabbits. Am J Respir Crit Care Med. 2001;163:478–83.
Sasayama S, Izumi T, Seino Y, Ueshima K, Asanoi H, and the CHF-HOT Study Group: Effects of nocturnal oxygen therapy on outcome measures in patients with chronic heart failure and Cheyne-Stokes respiration, Circ J 2006, 70:1–7.
Sasayama S, Izumi T, Matsuzaki M, CHF-HOT Study Group. Improvement of quality of life with nocturnal oxygen therapy in heart failure patients with central sleep apnea. Circ J. 2009;73:1255–62.
• Nakao YM, Ueshima K, Yasuno S, Sasayama S. Effects of nocturnal oxygen therapy in patients with chronic heart failure and central sleep apnea: CHF-HOT study. Heart Vessel. 2016;31:165–72. Evidence that treatment with nocturnal oxygen, when it effectively suppresses central sleep apnea in patients with heart failure, provides a benefit in terms of surrogate endpoints.
Javaheri S, Ahmed M, Parker TJ, Brown CR. Effects of nasal O2 on sleep-related disordered breathing in ambulatory patients with stable heart failure. Sleep. 22(8):1101–6.
Javaheri S. Effects of continuous positive airway pressure on sleep apnea and ventricular irritability in patients with heart failure. Circulation. 2000;101:392–7.
Davies RJ, Harrington KJ, Ormerod OJ, Stradling JR. Nasal continuous positive airway pressure in chronic heart failure with sleep-disordered breathing. Am Rev Respir Dis. 1993;147:630–4.
Sands SA, Edwards BA, Kee K, et al. Loop gain as a means to predict a positive airway pressure suppression of Cheyne-Stokes respiration in patients with heart failure. Am J Respir Crit Care Med. 2011;184:1067–75.
Javaheri S, Dempsey JA. Central sleep apnea. Compr Physiol. 2013;3:141–63.
Lorenzi-Filho G, Rankin F, Bies I, Douglas Bradley T. Effects of inhaled carbon dioxide and oxygen on Cheyne–Stokes respiration in patients with heart failure. Am J Respir Crit Care Med. 1999;159:1490–8.
Steens RD, Millar TW, Xiaoling S, et al. Effect of inhaled 3% CO2 on Cheyne–Stokes respiration in congestive heart failure. Sleep. 1994;17:61–8.
Khayat RN, Xie A, Patel AK, Kaminski A, Skatrud JB. Cardiorespiratory effects of added dead space in patients with heart failure and central sleep apnea. Chest. 2003;123:1551–60.
Ponikowski P, Javaheri S, Dariusz Michalkiewicz D, et al. Transvenous phrenic nerve stimulation for the treatment of central sleep apnoea in heart failure. Eur Heart J. 2012;33:889–94.
Abraham WT, Jagielski D, Oldenburg O, Remedē Pilot Study Investigators, et al. Phrenic nerve stimulation for the treatment of central sleep apnea. JACC Heart Fail. 2015;3:360–9.
Respicardia, Inc: A randomized trial evaluating the safety and effectiveness of the Remedē® system in patients with central sleep apnea. Available at: https://clinicaltrials.gov/ct 2/show/NCT01816776. Accessed 9/26/16.
Respicardia, Inc: Safety and efficacy evaluation of Respicardia therapy for central sleep apnea. Available at: https://clinicaltrials.gov/ct 2/show/NCT01124370 Accessed 9/26/16.
Koyama T, Watanabe H, Terada S, et al. Adaptive servo-ventilation improves renal function in patients with heart failure. Respir Med. 2011;105:1946–53.
Sharma BK, Bakker JP, McSharry DG, Desai AS, Javaheri S, Malhotra A. Adaptive servoventilation for treatment of sleep-disordered breathing in heart failure: a systematic review and meta-analysis. Chest. 2012;142:1211–21.
Bitter T, Gutleben K-J, Nölker G, et al. Treatment of Cheyne-Stokes respiration reduces arrhythmic events in chronic heart failure. J Cardiovasc Electrophysiol. 2013;24:1132–40.
Nakamura S, Asai K, Kubota Y, et al. Impact of sleep-disordered breathing and efficacy of positive airway pressure on mortality in patients with chronic heart failure and sleep-disordered breathing: a meta-analysis. Clin Res Cardiol. 2015;104:208–16.
Birner C, Sériès F, Lewis K, et al. Effects of auto-servo ventilation on patients with sleep-disordered breathing, stable systolic heart failure and concomitant diastolic dysfunction: subanalysis of a randomized controlled trial. Respir Int Rev Thorac Dis. 2014;87:54–62.
Kasai T, Usui Y, Yoshioka T, JASV Investigators, et al. Effect of flow-triggered adaptive servo-ventilation compared with continuous positive airway pressure in patients with chronic heart failure with coexisting obstructive sleep apnea and Cheyne-Stokes respiration. Circ Heart Fail. 2010;3:140–8.
Kourouklis SP, Vagiakis E, Paraskevaidis IA, et al. Effective sleep apnoea treatment improves cardiac function in patients with chronic heart failure. Int J Cardiol. 2013;168:157–62.
Yoshihisa A, Suzuki S, Yamaki T, et al. Impact of adaptive servo-ventilation on cardiovascular function and prognosis in heart failure patients with preserved left ventricular ejection fraction and sleep-disordered breathing. Eur J Heart Fail. 2013;15:543–50.
• Cowie MR, Woehrle H, Wegscheider K, et al. Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N Engl J Med. 2015;373:1095–105. Despite a number of methodological flaws, this study changed the paradigm for treatment of patients with systolic heart failure and central sleep apnea virtually overnight, proscribing the use of adaptive servo-ventilation in these individuals.
• Javaheri S, Brown LK, Randerath W, Khayat R. SERVE-HF: more questions than answers. Chest. 2016;149:900–4. A thorough critique of the SERVE-HF trial and its results, suggesting that the radical change in treatment of central sleep apnea in patients with systolic heart failure (proscription of the use of adaptive servo-ventilation) may not have been justified.
Fiuzat M, Oldenberg O, Whellan DJ, et al. Lessons learned from a clinical trial: design, rationale, and insights from The Cardiovascular Improvements with Minute Ventilation-targeted Adaptive Sero-Ventilation (ASV) Therapy in Heart Failure (CAT-HF) Study. Contemp Clin Trials. 2016;47:158–64.
West JB: Respiratory physiology. The essentials, 9th ed. Philadelphia: Lippincott Williams & Wilkins, 2012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sushma M. Dharia declares no conflict of interest. Lee K. Brown has participated in advisory panels for Philips Respironics and is an insurance claims reviewer for Considine and Associates, Inc. He coedits the sleep and respiratory neurobiology section of Current Opinion in Pulmonary Medicine and wrote on CPAP treatment for obstructive sleep apnea in UpToDate and on obstructive sleep apnea in Clinical Decision Support: Pulmonary Medicine and Sleep Disorders. He is currently coediting an issue of Sleep Medicine Clinics on positive airway pressure therapy. He serves on the Polysomnography Practice Advisory Committee of the New Mexico Medical Board and chairs the New Mexico Respiratory Care Advisory Board.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Epidemiology of Heart Failure
Rights and permissions
About this article
Cite this article
Dharia, S.M., Brown, L.K. Epidemiology of Sleep-Disordered Breathing and Heart Failure: What Drives What. Curr Heart Fail Rep 14, 351–364 (2017). https://doi.org/10.1007/s11897-017-0348-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-017-0348-6