Abstract
Background/Purpose
The present study attempted to replicate our previous finding that depressive symptoms are a risk factor for mortality in stable chronic obstructive pulmonary disease (COPD), but in a different population with a different measure of depressive symptoms. We further investigated whether type D personality is associated with mortality in patients with COPD and whether it explains any relationship observed between depressive symptoms and mortality.
Methods
In 122 COPD patients, mean age 60.8 ± 10.3 years, 52% female, and mean forced expiratory volume in 1 s (FEV1) 41.1 ± 17.6%pred, we assessed body mass index, post bronchodilator FEV1, exercise capacity, depressive symptoms with the Hospital Anxiety and Depression Scale, and type D with the Type D Scale.
Results
In the 7 years follow-up, 48 (39%) deaths occurred. The median survival time was 5.3 years. Depressive symptoms (hazard ratio = 1.07, 95% confidence intervals = 1.00–1.14) were an independent risk factor for mortality. Type D was not associated with mortality.
Conclusions
We can rule out type D as an explanation for the relationship between depressive symptoms and mortality observed in this sample. However, ambiguity remains as to the interpretation of the value of depressive symptoms in predicting death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Studies increasingly report that both depression and trait negative affectivity (NA) predict poor health outcomes, especially in coronary heart disease (CHD) [1–5]. In particular, associations between depression and all-cause mortality have been found in general community samples [6], as well as in persons with coronary heart disease, diabetes mellitus, and hypertension [7–11]. The prevalence of depressive symptoms in patients with chronic obstructive pulmonary disease (COPD) varies from 6% to over 60% [12–14], with most studies indicating prevalence well over 20% [15]. Therefore, the prognostic value of depressive symptoms for health status and survival among patients with COPD needs more attention than it has yet received.
COPD and Mortality
In COPD, most studies examining prognostic factors for mortality focus on single physiological variables. Mortality has been found to be predicted by airflow limitation, hypercapnia, hypoxemia, more severe dyspnea, low body mass index (BMI), and low exercise capacity [16–23]. In addition, the BODE index, a multidimensional ten-point scale consisting of graded scores of BMI, airflow obstruction, dyspnea, and exercise capacity is considered a valuable tool for predicting the risk of death in patients with COPD [24, 25].
To our knowledge, only two studies have demonstrated that symptoms of depression are associated with mortality in patients with COPD after hospitalization, independent of disease severity and other risk factors [26, 27]. These studies were carried out among patients with COPD shortly after they were hospitalized for acute exacerbation. Depression symptoms were assessed during hospitalization or immediately after discharge (2–4 weeks). The recent exacerbation could well have increased both the self-reported depressive symptoms, as well as conveyed increased mortality, introducing an important confound in any apparent association between depressive symptoms and death.
In clinically stable COPD, the association between depressive symptoms and mortality has been less clear. Two studies did not find an association after adjusting for disease severity [28, 29] and only one study demonstrated that adjusted depressive symptoms were associated with 3-year mortality and not with 1-year mortality in stable COPD [30]. However, we recently demonstrated, in a different cohort than the sample in the present study, that, in patients with stable COPD, symptoms of depression, assessed with the Beck Depression Inventory (BDI), were a prognostic factor for mortality, independent of age, sex, and exercise capacity (hazard ratio = 1.93, 95% confidence intervals [95%CI] = 1.12–3.33) [31]. While the study seemed to establish depressive symptoms as predictor of mortality over a relatively long period of time, ranging from 88 days to 7.8 years, there remains ambiguity in the explanation for our finding.
The Distressed Personality (Type D)
Denollet and his coworkers suggested that depression is related to underlying broader and more stable personality traits, which may explain individual differences in distress and mortality in patients with cardiovascular disease [32–34]. Denollet and his coworkers reported in several studies on “the notion that a general tendency to experience emotional and interpersonal difficulties may exacerbate progression of heart disease, irrespective of the diagnosis of depression or anxiety disorder,” which is the core of the “distressed (type D) personality” [35, page 949]. In an attempt to emphasize the role of normal personality characteristics rather than psychopathology, the “distressed (type D) personality” was constructed of two specific, nonpathological traits: NA (the tendency to experience negative emotions) and social inhibition (SI; the tendency to inhibit the expression of these emotions in social interaction). In research on coronary heart disease, type D is associated with increased risk of depression, vital exhaustion, social alienation, a high number of reinfarctions, and higher mortality, independently of traditional biomedical risk factors [36–38]. It is noteworthy that, for patients with COPD, there is strong evidence for cardiovascular comorbidity and mortality, with estimates up to 42% [39–41]. Moreover, to our knowledge, no studies have been done on the impact of type D on mortality in patients with COPD or any other chronic medical conditions besides cardiovascular diseases. Because of the relationship observed between depression and mortality, type D may offer an explanation in COPD as well.
Hence, the first aim of the present study was to attempt to replicate in a different population, with a different measure of depressive symptoms, earlier findings, including our own, on the association of depression symptoms and all-cause mortality in patients with stable COPD. We adjusted for known risk factors, such as age, forced expiratory volume in 1 s (FEV1) %pred, exercise capacity, BMI, and smoking behavior. The second aim was to examine if the presence of distressed personality (type D) is a prognostic factor for mortality in patients with COPD and, by doing so, explore a possible explanation for the association between depressive symptoms and mortality.
Methods
Subjects
Our study sample consisted of 122 consecutive patients with stable COPD (FEV1 < 80% predicted), diagnosed according to the ATS guidelines [42], who were referred for pulmonary rehabilitation within a period of 2 years. All patients were clinically stable for at least 6 weeks and did not require increase in medication or hospitalization. Exclusion criteria were inability to perform lung function and/or ergometry, refusal to fill out psychological questionnaires, and the presence of comorbidity which limits prognosis such as malignancy or severe heart failure.
Measurements
Patient Characteristics
Upon admission, demographic data, such as sex and age, were recorded. Marital status was dichotomized in terms of living with a partner versus living without a partner. Patients without a partner included those patients who were widowed, divorced, or never married. Smoking behavior was assessed by a self-report questionnaire and defined in three categories: (1) never smoked cigarettes (NS), (2) cessation of smoking for 1 year or more (ES ≥ 1 year), and (3) current smoker (CS) or cessation of smoking less than 1 year (ES < 1 year).
Depression
Depressive symptoms were assessed with the depression subscale of the Hospital Anxiety and Depression Scale (HADS) [43, 44]. The HADS is a validated and reliable psychological measure and it is widely used in medically ill populations. This 14-item self-report screening scale was developed to indicate the presence of anxious and depressive states. The depression subscale has seven items and total score range from 0 to 21, with a higher score indicating more pathology. In the present paper, we studied depressive symptoms and not major depressive disorder. To facilitate interpretation and comparison with others’ data, we also analyzed depressive symptoms using the conventional cut-off level of ≥8 to label patients in high and low depressive symptoms distinction.
Type D Personality
A distressed personality (type D) was assessed by the Type D Scale (DS16), a brief self-report measure comprising of an eight-item NA scale, which assesses the tendency to experience negative emotions, and an eight-item SI scale, which assesses the tendency to inhibit the expression of these emotions in social interaction [37]. Consistent with all past studies, these continuous variables were dichotomized using the same cut-off as the Denollet study, which were based on a median split of the NA and SI scales in his study. Patients with a distressed personality or type D reported high levels of NA (≥10) and SI (≥15).
Physiological Parameters
The BMI is weight in kilograms divided by the square of the body height in meters. Airflow obstruction was established by the FEV1, post bronchodilator, expressed in liters and as percentage of the predicted value and was assessed according to ATS standards (Jaeger Masterlab 4.521). Exercise capacity (W peak) was defined as the highest workload reached and maintained for at least 30 s during a symptom-limited incremental cycle ergometry (Oxycon pro, Viasys Healthcare) [45]. A protocol with 5 or 10 W/min increment in load was applied depending on the estimated W peak, starting with 1 min of unloaded pedaling and aiming at a duration of 6–12 min.
Mortality
The vital status of these patients was ascertained on 1st of April 2007 using municipal registrations. The rationale for relying on all-cause mortality was that clinical assessments of cause of death are difficult, often incorrect and always involve a subjective component [46].
Statistical Analysis
All analyses were performed using SPSS for Windows (SPSS, Chicago, IL, USA). All 122 patients were included in the analyses. Continuous variables are presented as means and standard deviations, except for follow-up time, where medians were presented. Dichotomous variables are presented as percentages. Surviving and nonsurviving patients were compared using independent t test for continuous variables and Fisher’s exact test for dichotomous variables. The relations among the variables were analyzed using Pearson’s correlations for continuous variables and Spearman’s correlations for ordinal variables (e.g., smoking). Bivariate hazard ratios associated with each possible predictor variable for mortality were examined. Multivariate Cox proportional hazard analyses with all variables entering in a single step in the model with backward stepwise selection, backward stepwise (Wald), were used to quantify the relationship between baseline variables and mortality and 95%CI were estimated with significance at p < 0.05. On a multivariate level, we analyzed whether type D adds to the model or whether type D is associated with mortality independent of age, FEV1 %pred, and W peak. High/low depressive symptoms were plotted in survival curves using Kaplan–Meier estimates.
Results
Characteristics of our study sample (63 women and 59 men) on the whole and according to their vital status are presented in Table 1. Correlations among the key predictor variables are presented in Table 2. The average age was 60.8 ± 10.3 years and the post bronchodilator FEV1 %pred was 41.1 ± 17.6.
The mean score was 6.3 ± 4.2 on the HADS depression scale. A third of the patients (33%) tested above the standard cut-off score and can be classified as having substantial depressive symptoms. Survival time varied from 21 days to 7 years (median = 5.3 years). For the 122 patients, 1-year mortality was 5 (4%), 2-year mortality was 12 (10%), 3-year mortality was 24 (20%), 4-year mortality was 33 (27%), 5-year mortality was 41 (34%), and 6-year mortality was 48 (39%). The rate of death differed between high depressive symptoms patients (21/40 = 53%) and low depressive symptoms patients (27/82 = 33%), chi square p = 0.04. Other significant differences between survivors and nonsurvivors were that survivors tested a larger FEV1 expressed in liters and as percentage of predicted value and more exercise capacity (W peak). Differences on sex, marital status, smoking behavior, BMI, and type D were not significant. Depressive symptoms were correlated with younger age (r = −0.18), current smoking or having quitted smoking less than a year (r = 0.21), type D (r = 0.49), and both DS16 subscales NA (r = 0.74) and SI (r = 0.36).
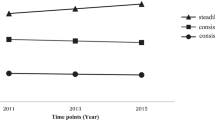
Table 3 shows the unadjusted and adjusted Cox proportional hazards analyses. On a bivariate level, having a lower FEV1 %pred (hazard ratio = 0.95, 95%CI = 0.93–0.97), a lower exercise capacity (W peak; hazard ratio = 0.97, 95%CI = 0.95–0.98), and having more symptoms of depression (hazard ratio = 1.08, 95%CI = 1.01–1.15) are significantly related to mortality in patients with COPD in our sample. Also, the dichotomous variable low/high depressive symptoms (hazard ratio = 1.96, 95%CI = 1.11–3.47) was found to be significantly related to mortality. However, sex, age, marital status, smoking behavior, BMI, and type D nor one of the subscales of the DS16 (i.e., NA and SI) were associated with mortality. Multivariate analysis demonstrates that depressive symptoms (hazard ratio = 1.07, 95%CI = 1.00–1.14) are significantly associated with mortality when adjusted for age, FEV1 %pred, and W peak. When using the adjusted dichotomous low/high depressive symptoms, based on the cut-off level of ≥8, again, we found a significant association with mortality (hazard ratio = 1.98, 95%CI = 1.07–3.69). This is illustrated in Fig. 1 in which the Kaplan–Meier survival curves are shown for the high and low depressive symptoms groups. Sex, marital status, smoking behavior, BMI, and type D were also included but were later removed from the model because they failed to reach statistical significance. We did not find any interaction effects.
The prevalence of the distressed personality (type D) in our sample was 29%. Type D and each subscale considered separately, NA and SI, did not differ significantly between survivors and nonsurvivors. The rate of death did not differ between type D patients (14/35 = 40%) and nontype D patients (34/87 = 39%), chi square p = 0.93. Furthermore, type D was not associated with any of the other predictor variables, except for, as earlier mentioned, depressive symptoms (r = 0.49).
Given the finding that depressive symptoms correlate 0.49 with type D and yet type D was not related to mortality, we undertook a number of exploratory analyses. We tested whether type D was associated with mortality when adjusted for age, FEV1 %pred, and W peak. This multivariate analysis shows that type D was not associated with mortality. Next, we looked at both the components NA and SI in relation to depressive symptoms. The correlation between depressive symptoms and NA is 0.74, as high as the reliabilities of the two scales would allow. However, it is notable that the type D concept involves being above the median splits of both NA and SI subscales. This both excludes 16 patients with substantial depressive symptoms because they did not meet the cut-off on the SI subscale (or the NA subscale) and included 11 patients with relatively low numbers of depressive symptoms who met both cut-off points.
Discussion
This study provides further evidence that depressive symptoms, independent of age, lung function, and exercise capacity, are prognostic factors for mortality in COPD. We found that type D personality is associated with depressive symptoms, but despite this moderate association, type D itself is not a prognostic factor for mortality in COPD.
Two previous studies in samples of patients with COPD who were hospitalized because of a recent exacerbation demonstrated that symptoms of depression were associated with mortality independent of disease severity and other risk factors [26, 27]. It has been argued that the possibility should be considered that these results may be a consequence of the difficulties of distinguishing affective dispositions from patients’ medical conditions [47]. However, one past study found a similar effect in patients with clinically stable COPD [30]. Moreover, in another recent study, we were able to obtain this result in a group of patients with clinically stable COPD in pulmonary rehabilitation. A similar association was found between depressive symptoms, assessed with the BDI and mortality, independent of sex, age, and exercise capacity [31]. It is noteworthy that our finding was in a population of patients with stabilized COPD. Unlike some recent studies in which the assessment of depressive symptoms was following a recent exacerbation of COPD, our results are less obviously the product of a spurious relationship between depressive symptoms and mortality due to a confounding with physical distress that anticipates death. Our median follow-up period was also longer than would be affected by acute illness.
Some sources have argued that, in the assessment of depressive symptoms in patients with cardiovascular disease, scores obtained with instruments like the widely used BDI are inflated among patients with medical disease because of the confounding of vegetative symptoms [48–50]. The HADS is constructed to avoid assessment of somatic symptoms. Still, in the present study, despite the use of a different instrument to assess depressive symptoms, the HADS, we found a similar effect of depressive symptoms on mortality. The fact that the depression–mortality association is consistent in two different groups of patients with stable COPD and with two different assessment tools for symptoms of depression, i.e., BDI and HADS, strengthens the evidence for this relation and adds to the established predictor variables.
With regard to the association of depressive symptoms and mortality, two hypothetical pathways are suggested. One may be through behavioral mechanisms such as that depression leads to low self-care and apathy resulting in avoidance of regular exercise, inadequate nutritional intake, low treatment adherence, and continued smoking, all of which are related to worse prognosis. Another pathway may be that depression affects the hypothalamic pituitary adrenal axis functioning which could deteriorate health status and influence prognosis [51–53]. Evidence is consistent that inflammation occurs among a subset of depressed patients and thus may worsen prognosis in COPD [54]. Still, the depression–mortality relation may still be confounded by other unmeasured factors related to both depressive symptoms and mortality, namely, overall chronic disease burden [55].
Regardless, depressive symptoms represent a burden for patients because of its influence on their quality of life. Elderly persons reporting depressive symptoms are particularly at risk of chronic decline of health [56]. Several studies have reported that major depression is reduced by psychological or antidepressant interventions [57]. Also, pulmonary rehabilitation has been known to reduce depression and improve quality of life [58–60]. Moreover, pulmonary rehabilitation is even potentially beneficial in reducing the risk of mortality [61]. However, there are no studies yet that have established if decrease of depression symptoms in patients with COPD actually reduces the risk for mortality.
In cardiovascular research, Denollet and his coworkers offered type D personality as an explanation of the observed association between depressive symptoms and a variety of cardiovascular outcomes [33, 38, 62]. Although there is evidence for substantial comorbidity between COPD and cardiovascular disease, with smoking and airflow limitation as independent risk factors for mortality [39–41], we did not find that the presence of type D personality was related to mortality at a bivariate level nor in a multivariate model. While type D is correlated with symptoms of depression, it is apparently not a factor which could explain the depression–mortality relation in COPD. Perhaps, although unlikely, type D is specifically associated with cardiovascular morbidity and death.
On the other hand, we have already noted the moderate correlation between depressive symptoms and type D, but that depressive symptoms have a high correlation with one of the components, namely, NA. Use of median splits then to construct typology resulted in some high depressive patients being excluded and some relatively low in depressive symptoms, but still above the median split, being included. Also, Suls and Bunde have presented their concerns on the degree of overlap among different affective dispositions [47]. The degree of overlap may provide a partial explanation for inconsistencies in our study. Despite the high correlation between NA and depressive symptoms, our null effect in the type D mortality association may be a consequence of minimal overlap with the cardiotoxic affect. However, we agree with Suls and Bunde that it is unlikely that this is the sole explanation for the inconsistency [47].
In another context, Maxwell and Delaney have cautioned about the likelihood of spurious results when a typological construct, like type D, is created from two dichotomized variables:
When two (or more) continuous predictor variables are dichotomized, the resulting 2 × 2 analyses are not necessarily conservative. Instead, there is a potential for an effect that is truly zero for a continuous measure to be estimated as a small to medium effect in the 2 × 2 factorial design [63, p. 188].
The present results thus offer no support for pursuing type D as an explanation for COPD mortality. However, it could be important to examine the potential statistical problems with type D construct in cardiovascular disease.
Some limitations of this study should be noted. First, data on the nature and numbers of comorbid conditions were not consistently recorded and, therefore, not included in the study. These data, especially on cardiovascular comorbidities, could have provided us with additional clues on a possible explanatory mechanism of the association between depressive symptoms and mortality and/or the null finding with regard to the type D–mortality association. Second, the cause of death was not determined. Variables in our study are prognostics for all-cause mortality and not just for respiratory causes. However, in studies of all-cause mortality, the actual cause of death is not independently validated and known to be less trustworthy [46]. Third, our study includes several potential modifiable variables, such as smoking behavior, BMI, FEV1, and exercise capacity, which may alter in time. In COPD, patient reported outcomes on health status, dyspnea, and psychological status, as well as physiological outcomes deteriorate over time, but intercorrelations between both types of outcomes are weak [64]. In our study, assessment of depressive symptoms was limited to a single point in time. This assessment leaves unexplored questions about the stability and course over time. However, we believe our assessment allows demonstration of the predictive value of depressive symptoms in COPD. Finally, we observed our findings among patients with clinically stable COPD, which perhaps limits generalization to all patients with COPD. However, taken together with findings of the other studies demonstrating the predictive value of depressive symptoms in COPD, our results give support to further studies on the course of depressive symptoms in relation to mortality.
In conclusion, the present paper provides further evidence for the association of depressive symptoms and mortality. This association may very well reflect confounding by other unmeasured factors [55]. In this study, we did not find that the presence of type D personality is related mortality or that it is a confounder in the depression–mortality relationship in patients with COPD. In contrast to cardiovascular disease, it seems that we can rule out type D as an explanation for the relationship between depressive symptoms and mortality observed in this sample. Further efforts are encouraged to disentangle the relationships found, and more attention should be paid to behavioral and physiological mechanisms.
References
Kubzansky LD, Kawachi I, Weiss ST, Sparrow D. Anxiety and coronary heart disease: A synthesis of epidemiological, psychological, and experimental evidence. Ann Behav Med. 1998; 20: 47-58.
Kubzansky LD, Kawachi I. Going to the heart of the matter: Do negative emotions cause coronary heart disease? J Psychosom Res. 2000; 48: 323-337.
Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychol Bull. 2003; 129: 10-51.
Shen BJ, Avivi YE, Todaro JF, et al. Anxiety characteristics independently and prospectively predict myocardial infarction in men the unique contribution of anxiety among psychologic factors. J Am Coll Cardiol. 2008; 51: 113-119.
Bleil ME, Gianaros PJ, Jennings JR, Flory JD, Manuck SB. Trait negative affect: Toward an integrated model of understanding psychological risk for impairment in cardiac autonomic function. Psychosom Med. 2008; 70: 328-337.
Murphy JM, Monson RR, Olivier DC, Sobol AM, Leighton AH. Affective disorders and mortality. A general population study. Arch Gen Psychiatry. 1987; 44: 473-480.
Wells KB, Rogers W, Burnam MA, Camp P. Course of depression in patients with hypertension, myocardial infarction, or insulin-dependent diabetes. Am J Psychiatry. 1993; 150: 632-638.
Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995; 91: 999-1005.
Lesperance F, Frasure-Smith N, Juneau M, Theroux P. Depression and 1-year prognosis in unstable angina. Arch Intern Med. 2000; 160: 1354-1360.
Rumsfeld JS, Jones PG, Whooley MA, et al. Depression predicts mortality and hospitalization in patients with myocardial infarction complicated by heart failure. Am Heart J. 2005; 150: 961-967.
Carney RM, Freedland KE, Jaffe AS, et al. Depression as a risk factor for post-MI mortality. J Am Coll Cardiol. 2004; 44: 472.
van Manen JG, Bindels PJ, Dekker FW, IJzermans CJ, van der Zee JS, Schade E. Risk of depression in patients with chronic obstructive pulmonary disease and its determinants. Thorax. 2002; 57: 412-416.
van Ede L, Yzermans CJ, Brouwer HJ. Prevalence of depression in patients with chronic obstructive pulmonary disease: A systematic review. Thorax. 1999; 54: 688-692.
Kunik E. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005; 127: 1205.
Maurer J, Rebbapragada V, Borson S, et al. Anxiety and depression in COPD: Current understanding, unanswered questions, and research needs. Chest. 2008; 134: 43S-56S.
Siafakas NM, Vermeire P, Pride NB, et al. Optimal assessment and management of chronic obstructive pulmonary disease (COPD). The European Respiratory Society Task Force. Eur Respir J. 1995; 8: 1398-1420.
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001; 163: 1256-1276.
Hansen EF, Vestbo J, Phanareth K, Kok-Jensen A, Dirksen A. Peak flow as predictor of overall mortality in asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001; 163: 690-693.
Groenewegen KH, Schols AM, Wouters EF. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest. 2003; 124: 459-467.
Nizet TA, van den Elshout FJ, Heijdra YF, van de Ven MJ, Mulder PG, Folgering HT. Survival of chronic hypercapnic COPD patients is predicted by smoking habits, comorbidity, and hypoxemia. Chest. 2005; 127: 1904-1910.
Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002; 121: 1434-1440.
Schols AMWJ, Slangen J, Volovics L, Wouters EFM. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998; 157: 1791-1797.
Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999; 160: 1856-1861.
Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004; 350: 1005-1012.
Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: Role of comorbidities. Eur Respir J. 2006; 28: 1245-1257.
Almagro P, Calbo E, Ochoa-de-Echaguen A, et al. Mortality after hospitalization for COPD. Chest. 2002; 121: 1441-1448.
Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease: Effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007; 167: 60-67.
Yohannes AM, Baldwin RC, Connolly M. Mortality predictors in disabling chronic obstructive pulmonary disease in old age. Age Ageing. 2002; 31: 137-140.
Stage KB, Middelboe T, Pisinger C. Depression and chronic obstructive pulmonary disease (COPD). Impact on survival. Acta Psychiatr Scand. 2005; 111: 320-323.
Fan VS, Ramsey SD, Giardino ND, et al. Sex, depression, and risk of hospitalization and mortality in chronic obstructive pulmonary disease. Arch Intern Med. 2007; 167: 2345-2353.
de Voogd JN, Wempe JB, Koeter GH, et al. Depressive symptoms as predictors of mortality in patients with COPD. Chest. 2009; 135: 619-625.
Denollet J, Sys SU, Stroobant N, Rombouts H, Gillebert TC, Brutsaert DL. Personality as independent predictor of long-term mortality in patients with coronary heart disease. Lancet. 1996; 347: 417-421.
Denollet J, Brutsaert DL. Personality, disease severity, and the risk of long-term cardiac events in patients with a decreased ejection fraction after myocardial infarction. Circulation. 1998; 97: 167-173.
Denollet J, Pedersen SS, Vrints CJ, Conraads VM. Usefulness of type D personality in predicting five-year cardiac events above and beyond concurrent symptoms of stress in patients with coronary heart disease. Am J Cardiol. 2006; 97: 970-973.
Denollet J. Depression, anxiety, and trait negative affect as predictors of cardiac events: Ten years after. Psychosom Med. 2008; 70: 949-951.
Denollet J. Type D personality. A potential risk factor refined. J Psychosom Res. 2000; 49: 255-266.
Denollet J. Personality and coronary heart disease: The type-D scale-16 (DS16). Ann Behav Med. 1998; 20: 209-215.
Denollet J, Van Heck GL. Psychological risk factors in heart disease: What Type D personality is (not) about. J Psychosom Res. 2001; 51: 465-468.
Huiart L, Ernst P, Suissa S. Cardiovascular morbidity and mortality in COPD. Chest. 2005; 128: 2640-2646.
Curkendall SM, DeLuise C, Jones JK, et al. Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada cardiovascular disease in COPD patients. Ann Epidemiol. 2006; 16: 63-70.
Calverley PM, Scott S. Is airway inflammation in chronic obstructive pulmonary disease (COPD) a risk factor for cardiovascular events? COPD. 2006; 3: 233-242.
Pulmonary rehabilitation-1999. American thoracic society. Am J Respir Crit Care Med. 1999; 159: 1666-1682.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67: 361-370.
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J Psychosom Res. 2002; 52: 69-77.
Varray A, Prefaut C. Exercise training in patients with respiratory disease: Procedures and results. Eur Respir Rev. 1995; 5: 25-58.
Gottlieb SS. Dead is dead—Artificial definitions are no substitute. Lancet. 1997; 349: 662-663.
Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychol Bull. 2005; 131: 260-300.
Irvine J, Basinski A, Baker B, et al. Depression and risk of sudden cardiac death after acute myocardial infarction: Testing for the confounding effects of fatigue. Psychosom Med. 1999; 61: 729-737.
Sorensenf C, Friis Hasche E, Haghfelt T, Bech P. Postmyocardial infarction mortality in relation to depression: A systematic critical review. Psychother Psychosom. 2005; 74: 69-80.
de Jonge P, Ormel J, van den Brink RH, et al. Symptom dimensions of depression following myocardial infarction and their relationship with somatic health status and cardiovascular prognosis. Am J Psychiatry. 2006; 163: 138-144.
Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000; 23: 477-501.
Ehlert U, Gaab J, Heinrichs M. Psychoneuroendocrinological contributions to the etiology of depression, posttraumatic stress disorder, and stress-related bodily disorders: The role of the hypothalamus–pituitary–adrenal axis. Biol Psychol. 2001; 57: 141-152.
Rosmond R, Bjorntorp P. The hypothalamic–pituitary–adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. J Intern Med. 2000; 247: 188-197.
Glassman AH, Miller GE. Where there is depression, there is inflammation… sometimes!. Biol Psychiatry. 2007; 62: 280-281.
Macleod J, Davey-Smith G. Psychosocial factors and public health: A suitable case for treatment? J Epidemiol Community Health. 2003; 57: 565-570.
de Jonge P, Ormel J, Slaets JP, et al. Depressive symptoms in elderly patients predict poor adjustment after somatic events. Am J Geriatr Psychiatry. 2004; 12: 57-64.
Gill D, Hatcher S. A systematic review of the treatment of depression with antidepressant drugs in patients who also have a physical illness. J Psychosom Res. 1999; 47: 131-143.
Withers NJ, Rudkin ST, White RJ. Anxiety and depression in severe chronic obstructive pulmonary disease: The effects of pulmonary rehabilitation. J Cardiopulm Rehabil. 1999; 19: 362-365.
Garuti G, Cilione C, Dell’Orso D, et al. Impact of comprehensive pulmonary rehabilitation on anxiety and depression in hospitalized COPD patients. Monaldi Arch Chest Dis. 2003; 59: 56-61.
de Godoy DV, de Godoy RF. A randomized controlled trial of the effect of psychotherapy on anxiety and depression in chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2003; 84: 1154-1157.
Puhan MA, Scharplatz M, Troosters T, Steurer J. Respiratory rehabilitation after acute exacerbation of COPD may reduce risk for readmission and mortality—A systematic review. Respir Res. 2005; 6: 54.
Denollet J, Sys SU, Brutsaert DL. Personality and mortality after myocardial infarction. Psychosom Med. 1995; 57: 582-591.
Maxwell SE, Delaney HD. Bivariate median splits and spurious statistical significance. Psychol Bull. 1993; 113: 181-190.
Oga T, Nishimura K, Tsukino M, Sato S, Hajiro T, Mishima M. Longitudinal deteriorations in patient reported outcomes in patients with COPD. Respir Med. 2007; 101: 146-153.
Acknowledgements
Preparation of this article was funded by the Beatrixoord Foundation, Haren, The Netherlands.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
de Voogd, J.N., Wempe, J.B., Postema, K. et al. More Evidence that Depressive Symptoms Predict Mortality in COPD Patients: Is Type D Personality an Alternative Explanation?. ann. behav. med. 38, 86–93 (2009). https://doi.org/10.1007/s12160-009-9105-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-009-9105-8