Abstract
The well-being and satisfaction of individuals with serious mental illnesses (SMI) and their family caregivers are less than desirable. Research on the quality of life (QoL) of individuals with SMI and their caregivers, including disorders other than schizophrenia, is limited. Thus, this study aimed to investigate the self-perception of QoL in patients with SMI and their family caregivers and the associated factors. This cross-sectional study was conducted in patients with SMI and their caregivers who completed self-assessment instruments to determine their QoL. Social support and burden in caregivers and symptomatology levels in individuals with SMI were assessed. The physical aspect of QoL in individuals with SMI was associated with employment status and symptom severity. The physical component of caregivers’ QoL was associated with kinship relationship, the presence of other family members with disabilities, social support, and age. The mental component was associated with global symptomatology and the diagnosis of major depression in individuals with SMI and caregiver burden in family members. In conclusion, these findings on correlated factors of QoL in individuals with SMI and their caregivers could be used in developing therapeutic interventions for mental health.
Plain summary
A significant number of people with serious mental health problems and their families often endure poor quality of life. However, research on how these individuals truly feel about their lives is limited. This study aimed to explore the perceptions of quality of life among individuals with serious mental health issues and their family caregivers in Spain. We sought to understand the personal sentiments of these individuals and their caregivers regarding their quality of life and the factors that influence it. Our findings indicate that job status, symptoms of the illness, and family relationships play crucial roles in how these individuals view their quality of life. Additionally, caregivers' age, support they receive, and the challenges they face in their families can influence their feelings. This implies that, to enhance their lives, it is crucial to consider these factors and provide appropriate support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quality of life (QoL) is a multifaceted and subjective concept that encompasses numerous human experiences and circumstances, extending beyond well-being. The World Health Organization defines QoL as an individual’s perception of their place in life within their cultural and value systems, considering their goals, expectations, standards, and concerns (Cai et al. 2021). This definition emphasizes the interconnectedness of physical health, psychological state, independence level, environmental factors, and personal beliefs (Pinto et al., 2017; Md Sakip et al., 2023).
Recognizing and addressing difficulties associated with serious mental illness (SMI) requires a deep understanding of the QoL of an individual. SMI refers to serious and long-lasting psychiatric disorders that lead to varying degrees of impairment and social dysfunction. These conditions require effective care and coordination of resources from healthcare and social support systems (Ministry of Health of the Government of Andalusia, 2020). Psychotic episodes, severe functional impairment, and disorders such as schizophrenia, bipolar disorder, major depressive disorder, obsessive–compulsive disorder (OCD), and personality disorders involve persistent behavioral patterns and internal experiences that differ from social norms. These conditions are distinguished by persistent symptoms that can significantly hinder an individual’s ability to perform activities of daily living (Maragakis & Vriesman, 2018).
In the context of SMI, QoL reflects not only the general well-being of individuals but also how they navigate and manage the challenges posed by their mental health conditions, including their ability to maintain social relationships, achieve personal goals, and cope with the daily demands of life (Grover & Sahoo, 2022). Families supporting individuals with SMI often cope with home care of their family members as their main source of support (de Jacq et al., 2016). Consequently, it can affect QoL of family caregivers, resulting in difficulties in social and occupational development, along with psychological reactions, such as anxiety, depression and feelings of frustration, anger, and discomfort (Cirici Amell et al., 2018).
In Spain, approximately 6.08 per 1000 people receiving mental health services have SMI. Various factors, such as the duration of service use, substance abuse, and psychological symptoms, are associated with SMI. SMI can affect higher mental functions, such as thoughts, beliefs, perceptions, volition, and emotions, leading to cognitive impairment, that is, distress or damage (Stoyanova & Pinilla 2019). A study in Spain found that most patients with SMI were prescribed antipsychotics and approximately 70% took multiple types (Martín-Pérez et al., 2019; Orrico-Sánchez et al., 2020; Stoyanova & Pinilla, 2019). SMI significantly impacts healthcare use and increases the demand for mental health services during economic crises, resulting in barriers to access and a noticeable gap in formal access to mental healthcare (Launders et al. 2023). Research on epidemiology and mental health services is crucial for developing effective policies and helping individuals with SMI (Buoli, 2023).
QoL is a relevant outcome assessment method for both research and treatment and is a particularly significant treatment goal in this population (Folsom et al., 2009). It has been extensively studied and found to be unsatisfactory in individuals with SMI and their caregivers (Tang & Wu, 2012). Given the higher rates of medical comorbidity and premature mortality associated with this population compared with the general population, prioritizing improving QoL is of utmost importance. This can be achieved by adopting a comprehensive definition of health that encompasses both physical and mental well-being (Folsom et al., 2009). In individuals with SMI, previous studies have examined the relationship between QoL and symptoms. Saavedra et al. (2023) found that psychiatric distress negatively affects QoL; however, recovery can have a positive effect. Barnes et al. (2012) demonstrated that physical and mental health related QoL are separate factors in individuals with SMI. Furthermore, research has highlighted the connection between poor functional outcomes, lower QoL and symptomatology in older adults with SMI (Bartels & Pratt, 2009). However, the current understanding of the interaction among various factors in different cultural and social settings, particularly in Spain, is limited. Although some studies have identified similar trends, the extent and characteristics of these connections are not yet clarified in diverse communities.
The QoL of family members of individuals with SMI was to be found significantly worse than that of the general population (Leng et al., 2019). Clinical knowledge establishes several factors that influence QoL, including degree of kinship (Noghani, 2016), employment status (ZamZam et al., 2011), social support (Leng et al., 2019), caregiver burden (Johansson et al., 2015), symptom status (Leng et al., 2019) and depressive symptoms (Johansson et al., 2015). Studies have shown that close kinship and unstable employment have negative effects on QoL, whereas strong social support and employment stability have positive effects. In addition, greater caregiver burden and depressive symptoms are associated with lower QoL for both caregivers and patients.
Previous studies have highlighted a negative correlation between caregiver burden and QoL of both caregivers and patients, indicating that increased caregiver stress adversely affects both parties’ well-being and reduces physical, psychological, social, and environmental QoL (Johansson et al., 2015; Kate et al., 2013; Li et al., 2007; Zauszniewski et al., 2009). Chou et al. (2009) found that a high level of perceived family support, in terms of instrumental, emotional, and informational support, increases the QoL of relatives. These findings indicate that greater family support improves QoL, whereas caregiver burden worsens it. However, no studies have evaluated the interaction of these factors in the context of SMI in Spain.
Therefore, the QoL of Spanish individuals with SMI and their family members should be investigated. This is particularly relevant due to the family-centric care approach in Spain, which can reveal different manifestations and effects of SMI in both patients and caregivers. Healthcare system and societal structure disparities in Spain, North America, and Northern Europe warrant further investigation (Kokorelias et al., 2019). Focusing on the Spanish context, this study addresses a significant gap in the literature and provides insights into the development of culturally sensitive and effective mental health interventions (Bouza et al., 2010).
Given the chronic nature of SMI, mental health professionals who wish to implement interventions for this population may want to identify potential correlations with QoL. Understanding how these factors are related to QoL may provide relevant details for mental health professionals on potentially helpful interventions to improve QoL. Several studies have examined factors associated with QoL in individuals with SMI (Berghöfer et al., 2020; Dong et al., 2019) or their family caregivers (Noghani 2016; ZamZam et al., 2011; Zhang et al., 2021). However, the focus on evaluating QoL in a group comprising caregivers and patients with SMI is limited, including disorders other than schizophrenia, such as bipolar disorder, major depressive disorder, OCD, and personality disorders.
Previous research on individuals with SMI and their caregivers has mainly focused on illness-related aspects. However, QoL studies provide a more comprehensive perspective, which aligns with the emphasis of the recovery model on the lived experiences of patients and their families (Lau & Hutchinson, 2021). This holistic approach integrates patient-centered factors, such as psychosocial and cultural, and emphasizes patient empowerment and autonomy. Understanding caregiver QoL is crucial for their well-being and the effectiveness of their care, which, in turn, affects the patient QoL (Deek et al., 2016). Despite existing research gaps, QoL, social support, caregiver burden, and symptomatology remain to be explored in the context of SMI in Spain (Menzies & Menzies, 2020).
The proposed research is not only a response to the identified need for localized studies but also an effort to enrich the broader discourse on mental healthcare, making it a novel and significant contribution to the field. Consequently, the present study aimed to determine the self-perceived QoL of patients with SMI and their caregivers, along with related factors, filling a significant gap in the existing literature while providing unique perspectives tailored to the Spanish context.
Methods
Participants and procedures
The Strengthening the Reporting of Observational Studies in Epidemiology guidelines (Sharp et al., 2019) were followed to conduct this cross-sectional study. These guidelines promote transparency and accuracy by focusing on methods, population, data collection, and statistical analysis. In 2018, data were collected from individuals who attended multidisciplinary care programs for SMI in Andalusia, Extremadura, Cantabria, and the Balearic Islands. Participants were recruited from the Mental Health Day Hospital and various other facilities, including the Psychosocial Rehabilitation Center, Community Mental Health Unit, Occupational Rehabilitation Unit, Eating Disorders Unit, Medium Stay Unit, Brief Hospitalization Unit, and other similar centers. This multisite approach provided a diverse and representative sample, offering a broad perspective on QoL determinants for individuals with SMI and their caregivers in various healthcare settings in Spain.
This study included 105 adults with schizophrenia, schizotypal disorders, and delusional, affective, and personality disorders (SMI) and 86 family caregivers. Using G*Power software with sample size estimation for bivariate correlations, bilateral contrast, mean size effect (0.5), type I error of 5% and 80% power, the sample size was found sufficient to obtain adequate statistical power.
A non-probabilistic quota sampling approach was used, which provides specific subgroup representativeness, is efficient, and allows researchers to control sample composition. Prevalence studies in the Spanish population reported that 52% of patients had schizophrenia and OCD-related disorders, 35% had affective disorders, and 13% had personality disorders (Disability Observatory, 2003). In our study, specific criteria were set for the inclusion and exclusion of participants to ensure a representative sample. Participants were required to have a formal diagnosis of SMI.
In our study, specific criteria were set for the inclusion and exclusion of participants to ensure a representative sample. Participants were required to have a formal diagnosis of SMI for at least 2 years, must be of legal age (18 years) and understand Spanish. They needed to be able to provide informed consent and be in the stable phase of their illness. The exclusion criteria were significant cognitive impairments that could interfere with understanding the study or providing informed consent, severe communication difficulties, and active substance abuse or dependence. No further exclusion criteria were applied beyond these parameters.
Data collection and measurements
We contacted 30 mental health organizations and facilities throughout Spain, including both the public and private sectors, in urban and rural settings to ensure diversity. These organizations were selected based on their services to individuals with SMI and their geographic distribution throughout the country. Our recruitment strategies involved sending detailed emails and making phone calls to explain the purpose and requirements of the study. Once they agreed to participate, each organization received a research project package containing an overview of the study, its objectives, and specific questionnaires. To effectively reach potential participants, both passive methods, such as placing informational posters within participating organizations, and active methods, such as contacting interested individuals directly from the databases of organizations that met our inclusion criteria, were used. An experienced researcher was responsible for coordinating these efforts to personally invite potential participants while ensuring that full information about confidentiality agreements was shared. In cases where organizations participated electronically, specific links tailored to two distinct groups, one for individuals with SMI and another for family caregivers, were provided, allowing those facing geographical or logistical constraints to conveniently answer online questionnaires. Our comprehensive recruitment strategies ensured a representative sample reflecting varied experiences across Spain.
The questionnaire for people with SMI and family members includes information about sociodemographic data and relevant scales. Sociodemographic data (age measured by years, sex [male or female] and employment situation [employed or unemployed]) were collected from both population groups. In addition, family characteristics were requested from family members (kinship [partner or spouse, child, sibling, or parent], if they live with the person with SMI [yes or no] and if there are other family members with disabilities [yes or no]).
SF-12 Health questionnaire
QoL was assessed in people with SMI and family members using the SF-12 Health Questionnaire (Huo et al., 2018), comprising 12 items in eight dimensions of health status dimensions with a score of 0–100 for each dimension: physical functioning (PF), role-physical (RP), role-emotional (RE), mental health (MH), bodily pain (BP), general health (GH), vitality (VT) and social functioning (SF). Factor analyses showed that the eight scales defined two main health components: physical and mental summary. Norm-based scores were used, and this approach has the advantage that the results are directly interpretable: scores > 50 or < 50 indicate better or worse health status, respectively, compared to the mean of the reference population. Vera-Villarroel et al. (2014) conducted interitem correlation, internal consistency (α = 0.74), exploratory factor, and external validity analyses in Spain. The Cronbach's alpha values obtained in this study were 0.82 for the total sample, 0.78 for individuals with SMI and 0.85 for family members.
Symptom assessment-45
Symptom Assessment-45 (Maruish, 2004) was used to measure the psychopathological state of patients with SMI, consisting of 45 items clustered into nine symptom scales somatization obsession–compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism). This instrument ranks symptoms with equally spaced categories, making it easier to assess severity on different scales. Higher scores indicate more severe symptoms, providing a clear measure for evaluating symptom intensity. The internal consistency of this scale was determined to be good, with a Cronbach’s α value of 0.95 (Holgado Tello et al., 2019). Specifically, Cronbach’s α value obtained for the sample under investigation was 0.95.
Functional social support duke-UNC-11
Perceived social support was measured in family members using Duke-UNC Functional Social Support with 11 items scored from 1 to 5 on a Likert scale (Broadhead et al., 1988). This ordinal scale ranks items based on their relative position, offering a discernible order of magnitude despite the challenges of precise quantification. It is particularly useful for subjective assessments in which clear distinctions can be made; however, precise measurements are difficult to obtain. The scores ranged from 11 to 55 points, indicating low perceived social support if it was < 32. The questionnaire was determined to have acceptable reliability within the Spanish population, with a Cronbach’s α value of 0.86 (Cuéllar-Flores & Dresch, 2012), and our investigation produced a value of 0.89, signifying high reliability.
Zarit burden interview
To assess the caregiver burden on family members, the Zarit burden interview was used, consisting of a 22-point Likert scale. The scale is then used to classify the burden level into separate ordered groups, with ≤ 46, 47–55 or ≥ 56 indicating no, moderate, or severe burden, respectively (Ribé Buitrón et al., 2018). The original study reported a Cronbach’s α value of 0.91 (Tang et al., 2017), and the value obtained in the present study was 0.86, indicating high reliability.
Data analysis
Data analysis was performed in two phases: descriptive and inferential (p < 0.05). There were no data missing for the survey. The Kolmogorov–Smirnov test determined a non-normal QoL distribution. Spearman's non-parametric correlation coefficient was used. The effect size (ES) was obtained through r, considering a coefficient of 0.10–0.30 to be small, 0.30–0.50 to be moderate and > 0.50 to be large (Funder & Ozer, 2019). The Kruskal–Wallis’ test was used to determine significant differences among qualitative variables. To perform multivariate analysis, the stepwise and backward regression approach was used on significantly related variables, checking for linearity, homoscedasticity, normality, and non-collinearity. For the evaluation of the model, the Snedecor F statistic was used. ES was calculated using adjusted R2 (low ES, 0.01; medium ES, 0.10; and large ES, 0.25) and β-coefficients (ES of < 0.20, weak; 0.2–0.50, moderate; and > 0.50, strong; Dominguez-Lara, 2018).
Multiple regression analysis was considered to assess significantly different multiple predictors with different measurement scales, which were considered dummy or numeric factors, measured using scales. Correlations were previously explored to identify multicollinearity issues. By considering potential confounders, multiple regression analysis improves our understanding of unique QoL-related factors for people with SMI and their caregivers. Furthermore, the reporting of ESs and β coefficients provides clear insights into the relationship between variables. The ability of this method to handle non-normal distributions underscores its suitability for our dataset.
Results
Sociodemographic and personal characteristics
Among SMI-affected individuals, the majority were men (58.1%), unemployed (43.6%) or had permanent disability (26.7%). Most of the caregivers were women (55.8%), who were working (31.4%) or retired (32.6%). The vast majority (83.7%) lived with an individual with SMI and had a parental relationship (53.5%). Furthermore, 22.1% reported other family members with disabilities (Supplementary Table 1).
The study revealed that family caregivers had higher QoL than individuals with SMI, as well as higher scores on the dimensions of SF, role enjoyment (RE), MH, and summary mental components. Additionally, family caregivers reported a low burden (mean, 48.85; SD, 1.59) and appropriate social support (mean, 38.45; SD, 1.09). The quantitative variables are summarized in Supplementary Table 2.
Bivariate analysis
Among individuals with SMI, significant sex differences were found in PF (Χ2 = 4.99, p < 0.05), RP (Χ2 = 4.82, p < 0.05) and RE (Χ2 = 9.18, p < 0.01), which were lower in women. RP (Χ2 = 11.81, p < 0.05), VT (Χ2 = 14.61, p < 0.01) and the physical component (Χ2 = 12.06, p < 0.05) QoL dimensions were lower in the homemaker group but higher in the retirement group. Regarding diagnosis, significant differences were found in RP (Χ2 = 11.50, p < 0.05), MH (Χ2 = 10.17, p < 0.05) and mental component (Χ2 = 10.78, p < 0.05), which were lower in BPD, OCD, and major depression. In the correlational analysis (Table 1), QoL were significantly associated with each other, with ES ranging from small to large and lower levels of symptomatology in all nine dimensions (ES from small to large).
In caregivers, significant sex differences were found in PF (Χ2 = 5.71), RP (Χ2 = 4.98, p < 0.05), BP (Χ2 = 4.85, p < 0.05), GH (Χ2 = 6.46, p < 0.05) and the physical summary component (Χ2 = 6.31, p < 0.05) of QoL, which were lower in women. Homemakers and those with permanent disabilities had lower levels of PF (Χ2 = 17.05, p < 0.01), GH (Χ2 = 10.29, p < 0.05) and MH levels (Χ2 = 11.25, p < 0.05). Based on the kinship relationship, parents perceived worse PF (Χ2 = 14.03, p < 0.05), RP (Χ2 = 12.54, p < 0.05), BP (Χ2 = 14.08, p < 0.05), GH (Χ2 = 11.99, p < 0.05), SF (Χ2 = 8.37, p < 0.05) and summary physical component levels (Χ2 = 14.99, p < 0.05). Finally, when other family members with disabilities were present, the RP of the family members’ RP (Χ2 = 5.80, p < 0.05) and the summary physical component (Χ2 = 5.99, p < 0.05) were low. In the correlation analysis (Table 2), higher QoL was associated with younger age, higher perceived social support (small and medium SE), and lower levels of caregiver burden (small to large SE).
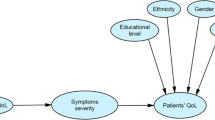
In Fig. 1, scatterplots graphically depict the salient associations revealed (Fig. 1). These visualizations offer a clear and intuitive depiction of interconnections between the investigated variables: Individuals with SMI who experience more severe symptoms tend to have lower physical and mental QoL. In contrast, caregivers who received more social support tended to have better physical QoL. However, those with a higher caregiver burden tended to have a poorer mental QoL. The mental component of the graphs reveals a more pronounced trend, indicating a more pronounced tension between symptomatology and mental QoL as well as between caregiver burden and mental QoL.
Patients with SMI
Multivariate analysis
For those with SMI, the multivariate model for the physical component of QoL (Table 3) was composed of four independent variables: permanent disability status (β = − 8.00), homemakers (β = − 13.53), symptomatology (β = − 0.09) (all with moderate ES) and being unemployed (β = − 4.22) (weak ES). The adjusted R2 value of the model was moderate (0.23). Two predictor variables were identified for the mental component: global symptomatology (β = − 0.21) (strong ES) and major depression diagnosis (β = − 8.26) (weak ES). The adjusted R2 of the model was large (0.30).
Among the family caregivers, the model for the physical component of QoL (Table 4) consisted of five independent variables: the presence of other family members with disability (β = − 7.47), social support (β = 0.27), partner relationship (β = 7.39), sibling relationship (β = 6.90) (all with moderate ES) and age (β = − 0.14) (weak ES). Together, these variables partially explain the variability. Although the age and sibling relationships were not statistically significant, they were considered confounding variables when attempting to remove them from the model. The adjusted value of R2 for the model was moderate (0.23). For the mental component of QoL, the model consisted of one predictor variable, caregiver burden (moderate ES). Each additional point in the caregiver burden worsened the summary mental component by 0.50 points. The adjusted R2 value of the model was moderate (0.22).
Discussion
Our study investigated the sociodemographic and personal characteristics of patients with SMI and their caregivers, focusing on QoL. Most of the patients with SMI were male, unemployed, or disabled, while most caregivers were female, employed, or retired. Surprisingly, caregivers reported a higher QoL than patients with SMI. Bivariate and multivariate analyses revealed significant differences in QoL according to sex, employment status, diagnosis, and family relationships. These findings provide insight into the factors that influence QoL for individuals with SMI and their caregivers and contribute to a better understanding of this population. This study aimed to assess the QoL of families with a member with SMI while identifying associated factors. This study stands out for its comprehensive examination of QoL in individuals diagnosed with various forms of SMI in Spain. Going beyond the typical focus on schizophrenia reflects a broader perspective that aligns with an evolving MH paradigm advocating a more inclusive understanding that encompasses diverse diagnoses associated with SMI.
The main QoL determinants in individuals with SMI were symptomatology, employment status (physical component) and diagnosis and symptomatology (mental component). Concerning caregivers, kinship, age, social support, presence of other disabled family members (physical component) and burden (mental component) were the main determinants of QoL.
In both groups, all QoL dimensions were lower than the cut-off points in the general population, especially in patients with GH, social function, emotional role and mental component (50). Other authors have also found poor QoL in a similar sample (Noghani, 2016). SMI is chronic and often leads to significant limitations for the affected person and a considerable burden on the family, resulting in a lower QoL (Leng et al., 2019). The caregiver group scored higher on QoL. Lower self-perception in individuals with SMI may be due to their symptomatology and limitations in well-being caused by their disability (Tang & Wu, 2012).
The results of the regression analysis performed on individuals with SMI showed a model consisting of four predictor variables for the physical component of QoL: permanent disability, homemaker status, symptomatology, and unemployment. The model for the mental component of QoL comprised symptomatology and major depression diagnosis. QoL was lower for homemakers than for retirees. Homemakers are often faced with the responsibility of continuous, unpaid care work, which may explain their perceived distress. The findings for retirees were surprising because they typically have poorer levels of perceived health, due to their older age. This result could be attributed to fewer responsibilities associated with this condition (Son, 2020). Furthermore, low QoL levels are consistent in individuals who are unemployed or with a permanent disability due to economic difficulties, reduced social support networks, and negative consequences for self-concept associated with these circumstances (Leng et al., 2019). These findings are consistent with those of a previous study that detected worse QoL outcomes in individuals with major depression than in those with other SMIs (Mosqueiro et al., 2015). The cognitive triad of major depression, characterized by negative self-perceptions, pessimistic worldviews, and a bleak outlook on the future, can have a profound impact on an individual’s overall well-being (Keser et al., 2020). QoL is also associated with lower levels of symptomatology. SMI often leads to lower global functioning when the symptomatology is high (social, cognitive, emotional, and physical). Because of the disease, they often withdraw from social contact and lose their previous role, resulting in a worsening of self-concept and symptomatology that deteriorates the functional level of an individual (Leonhardt et al., 2017).
Regarding the physical component of QoL in caregivers, the results revealed five predictor variables: the presence of other family members with disabilities, social support, partner and sibling relationships, and age. Given the presence of other family members with disabilities other than SMI, family members experience a decrease in their QoL. Along these lines, ZamZam et al. (2011) also argued that having two or more dependent family members is related to poorer QoL in caregivers, who find themselves in the position of providing a wider range of care, compromising their well-being. Increased social support was positively associated with QoL. Furthermore, Leng et al. (2019) revealed that better perceived social support, encompassing instrumental, emotional, and informational support, leads to an improvement in caregiver QoL. Bernabéu-Álvarez et al. (2020) reported that social support plays an important role in caregivers as it increases emotional well-being, thereby leading them to feel better and perceive their environment positively. Based on the relationship between kinship and SMI, parents had a lower QoL. Several studies have shown that being a parent, as opposed to having any other relationship with an individual with SMI, is associated with a worse QoL in all dimensions (Boyer et al., 2012; Lua & Bakar, 2011; Margetic et al., 2013). Parents often care for their children with SMI, going as far as health services cannot. Compared to other kinship relationships, greater emotional involvement and attachment between parents and their children can increase concerns about relapses, feelings of personal responsibility for the disease, and concerns about the future of their relatives (Noghani 2016).
In the multivariate analysis of the mental component of QoL, a higher caregiver burden was the unique factor related to this with QoL. Johansson et al. (2015) found that family problems and changes were associated with poorer QoL. Moreover, negative feelings and relative MH status (caregiver burden) were associated with lower QoL. Relatives can experience a burden in providing care for their relatives, in addition to household duties and other family responsibilities (Leng et al., 2019). Despite being excluded in multivariate analysis, the female sex was associated with a lower QoL for caregivers. This reflects the trend in the general population, that is, women have a lower quality of life than men, probably because of socialization by sex on health and well-being (Gumà et al., 2015).
Limitations and strengths
Given its descriptive nature, this study prevented a cause–effect relationship from being established, making it difficult to explain every factor that determines the situation investigated. Furthermore, the instruments used were generic self-reported measures that reflected the perceptions and feelings of the participants at one point in time. Nonprobability quota sampling also has limitations, such as no randomization researcher bias and difficulty generalizing the results to the population. Longitudinal studies should be conducted in the future to further investigate these relationships.
The sample size was determined using correlation analysis, a simple and widely applicable method for initial study planning. However, to understand the unique factors associated with QoL, multiple linear regressions were used for the primary analysis. To ensure the adequacy of our sample size for this complex analysis, a post hoc power analysis was performed considering various factors, such as predictor variables in our regression model, and ES was anticipated from previous literature. The results showed that our sample size was sufficient to attain an acceptable power level (usually set at 0.80) to detect significant relationships within a multiple regression framework. This approach allowed us to adequately test the hypotheses, despite initially estimating the sample size based on correlation alone. Furthermore, using multiple linear regression provided a more refined understanding of the factors affecting the QoL of individuals with SMI and their caregivers, enhancing both the depth and validity of the findings and contributing to a comprehensive understanding of the subject matter.
However, this study has crucial practical implications. QoL was investigated from the perspective of a broad construct, such as SMI, allowing it to be studied outside prototypical diagnostic categories such as schizophrenia spectrum disorders. Considering QoL as a variable associated with both physical and mental well-being brings a positive vision to the study of this phenomenon by associating it with other variables associated with subjective discomfort (burden and symptomatology) following the recovery model. The focus of our study on the physical and mental components of QoL for both caregivers and patients with SMI offers a comprehensive perspective on their well-being. This approach underscores the importance of addressing both aspects of mental health. This holistic view aligns with contemporary trends in MH treatment, which promote a more comprehensive and multidimensional understanding of patient and caregiver needs. By examining the interrelated nature of physical and mental QoL, our study emphasizes their collective influence on overall well-being.
The novelty of our study lies in its comprehensive examination of QoL within the dual framework of patients with SMI and their caregivers in Spain, a perspective that has not been investigated in previous studies. This approach enables a more holistic understanding of the impact of SMI, paving the way for interventions that align with the specific needs and circumstances of this population. This study was, by far, the first to investigate QoL and its determinants in a heterogeneous sample in terms of diagnostic groups of individuals with SMI and their caregivers in a Spanish context, providing a broad overview of the physical and MH of this population, which is consistent with the recovery model in MH (Pinto et al., 2017). Our study provides a distinctive and insightful perspective on the disparate influence of various elements on QoL among diverse diagnostic categories within the extensive spectrum of SMI. This discernibility is of paramount importance in designing customized interventions to address the specific requirements of each subgroup within the SMI cohort.
Conclusion and implications for practice
Several factors have been identified to affect the physical and mental well-being of individuals with SMI and their caregivers. These factors include symptoms, employment status, diagnosis, family relationships, age, social support, presence of other disabled family members, and caregiver burden. This study is groundbreaking in its scope, providing information on multiple elements that influence the QoL of individuals with SMI and their caregivers. This is the first study to determine QoL determinants based on the global SMI construct in Spain.
The findings of this study have significant implications for recovery-oriented care. This study emphasizes the importance of individualized care plans that consider various factors affecting the QoL of individuals with SMI and their caregivers. These findings highlight the need for a holistic approach that addresses physical and mental health needs and improves social support networks. Educational interventions and collaborative care models are crucial to improving the effectiveness of mental healthcare, as indicated in our study. Regular monitoring and evaluation of QoL as part of care adheres to the principles of recovery-oriented practice and ensures that interventions remain responsive and adaptive to the evolving needs of patients and caregivers. This study emphasizes the importance of a nuanced, patient-centered approach to MH, which is essential for achieving better outcomes in the care of individuals with SMI and their caregivers (Agustina et al., 2019; Vecchi et al., 2015).
This may provide a basis for future studies to determine the direction of cause–effect relationships. Future studies can establish the associations found by determining cause–effect relationships, studying changes in outcomes over time, exploring other populations, and areas of applicability. Support networks, such as support groups, family therapies, and community programs, can help individuals with SMI access resources and connect with other families. The present study aligns with current trends in mental healthcare by focusing on a holistic perspective on QoL, thus promoting a more comprehensive appreciation of the needs of patients and their caregivers.
This study provided baseline data that could be used by MH professionals to assess the QoL, clinical state, and burden of patients with SMI and their caregivers and to track progress throughout recovery. These findings can also be used to develop therapeutic interventions for MH in individuals with SMI and their families. Interventions to reduce caregiver burden, such as education on SMI, stress management, and coping skills, can benefit caregivers and individuals with SMI. A population presenting with nonmodifiable factors could be considered a target group for individualized healthcare. On the contrary, focusing on modifiable factors will allow for the treatment of these factors and the improvement of the health status of the individuals receiving care. It may be worthwhile to intervene in QoL, especially in individuals with predictive factors for worsening QoL, as it may be associated with lower levels of psychiatric symptoms in individuals with SMI, greater perceived social support, and lower caregiver burden. This study emphasizes the need to look beyond traditional diagnostic categories for more comprehensive recovery-oriented care. It also sets the stage for future research and guides MH interventions. These findings should be used by MH professionals to improve the care provided to patients with SMI and their families.
Data availability
Data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Agustina, H. S., Suryani, S., & Widianti, E. (2019). Nurses’ life experiences as persons in charge of mental health programs in community health center. Jurnal Keperawatan Padjadjaran, 7(2), 200–210. https://doi.org/10.24198/jkp.v7i2.1113
Barnes, A. L., Murphy, M. E., Fowler, C. A., & Rempfer, M. V. (2012). Health-related quality of life and overall life satisfaction in people with serious mental illness. Schizophrenia Research and Treatment, 2012, 245103. https://doi.org/10.1155/2012/245103
Bartels, S. J., & Pratt, S. I. (2009). Psychosocial rehabilitation and quality of life for older adults with serious mental illness: Recent findings and future research directions. Current Opinion in Psychiatry, 22(4), 381–385. https://doi.org/10.1097/YCO.0b013e32832c9234
Berghöfer, A., Martin, L., Hense, S., Weinmann, S., & Roll, S. (2020). Quality of life in patients with severe mental illness: A cross-sectional survey in an integrated outpatient health care model. Quality of Life Research, 29(8), 2073–2087. https://doi.org/10.1007/s11136-020-02470-0
Bernabéu-Álvarez, C., Faus-Sanoguera, M., Lima-Serrano, M., & Lima-Rodríguez, J. S. (2020). Systematic review: Influence of self-help groups on family caregivers. Enfermería Global, 58, 576–590.
Bouza, C., López-Cuadrado, T., & Amate, J. M. (2010). Physical disease in schizophrenia: A population-based analysis in Spain. BMC Public Health, 10(1), 745. https://doi.org/10.1186/1471-2458-10-745
Boyer, L., Caqueo-Urízar, A., Richieri, R., Lancon, C., Gutiérrez-Maldonado, J., & Auquier, P. (2012). Quality of life among caregivers of patients with schizophrenia: A cross-cultural comparison of Chilean and French families. BMC Family Practice, 13, 42. https://doi.org/10.1186/1471-2296-13-42
Broadhead, W. E., Gehlbach, S. H., De Gruy, F. V., & Kaplan, B. H. (1988). The duke-UNC functional social support questionnaire: Measurement of social support in family medicine patients. Medical Care, 26(7), 709–723. https://doi.org/10.1097/00005650-198807000-00006
Buoli, M. (2023). New research horizons of epidemiology applied to mental health. Recenti Progressi in Medicina, 114(6), 380–381. https://doi.org/10.1701/4042.40235
Cai, T., Verze, P., & Bjerklund Johansen, T. E. (2021). The quality of life definition: where are we going? Uro, 1(1), 14–22. https://doi.org/10.3390/uro1010003
Chou, Y. C., Pu, C. Y., Lee, Y. C., Lin, L. C., & Kröger, T. (2009). Effect of perceived stigmatization on the quality of life among ageing female family carers: A comparison of carers of adults with intellectual disability and carers of adults with mental illness. Journal of Intellectual Disability Research, 53(7), 654–664. https://doi.org/10.1111/j.1365-2788.2009.01173.x
Cirici Amell, R., Cobo, J., Martí Castanyer, M., & Giménez Gómez, N. (2018). Gender and other factors influencing the burden of care in relatives of people diagnosed with schizophrenia and schizophrenia spectrum disorders. International Journal of Culture and Mental Health, 11(4), 638–652. https://doi.org/10.1080/17542863.2018.1479764
Cuéllar-Flores, I., & Dresch, V. (2012). Validación del cuestionario de apoyo Social funcional Duke-UNK-11 en personas cuidadoras. Revista Iberoamericana De Diagnóstico y Evaluación-e Avaliação Psicológica, 2(34), 89–101.
de Jacq, K., Norful, A. A., & Larson, E. (2016). The variability of nursing attitudes toward mental illness: An integrative review. Archives of Psychiatric Nursing, 30(6), 788–796. https://doi.org/10.1016/j.apnu.2016.07.004
De Vecchi, N., Kenny, A., & Kidd, S. (2015). Stakeholder views on a recovery-oriented psychiatric rehabilitation art therapy program in a rural Australian mental health service: A qualitative description. International Journal of Mental Health Systems, 9, 11. https://doi.org/10.1186/s13033-015-0005-y
Deek, H., Hamilton, S., Brown, N., Inglis, S. C., Digiacomo, M., Newton, P. J., Noureddine, S., MacDonald, P. S., Davidson, P. M., F.A.A.A.A.Y. Project Investigators. (2016). Family-centred approaches to healthcare interventions in chronic diseases in adults: A quantitative systematic review. Journal of Advanced Nursing, 72(5), 968–979. https://doi.org/10.1111/jan.12885
Disability Observatory. (2003). Population with severe and prolonged mental illness. Ministry of labor and social affairs.
Dominguez-Lara, S. (2018). Magnitud del efecto, una guía rápida. Educación Médica, 19(4), 251–254. https://doi.org/10.1016/j.edumed.2017.07.002
Dong, M., Lu, L., Zhang, L., Zhang, Y. S., Ng, C. H., Ungvari, G. S., Li, G., Meng, X., Wang, G., & Xiang, Y. T. (2019). Quality of life in schizophrenia: A meta-analysis of comparative studies. The Psychiatric Quarterly, 90(3), 519–532. https://doi.org/10.1007/s11126-019-09633-4
Folsom, D. P., Depp, C., Palmer, B. W., Mausbach, B. T., Golshan, S., Fellows, I., Cardenas, V., Patterson, T. L., Kraemer, H. C., & Jeste, D. V. (2009). Physical and mental health-related quality of life among older people with schizophrenia. Schizophrenia Research, 108(1–3), 207–213. https://doi.org/10.1016/j.schres.2008.12.008
Funder DC, Ozer DJ (2019) Evaluating effect size in psychological research: Sense and nonsense. Advances in Methods and Practices in Psychological Science, 2(2), 156–168. https://doi.org/10.1177/2515245919847202
Grover, S., & Sahoo, S. (2022). Optimising Patient Care in psychiatry–focus on quality of life. In Handbook on optimizing Patient Care in psychiatry. Routledge. https://doi.org/10.4324/9780429030260-3
Gumà, J., Treviño, R., & Cámara, A. D. (2015). Posición en el hogar y género. Desigualdades en la calidad de vida relacionada con la salud entre la población adulta en España. Revista Internacional de Sociología, 73(1), 1–17. https://doi.org/10.3989/2013.03.04
Holgado Tello, F. P., Vila Abad, E., & Barbero Garcia, M. I. (2019). Factor structure of the symptom Assessment-45 questionnaire (Sa-45). Acción Psicológica, 16(1), 31–42. https://doi.org/10.5944/ap.16.1.22048
Huo, T., Guo, Y., Shenkman, E., & Muller, K. (2018). Assessing the reliability of the short form 12 (SF-12) health survey in adults with mental health conditions: A report from the wellness incentive and navigation (WIN) study. Health and Quality of Life Outcomes, 16(1), 34. https://doi.org/10.1186/s12955-018-0858-2
Johansson, A., Ewertzon, M., Andershed, B., Anderzen-Carlsson, A., Nasic, S., & Ahlin, A. (2015). Health-related quality of life—From the perspective of mothers and fathers of adult children suffering from long-term mental disorders. Archives of Psychiatric Nursing, 29(3), 180–185. https://doi.org/10.1016/j.apnu.2015.02.002
Kate, N., Grover, S., Kulhara, P., & Nehra, R. (2013). Relationship of caregiver burden with coping strategies, social support, psychological morbidity, and quality of life in the caregivers of schizophrenia. Asian Journal of Psychiatry, 6(5), 380–388. https://doi.org/10.1016/j.ajp.2013.03.014
Keser, E., Kahya, Y., & Akın, B. (2020). Stress generation hypothesis of depressive symptoms in interpersonal stressful life events: The roles of cognitive triad and coping styles via structural equation modeling. Current Psychology, 39(1), 174–182. https://doi.org/10.1007/s12144-017-9744-z
Kokorelias, K. M., Gignac, M. A. M., Naglie, G., & Cameron, J. I. (2019). Towards a universal model of family centered care: A scoping review. BMC Health Services Research, 19(1), 564. https://doi.org/10.1186/s12913-019-4394-5
Lau, R., & Hutchinson, A. (2021). Mental health service users’ lived experiences of recovery-oriented services: A scoping review. Mental Health Review Journal, 26(4), 403–423. https://doi.org/10.1108/MHRJ-09-2020-0064
Launders, N., Hayes, J. F., Price, G., Marston, L., & Osborn, D. P. (2023). The incidence rate of planned and emergency physical health hospital admissions in people diagnosed with severe mental illness: a cohort study. Psychological medicine, 53(12), 5603–5614. https://doi.org/10.1017/S0033291722002811
Leng, A., Xu, C., Nicholas, S., Nicholas, J., & Wang, J. (2019). Quality of life in caregivers of a family member with serious mental illness: Evidence from China. Archives of Psychiatric Nursing, 33(1), 23–29. https://doi.org/10.1016/j.apnu.2018.08.010
Leonhardt, B. L., Huling, K., Hamm, J. A., Roe, D., Hasson-Ohayon, I., McLeod, H. J., & Lysaker, P. H. (2017). Recovery and serious mental illness: A review of current clinical and research paradigms and future directions. Expert Review of Neurotherapeutics, 17(11), 1117–1130. https://doi.org/10.1080/14737175.2017.1378099
Li, J., Lambert, C. E., & Lambert, V. A. (2007). Predictors of family caregivers’ burden and quality of life when providing care for a family member with schizophrenia in the People’s Republic of China. Nursing and Health Sciences, 9(3), 192–198. https://doi.org/10.1111/j.1442-2018.2007.00327.x
Lua, P. L., & Bakar, Z. A. (2011). Health-related quality of life profiles among family caregivers of patients with schizophrenia. Family and Community Health, 34(4), 331–339. https://doi.org/10.1097/FCH.0b013e31822b54ad
Maragakis, A., & Vriesman, M. (2018). Serious mental illness. Principle-Based Stepped Care and Brief Psychotherapy for Integrated Care Settings, 369–378. https://doi.org/10.1007/978-3-319-70539-2_33
Margetić, B. A., Jakovljević, M., Furjan, Z., Margetić, B., & Marsanić, V. B. (2013). Quality of life of key caregivers of schizophrenia patients and association with kinship. Central European Journal of Public Health, 21(4), 220–223. https://doi.org/10.21101/cejph.a3918
Martín-Pérez, C., Herrero-Martin, J. J., Pérez-López, G., Pedrosa-García, R., Ibañez-Casas, I., Torres-González, F., & Moreno-Küstner, B. (2019). Severe mental illness in community mental health care in Spain: Prevalence and related factors. Journal of Nervous and Mental Disease, 207(2), 106–111. https://doi.org/10.1097/NMD.0000000000000929
Maruish, M. E. (Ed.). (2004). Symptom Assessment-45 questionnaire (SA-45). In The use of psychological testing for treatment planning and outcomes assessment. Lawrence Erlbaum Associates. https://doi.org/10.4324/9781410610638
Md Sakip, S. R., Mohd Zukri, A. Z., & Megat Abdul Rahim, P. R. (2023). Assessing the relationship between environmental, psychological, physical and social towards the quality of life. International Journal of Sustainable Construction Engineering and Technology, 14(2), 256–265. https://doi.org/10.30880/ijscet.2023.14.02.027
Menzies, R. G., & Menzies, R. E. (2020). Emotional pain and suffering: The search for global solutions. Beyond the psychology industry: How else might we heal? (pp. 11–22). https://doi.org/10.1007/978-3-030-33762-9_2
Ministry of Health of the government of Andalusia. (2020). Integrated care process in serious mental disorder. Autonomous Government of Andalusia. Ministry of Health and Families
Mosqueiro, B. P., da Rocha, N. S., & Fleck, M. P. (2015). Intrinsic religiosity, resilience, quality of life, and suicide risk in depressed inpatients. Journal of Affective Disorders, 179, 128–133. https://doi.org/10.1016/j.jad.2015.03.022
Noghani, F. (2016). Health related quality of life in family caregivers of patients suffering from mental disorders. Journal of Clinical and Diagnostic Research, 10(11), VC05–VC09. https://doi.org/10.7860/JCDR/2016/19671.8792
Orrico-Sánchez, A., López-Lacort, M., Muñoz-Quiles, C., Sanfélix-Gimeno, G., & Díez-Domingo, J. (2020). Epidemiology of schizophrenia and its management over 8-years period using real-world data in Spain. BMC Psychiatry, 20(1), 149. https://doi.org/10.1186/s12888-020-02538-8
Pinto, S., Fumincelli, L., Mazzo, A., Caldeira, S., & Martins, J. C. (2017). Comfort, well-being and quality of life: Discussion of the differences and similarities among the concepts. Porto Biomedical Journal, 2(1), 6–12. https://doi.org/10.1016/j.pbj.2016.11.003
Ribé Buitrón, J. M., Pérez Téstor, C., Muros Guijarro, R., & Nofuentes García, C. (2018). Considerations about the interpretation of the Zarit scale in caregivers of patients with schizophrenia. Atención Primaria, 50(7), 443–444. https://doi.org/10.1016/j.aprim.2017.10.009
Saavedra, J., Brzeska, J., Matías-García, J. A., & Arias-Sánchez, S. (2023). Quality of life and psychiatric distress in people with serious mental illness, the role of personal recovery. Psychology and Psychotherapy, 96(2), 525–541. https://doi.org/10.1111/papt.12451
Sharp, M. K., Bertizzolo, L., Rius, R., Wager, E., Gómez, G., & Hren, D. (2019). Using the STROBE statement: Survey findings emphasized the role of journals in enforcing reporting guidelines. Journal of Clinical Epidemiology, 116, 26–35. https://doi.org/10.1016/j.jclinepi.2019.07.019
Son, C. H. (2020). The effects of retirement on health-related quality of life of retirement-aged adults for four marital status subgroups. International Journal of Economic Sciences, IX(1), 179–201. https://doi.org/10.20472/ES.2020.9.1.010
Stoyanova, A., & Pinilla, J. (2019). Socioeconomic burden of mental disorders in Spain 2006–2017. SSRN Electronic Journal. https://doi.org/10.2139/ssrn.3369466
Tang, I. C., & Wu, H. C. (2012). Quality of life and self-stigma in individuals with schizophrenia. The Psychiatric Quarterly, 83(4), 497–507. https://doi.org/10.1007/s11126-012-9218-2
Tang, B., Yu, Y., Liu, Z., Lin, M., Chen, Y., Zhao, M., & Xiao, S. (2017). Factor analyses of the Chinese Zarit Burden Interview among caregivers of patients with schizophrenia in a rural Chinese community. British Medical Journal Open, 7(9), e015621. https://doi.org/10.1136/bmjopen-2016-015621
Vera-Villarroel, P., Silva, J., Celis-Atenas, K., & Pavez, P. (2014). Evaluación del cuestionario SF-12: Verificación de la utilidad de la escala salud mental. Revista Médica De Chile, 142(10), 1275–1283. https://doi.org/10.4067/S0034-98872014001000007
ZamZam, R., Midin, M., Hooi, L. S., Yi, E. J., Ahmad, S. N., Azman, S. F., Borhanudin, M. S., & Radzi, R. S. (2011). Schizophrenia in Malaysian families: A study on factors associated with quality of life of primary family caregivers. International Journal of Mental Health Systems, 5(1), 16. https://doi.org/10.1186/1752-4458-5-16
Zauszniewski, J. A., Bekhet, A. K., & Suresky, M. J. (2009). Relationships among perceived burden, depressive cognitions, resourcefulness, and quality of life in female relatives of seriously mentally ill adults. Issues in Mental Health Nursing, 30(3), 142–150. https://doi.org/10.1080/01612840802557204
Zhang, B., Conner, K. O., Meng, H., Tu, N., Liu, D., & Chen, Y. (2021). Social support and quality of life among rural family caregivers of persons with severe mental illness in Sichuan Province, China: Mediating roles of care burden and loneliness. Quality of Life Research, 30(7), 1881–1890. https://doi.org/10.1007/s11136-021-02793-6
Acknowledgements
We are grateful to the team of translators at Enago for their valuable contributions, including their expertise in the English language and their insightful suggestions, which played a crucial role in the success of this paper.
Funding
Funding for open access publishing: Universidad de Sevilla/CBUA The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by De Medina-Moragas AJ and Lima-Serrano M. The first draft of the manuscript was written by De Medina-Moragas AJ and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical statement
All participants provided informed consent for inclusion before participating in the study after being appropriately informed. Ethical integrity was ensured by employing a multidisciplinary team, including mental health professionals, to rigorously and objectively evaluate the consent capacity of participants with SMI who were deemed unable to provide consent. Legal representatives were provided with regular training sessions to align their decisions with the participants’ interests, and communication barriers were addressed through iterative feedback processes. Simplified or adapted consent forms were used to facilitate participants’ understanding, and the study design allowed for the ongoing reassessment of consent and participant well-being. This comprehensive approach accommodated the complex needs of the SMI population while maintaining ethical standards. Appropriate steps were taken to ensure the provision of accurate information to participants through data confidentiality, archiving, and safekeeping of documents. This study was conducted in accordance with the ethical principles outlined in the 1964 Declaration of Helsinki and its later addenda. All procedures involving human participants were approved by the Biomedical Ethics Committee of Andalusia.
Conflict of interest
Nothing to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Medina-Moragas, A.J., Lima-Serrano, M., Fernández-Fernández, M.J. et al. Quality of life of individuals with serious mental illness and family caregivers. Curr Psychol 43, 21756–21767 (2024). https://doi.org/10.1007/s12144-024-05961-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-024-05961-2