Abstract
Previous studies have documented the average impact of the COVID-19 pandemic on depressive symptoms among the older population. However, discerning specific individuals at a higher risk and developing targeted support based on the significant average effect has proven challenging. In response to this gap, this study explored the influence of personal histories, encompassing pre-existing depression and personal depression trajectories, as well as personal experiences such as pandemic-related financial and health impacts, on deviations in individual depression curves during the pandemic. The results of the study indicated that individuals with pre-existing depressive symptoms or those affected by pandemic-related financial and health challenges experienced an upward deviation from their original depression trajectory, signifying a more severe level of depression during the pandemic. Interestingly, individuals who demonstrated a steeper growth in depression prior to the pandemic exhibited less severe depressive symptoms during this period, showcasing a downward deviation in their personal depression trajectory. These findings contribute valuable insights into the diverse personal factors driving depression during the pandemic. They also provide guidance on prioritizing the allocation of social support resources to effectively manage depression among the older population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The COVID-19 pandemic has significantly impacted people's mental health, causing disruptions in various aspects of their lives. Economic shutdowns and social distancing measures have negatively affected labor force participation, social connections, engagement, and recreational activities, leading to a higher prevalence of depressive symptoms in the general population (Necho et al., 2021; Zhang et al., 2022). Among different age groups, older adults tend to experience a more chronic course of depressive symptoms (Gondek et al., 2022; Kwong et al., 2019). Importantly, depression in old age is associated with a higher risk of physical disability, psychiatric comorbidity, and mortality (Ho et al., 2014; Krishnamoorthy et al., 2020). Consequently, researchers have shown particular interest in examining the relationship between the COVID-19 pandemic and depressive symptoms (Ciuffreda et al., 2021; Lebrasseur et al., 2021; Mistry et al., 2021; Morrow-Howell et al., 2020).
However, prior studies have not adequately concentrated on older adults, particularly those who have been grappling with depression long before the pandemic (Yan et al., 2022). Specifically, existing research insufficiently explores how pre-existing depression and distinct personal depression trajectories before the pandemic influence depressive symptoms during this period. Establishing this knowledge holds valuable implications, including the development of more targeted interventions catering to the unique needs of older individuals who have been experiencing depression prior to the pandemic. Additionally, it contributes to fostering a nuanced understanding of the severity of depression during the pandemic by adopting the perspective of "depression history." This knowledge is crucial for mental health professionals in devising effective long-term support strategies.
Furthermore, we observed that previous research often treats the impact of the pandemic as a broad environmental construct, neglecting to examine how specific pandemic characteristics, such as financial and health impacts, influence changes in depression during this period. Addressing this limitation is crucial, as it can guide the allocation of limited resources to more effectively manage depressive symptoms among older individuals with "different negative experiences" during the pandemic. Motivated by these considerations, this study aimed to investigate the impact of pre-existing depression on changes in depression during the pandemic, explore how variations in personal depression trajectories affect changes in depression during this period, and examine how pandemic characteristics, including financial and health impacts, influence changes in depression during the pandemic. To achieve these objectives, we utilized a panel dataset consisting of three-wave observations before the pandemic and a follow-up test conducted during the pandemic among older adults in Hong Kong. The findings have the potential to comprehensively illustrate how personal history before the pandemic and personal experiences during the pandemic affect depressive symptomatology during this challenging period.
Literature review
The COVID-19 pandemic as a special disaster
Disasters are acute events that negatively affect the living environment, physical health, employment opportunities, and financial status of individuals, subsequently becoming stressors that increase the likelihood of depression (Lock et al., 2012). Disasters can be either natural, such as tornados or tsunamis, or human-made, such as terrorist attacks (Wilson-Genderson et al., 2018). Unlike disasters that are geographically confined and affect specific population groups, the COVID-19 pandemic has impacted social and economic activities across almost all segments of the population (National Center for Health Statistics and Centers for Disease Control and Prevention, 2020; Peleg et al., 2021). Scholars found high prevalence of anxiety symptoms (6.33% to 50.9%), depression (14.6% to 48.3%), post-traumatic stress disorder (7% to 53.8%), psychological distress (34.43% to 38%), and stress (8.1% to 81.9%) in the general population across various countries during the COVID-19 pandemic (Xiong et al., 2020). However, older adults are particularly vulnerable to mental health disorders during this period due to limited access to resources, such as financial and instrumental support, from families and society, exacerbating the occurrence of mental health issues (Gilligan et al., 2020; Li et al., 2021).
Existing literature has made significant progress in understanding the link between disasters and depressive symptoms. Disasters inevitably result in financial impacts, such as property damage and unemployment, as well as health-related consequences like injuries during such events (Schwartz et al., 2016; Tsuboya et al., 2016). Pre-existing depression can evoke feelings of fear, which are likely to contribute to more severe depressive symptoms in the context of disasters (Kar, 2019; Tang et al., 2014). Furthermore, for individuals with prolonged depressive symptoms and established personal depression trajectories before the pandemic, the disaster itself may inevitably reshape these trajectories in the long term (Mandavia & Bonanno, 2019; van der Velden et al., 2013). Given that the COVID-19 pandemic is a unique disaster in human history, affecting almost all economies and societies, there is a strong motivation to comprehensively study these issues in the context of the pandemic.
COVID-19 pandemic and depression among older adults
According to the research landscape mentioned above, our understanding of the impact of the pandemic on depression among older adults remains incomplete, primarily due to the sole reliance on cross-sectional samples, inadequate baseline assessments, limited exploration of within-person changes and individual differences, and inconsistent findings (Bendau et al., 2021; Hamm et al., 2020). Based on cross-sectional data collected from a sample of older adults in the United States during the pandemic, Hamm et al. (2020) found that most older adults with pre-existing depressive symptoms did not report more severe depression during the pandemic and demonstrated resilience.
However, studies that tracked depression status among older adults during the pandemic (Bendau et al., 2021) or compared data collected before and after the pandemic in European countries (Paccagnella & Pongiglione, 2022) revealed that pre-existing depression increased the risk of depression worsening during the pandemic. A more advanced design by den Besselaar et al. (2021) tracked the depression of a sample of Dutch older adults across four waves before the pandemic and included a follow-up assessment during the pandemic. They found that the depression of older adults did not deteriorate during the pandemic, suggesting resilience. However, den Besselaar et al. (2021) did not further investigate certain issues:
-
Estimating personal depression trajectories among older adults before the pandemic.
-
Investigating how pre-existing depression affects changes in depression during the pandemic.
-
Examining how differences in personal depression trajectories affect changes in depression during the pandemic.
-
Investigating how pandemic characteristics, such as financial and health impacts, influence changes in depression during the pandemic.
These issues are crucial components of the research landscape concerning the effects of disasters on depression. In response, this study fills these gaps by conducting a follow-up assessment of a sample of older adults in Hong Kong, tracking them across three waves before the outbreak of the COVID-19 pandemic. We adopted a data structure similar to that of den Besselaar et al. (2021) but employed advanced data analytics to generate findings that contribute to the research landscape on the effects of COVID-19 on depression among older adults.
Pre-existing depression and depression during the pandemic
The COVID-19 pandemic may increase the vulnerability of older adults with pre-existing mental health disorders to the development of depressive symptoms (United Nations, 2020). Factors such as pre-existing social isolation and fear of infection can contribute to more severe depression during the pandemic. Qualitative interviews conducted with older adults in the US revealed that those with pre-existing depression initially displayed resilience to social isolation due to their prior experience in coping with depression (Hamm et al., 2020). However, prolonged social distancing measures may gradually erode this resilience, ultimately leading to an increase in depression among individuals with pre-existing depressive symptoms (Hamm et al., 2020).
A systematic review by Neelam et al. (2021) identified a limited number of quantitative analyses examining the relationship between pre-existing mental illness and mental health during the pandemic. The findings echoed the "honeymoon effect," indicating that individuals with pre-existing mental disorders experienced a deterioration in their mental health during the pandemic. However, most of the previous research relied on cross-sectional samples, and only a few studies compared mental health before and during the pandemic (Berthelot et al., 2020; Lara et al., 2020). To validate these findings, there is a need for follow-up assessments during the pandemic of older adults who were well-tracked before the outbreak.
Individual depression trajectory and depression during the pandemic
Previous studies have consistently revealed diverse trajectories of depression among older adults at the individual level (Holmes et al., 2018; Musliner et al., 2016). Factors such as age, sex, education, income, and health-related factors contribute to the longitudinal changing trends in depressive symptoms (Andreescu et al., 2008; de la Torre-Luque et al., 2019). Musliner et al.'s (2016) systematic review identified different trajectory types characterized by the intensity and stability of depression. The persistently rising depression trajectory has garnered attention due to its association with more severe depressive symptoms, sensory difficulties, worsened physical functioning, higher risk of dementia, and increased mortality in old age (Fritze et al., 2016; Kaup et al., 2016; Liang et al., 2011).
Considering the negative effects of the rising depression trajectory, it is important to investigate how the pandemic shapes depression among older adults who experienced an increase in depression before the outbreak. This area remains underexplored in the literature. Therefore, this study examined how the estimated depression slope based on three-wave pre-pandemic data predicted depressive symptoms during the pandemic among older adults in Hong Kong.
Pandemic-related characteristics and depression during the pandemic
When considering the deviation of depression during the pandemic from pre-pandemic trajectories, the role of pandemic-related impacts becomes crucial (De France et al., 2022). Financial and health impacts are two significant factors related to the pandemic, with financial impacts stemming from the economic shutdown and health impacts arising from fear or actual declines in physical health due to the infection. Recent research has shown that poor financial status, particularly expenditure-based poverty and material deprivation, is associated with higher levels of depression among older adults before the pandemic (Zhu & Chou, 2022b).
An interesting issue arises regarding older adults who were not initially expenditure-poor or materially deprived before the pandemic but fell into expenditure-based poverty or experienced material deprivation during the pandemic. It remains unclear whether these individuals deviate more from their personal depression trajectory and report higher levels of depressive symptoms during the pandemic. Similarly, the impact of perceived worsening physical health during the pandemic on depression trajectory deviation remains underexplored. Addressing these issues can provide valuable insights into the pandemic's specific impact and offer actionable strategies for policymakers to address depression among older adults. Therefore, this study examined how changes in poverty and health status before and during the pandemic predicted depressive symptoms among older adults in Hong Kong.
Research hypotheses
Based on our previous tracking of depression and other characteristics of older adults in Hong Kong (i.e., the three-wave data collected before the pandemic), we collected an additional wave during the pandemic to comprehensively examine the effects of the pandemic on depression in this population (Zhu & Chou, 2022a, b). We hypothesized that older adults would report an upward deviation in depression during the pandemic compared to the estimated trajectory based on pre-pandemic observations (Hypothesis 1). Furthermore, individuals with more severe pre-existing depression or a steeper depression trajectory were expected to exhibit a greater upward deviation from their individual depression trajectory during the pandemic (Hypotheses 2 and 3). Lastly, we hypothesized that older adults who experienced a transition into poverty or perceived worsened physical health during the pandemic would report higher levels of depressive symptoms that deviated from their individual trajectory (Hypotheses 4 and 5).
Methods
Sample
In 2015, we identified the target participants based on a complete sampling framework in Hong Kong that could connect the sample identified to the population. The Census and Statistics Department of Hong Kong codes all living units in Hong Kong based on their register of quarters and the register of segments. We used stratified sampling to obtain a small but representative sample of households (N = 3,000). We invited one older adult in each household to be interviewed with a structural questionnaire in person by our well-trained interviewer. Excluding empty households and households without older adults aged 60 or above, 2,817 households accepted our invitation to join the data collection. When there was more than one older resident in a household, we invited the one whose birthday was closest to the interview date to join the interview. In 2017, our team tracked the same sample but successfully interviewed only 1,696 older adults (attrition rate 39.8%). In 2019, we continued to track these 1,696 participants but successfully collected data from only 838 of them (attrition rate 50.6%). Considering that the third-wave data were collected between May and October 2019 and that the first infectious case of COVID-19 occurred in Wuhan, China, in December 2019, the three-wave dataset (N = 838) could be used as longitudinal observations before the outbreak of the coronavirus pandemic.
To measure the depressive symptoms of older adults during the pandemic, we collected the fourth wave of data on the pandemic. More specifically, we conducted the fieldwork between May and July 2021. We successfully approached 275 older adults who joined the interviews in the third wave of data collection in 2019 (attrition rate 67.9%). The participants successfully interviewed in all four waves (N = 275) constituted the sample used to examine the five hypotheses, as mentioned earlier.
Measures
We assessed the pandemic’s financial impacts as the change in poverty between the third and fourth waves. We assessed poverty using four indicators: income-based, expenditure-based, and asset-based poverty, as well as material deprivation. The outcome variable, depression, was measured in all four waves. We assessed the pandemic’s health impacts as the change in health status between the third and fourth waves. All measurement constructs, their respective observed items, and coding details are reported in Table 1.
Data analysis
Following the design of a very recent longitudinal study that examined the mental health changes during the pandemic (De France et al., 2022), the current study adopted the linear latent growth model to examine five hypotheses proposed earlier that elaborate the impacts of the pandemic on depression among older adults (see Fig. 1). The difference in the path coefficients of slopes across the four waves was fixed as equal, considering there was no difference in space between each pair of consecutive data collection time points (Hancock et al., 2013). As the intercept should reflect the baseline score of depression, the path coefficients of the intercepts were fixed as equal across four waves (see Fig. 1). The next step in specifying the model structure was to link both slope and intercept to the residual depression at wave 4 (see Fig. 1). The significance of the residual intercept in wave 4 reflected whether the depression during the pandemic was significantly different than that before the pandemic at the average level.
The estimated coefficient of the path from the latent intercept that was to the residual depression in wave 4 suggested how the depression of older adults with pre-existing depression deviated from their trajectory during the pandemic. The estimated coefficient of the path from the latent slope to the residual depression in wave 4 reflected how the depressive symptoms of those with steeper growth of depression deviated from their trajectories (Burant, 2016). Lastly, we added four financial and health impacts to the model separately, suggesting that five models should be examined in total. Overall, the critical parameters to be estimated in the model were the intercept of the residual depression in wave 4, the path coefficients of the “latent” intercept and slope, and the path coefficients of the four financial impact predictors and health impact predictors.
Results
We performed the formal attrition analysis and reported the results in Table 2. Although the attrition rate was not low, there was almost no significant structural difference between the dropouts and survivors in 2021, based on the measurement outcomes at the baseline in 2015. Income-based and asset-based poverty (measured in 2015) was slightly higher among survivors in 2021 compared to those among dropouts between 2015 and 2019 (Income-based poverty: 32.4% vs. 25.5%; Asset-based poverty: 37.5% vs. 30.9%). There was no significant difference in gender, age, or other focal variables (expenditure-based poverty, material deprivation, depression, and self-rated health) between survivors in 2021 and dropouts between 2015 and 2019.
The results of the latent linear growth models are reported in Table 3. In all five models, the estimated variances of both latent intercept and slope were positive and significant (variance [intercept] = 17.183 − 17.290, p < 0.001; variance [slope] = 19.611 − 19.803, p < 0.001). This suggests that there were sufficient differences in the baseline depression and personal depression trajectory among the participants. The intercept of the residual depression score at wave 4 (during the pandemic) was insignificant (b = 0.013 − 0.079, p > 0.05) in all five models. This indicates that the level of depression during the pandemic (i.e., wave 4) did not show a significant difference compared to the period before the pandemic at the average level.
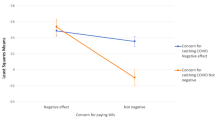
The significant and positive coefficients of the paths from the latent intercept to the residual depression in wave 4 suggested that those with a higher level of depression at the baseline had a higher residual of depression at wave 4 (b = 0.055 − 0.057, p < 0.001). This meant that the depression score of those with more serious pre-existing depression deviated more upward from the individual depression trajectory during the pandemic. The significant and negative coefficients of the paths from the latent slope to the residual depression in wave 4 revealed that older adults with a steeper growth of depression reported lower residual depression at wave 4 (b = -0.211 − -0.209, p < 0.001). In other words, the depression score of older adults holding a steeper growth of depression before the pandemic deviated downward from the individual depression trajectory during the pandemic.
Older participants exposed to four financial impacts had higher residuals of depression. Specifically, the impact of falling into expenditure-based poverty on promoting residual depression at wave 4 was the highest (b = 0.243, p < 0.001), followed by material deprivation (b = 0.064, p < 0.001), asset-based poverty (b = 0.045, p < 0.001), and income-based poverty (b = 0.014, p < 0.001). Falling into expenditure-poor at wave 4 most powerfully changed the personal depression trajectory. Moreover, older adults who suffered health-related problems reported a higher residual depression at wave 4, suggesting that the depression during the pandemic deviated upward from the individual trajectory (b = 0.094, p < 0.001).
Discussion
The COVID-19 pandemic has had a significant impact on the mental health of older adults, and this study comprehensively examined the deviation of depression from its original trajectory during the pandemic. We did not find the average effect, but found that the pandemic's effect on depression among older adults is conditional, depending on their pre-existing depression, personal depression trajectories, and exposure to financial or health risks.
Contrary to Hypothesis 1, which suggested that the pandemic would modify the development path of depression among older adults at the individual level, we found that the pandemic alone did not significantly alter the overall trajectory of depression at the average level. This finding emphasizes the importance of considering individual characteristics (e.g., personal history before the pandemic and personal experience during the pandemic) and pandemic-related factors (e.g., financial and health impacts) in understanding the relationship between the pandemic and depression.
Our findings supported Hypothesis 2, indicating that older adults with pre-existing depression experienced worsened depressive symptoms during the pandemic. Despite their prior experience in managing depression, the prolonged economic shutdown and social distancing measures likely depleted their resilience and patience. This highlights the need for targeted interventions and support for older adults with pre-existing depression during crises like the COVID-19 pandemic.
Surprisingly, we found evidence contradicting Hypothesis 3. Older adults with steeper growth in depression before the pandemic were less susceptible to the pandemic's impact on their depression trajectory. This could be attributed to a ceiling effect, where personal stressors leading to a steep growth in depression in old age may have already driven their depression to a high level before the pandemic began. As a result, they may have become less sensitive to adverse events occurring during the pandemic. This finding underscores the importance of considering an individual's depression history rather than a single baseline measurement when assessing their risk of experiencing severe depression during crises.
Regarding the pandemic-related factors, we examined the impact of poverty and perceived worsened physical health. We found that all indicators of poverty, including income-based, asset-based, material-based, and expenditure-based poverty, were associated with a upward deviation in the depression trajectory during the pandemic. Notably, expenditure-based poverty had the strongest influence on promoting depressive symptoms during the pandemic among older adults. This suggests that the economic stressors arising from the pandemic, such as increased costs of essential goods and limited consumption options, can significantly impact the mental health of older adults, especially those who fall into expenditure-based poverty during this period.
Similarly, perceived worsened physical health during the pandemic was associated with a upward deviation in the depression trajectory, although to a lesser extent than expenditure-based poverty. This finding highlights the importance of addressing the quality of life and physical well-being of older adults during crises to prevent the exacerbation of depressive symptoms (Amuda et al., 2022; Oluwatayo et al., 2022). Our results contribute to the theoretical debates on how the personal depression trajectory changes during a pandemic when individuals are exposed to the pandemic in different ways. They also shed light on the significance of economic stressors and the need for social services to consider the history of depressive symptoms when identifying vulnerable older adults.
Limitations
Despite the valuable insights provided by this study, several limitations should be acknowledged. First, the inclusion of only one wave of measurement during the pandemic limits our understanding of the development pattern of depression during this period. Multiple waves of follow-up assessments during the pandemic would have allowed for a more comprehensive analysis of how the depression status of older adults changed in the long run after exposure to the pandemic. Chudzicka-Czupała et al. (2022) monitored the mental health of a sizable sample in Poland during the pandemic, examining conditions such as depression, stress, and anxiety. They did not observe a "continuously increasing" or "continuously decreasing" trend in mental health disorder symptoms throughout the pandemic. This underscores the necessity to delve deeper into the changes in depressive symptoms during the pandemic by considering individual trajectories (Chudzicka-Czupała et al., 2022). Their findings strongly motivated us to gather additional data in the form of the fifth and sixth waves, during or after the pandemic, and this data collection is currently underway.
Non-random attrition is another limitation of this study. The sample had a tendency to consist of economically disadvantaged older adults, suggesting that the reported depressive symptoms in the sample may be more severe than those in the general older population. This likely "ceiling effect" may explain why the model could not detect a significant intercept of residual depression (i.e., no average effect). Replicating this design with a large-scale sample and low attrition rates would provide further insights into the relationship between the pandemic and depression among older adults.
Furthermore, the high dropout rate in this study may have been influenced by the long time interval between assessments (i.e., two years). Future follow-up tests should consider shortening the time interval (e.g., six months) to minimize attrition. Statistical adjustments, such as constrained factor loading on the slope, can be applied to reflect the different time intervals when estimating the model.
Conclusion
After finding the significant average effects of exposure to the pandemic on the increased prevalence of mental disorders among the older population, scholars were naturally drawn to considering the pandemic as the starting point and studying mental disorders as outcomes of a shared negative psychological transformation activated by pandemic-related factors (e.g., social isolation). This approach indeed contributes to understanding social psychology in the context of the pandemic. However, it overlooks the fact that the observed average increase in depression can be partially attributed to personal depression histories (e.g., pre-existing depression, personal depression trajectories) and individual pandemic-related experiences (e.g., worsened health, falling into poverty). Directly exploring these personalized drivers is crucial, as it provides guidance on where limited social resources should be invested, especially if the priority policy goal is to minimize the negative impacts of the pandemic.
Our findings clearly indicate that, among those with serious pre-existing depression and those experiencing a steep increase in depression before the pandemic, more social support should be directed to the former. Similarly, between those suffering from worsened self-rated health and those falling into expenditure-based poverty, more social support should be directed to the latter. We encourage scholars in other economies to replicate our design using their longitudinal data (if available). We believe that different narratives may emerge, and the findings can be linked to the specific healthcare and welfare systems in each economy.
Data availability
Data and materials are available on request from the authors.
References
Amuda, Y. J., Chikhaoui, E., Hassan, S., & Dhali, M. (2022). Qualitative exploration of legal, economic and health impacts of Covid-19 in Saudi Arabia. Emerging Science Journal, 6, 1–14.
Andreescu, C., Chang, C. C. H., Mulsant, B. H., & Ganguli, M. (2008). Twelve-year depressive symptom trajectories and their predictors in a community sample of older adults. International Psychogeriatrics, 20(2), 221–236.
Bendau, A., Kunas, S. L., Wyka, S., Petzold, M. B., Plag, J., Asselmann, E., & Ströhle, A. (2021). Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: The role of pre-existing anxiety, depressive, and other mental disorders. Journal of Anxiety Disorders, 79, 102377.
Berthelot, N., Lemieux, R., Garon-Bissonnette, J., Drouin-Maziade, C., Martel, É., & Maziade, M. (2020). Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstetricia et Gynecologica Scandinavica, 99(7), 848–855.
Burant, C. J. (2016). Latent growth curve models: Tracking changes over time. The International Journal of Aging and Human Development, 82(4), 336–350.
Cheung, K. C. K., & Chou, K. L. (2019). Poverty, deprivation and life satisfaction among Hong Kong older persons. Ageing & Society, 39(4), 703–721.
Chudzicka-Czupała, A., Chiang, S. K., Grabowski, D., Żywiołek-Szeja, M., Quek, M., Pudełek, B., ..., & McIntyre, R. S. (2022). Predictors of psychological distress across three time periods during the COVID-19 pandemic in Poland. International Journal of Environmental Research and Public Health, 19(22), 15405.
Ciuffreda, G., Cabanillas-Barea, S., Carrasco-Uribarren, A., Albarova-Corral, M. I., Argüello-Espinosa, M. I., & Marcén-Román, Y. (2021). Factors associated with depression and anxiety in adults≥ 60 years old during the COVID-19 pandemic: A systematic review. International Journal of Environmental Research and Public Health, 18(22), 11859.
De France, K., Hancock, G. R., Stack, D. M., Serbin, L. A., & Hollenstein, T. (2022). The mental health implications of COVID-19 for adolescents: Follow-up of a four-wave longitudinal study during the pandemic. American Psychologist, 77(1), 85–99.
de la Torre-Luque, A., de la Fuente, J., Prina, M., Sanchez-Niubo, A., Haro, J. M., & Ayuso-Mateos, J. L. (2019). Long-term trajectories of depressive symptoms in old age: Relationships with sociodemographic and health-related factors. Journal of Affective Disorders, 246, 329–337.
Fritze, T., Teipel, S., Óvári, A., Kilimann, I., Witt, G., & Doblhammer, G. (2016). Hearing impairment affects dementia incidence. An analysis based on longitudinal health claims data in Germany. PLoS One, 11(7), e0156876.
Gilligan, M., Suitor, J. J., Rurka, M., & Silverstein, M. (2020). Multigenerational social support in the face of the COVID-19 pandemic. Journal of Family Theory & Review, 12(4), 431–447.
Gondek, D., Bann, D., Patalay, P., Goodman, A., McElroy, E., Richards, M., & Ploubidis, G. B. (2022). Psychological distress from early adulthood to early old age: Evidence from the 1946, 1958 and 1970 British birth cohorts. Psychological Medicine, 52(8), 1471–1480.
Hamm, M. E., Brown, P. J., Karp, J. F., Lenard, E., Cameron, F., Dawdani, A., ..., & Lenze, E. J. (2020). Experiences of American older adults with pre-existing depression during the beginnings of the COVID-19 pandemic: A multicity, mixed-methods study. The American Journal of Geriatric Psychiatry, 28(9), 924−932.
Hancock, G. R., Harring, J. R., & Lawrence, F. R. (2013). Using latent growth modeling to evaluate longitudinal change. In G. R. Hancock & R. O. Mueller (Eds.), Quantitative methods in education and the behavioral sciences: Issues, research, and teaching (pp. 309–341). IAP Information Age Publishing.
Ho, R. C., Ho, E. C., Tai, B. C., Ng, W. Y., & Chia, B. H. (2014). Elderly suicide with and without a history of suicidal behavior: Implications for suicide prevention and management. Archives of Suicide Research, 18(4), 363–375.
Holmes, S. E., Esterlis, I., Mazure, C. M., Lim, Y. Y., Ames, D., Rainey‐Smith, S., ..., & Australian Imaging, Biomarkers and Lifestyle Research Group. (2018). Trajectories of depressive and anxiety symptoms in older adults: A 6‐year prospective cohort study. International Journal of Geriatric Psychiatry, 33(2), 405−413.
Kar, N. (2019). Depression in youth exposed to disasters, terrorism and political violence. Current Psychiatry Reports, 21(8), 1–11.
Kaup, A. R., Byers, A. L., Falvey, C., Simonsick, E. M., Satterfield, S., Ayonayon, H. N., ..., & Yaffe, K. (2016). Trajectories of depressive symptoms in older adults and risk of dementia. JAMA Psychiatry, 73(5), 525−531.
Krishnamoorthy, Y., Rajaa, S., & Rehman, T. (2020). Diagnostic accuracy of various forms of geriatric depression scale for screening of depression among older adults: Systematic review and meta-analysis. Archives of Gerontology and Geriatrics, 87, 104002.
Kwong, A. S., Manley, D., Timpson, N. J., Pearson, R. M., Heron, J., Sallis, H., ..., & Leckie, G. (2019). Identifying critical points of trajectories of depressive symptoms from childhood to young adulthood. Journal of Youth and Adolescence, 48(4), 815−827.
Lara, B., Carnes, A., Dakterzada, F., Benitez, I., & Piñol-Ripoll, G. (2020). Neuropsychiatric symptoms and quality of life in Spanish patients with Alzheimer’s disease during the COVID-19 lockdown. European Journal of Neurology, 27(9), 1744–1747.
Lebrasseur, A., Fortin-Bédard, N., Lettre, J., Raymond, E., Bussières, E. L., Lapierre, N., ..., & Routhier, F. (2021). Impact of the COVID-19 pandemic on older adults: Rapid review. JMIR Aging, 4(2), e26474.
Li, F., Luo, S., Mu, W., Li, Y., Ye, L., Zheng, X., ..., & Chen, X. (2021). Effects of sources o social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry, 21(1), 1−14.
Liang, J., Xu, X., Quiñones, A. R., Bennett, J. M., & Ye, W. (2011). Multiple trajectories of depressive symptoms in middle and late life: Racial/ethnic variations. Psychology and Aging, 26(4), 761–777.
Lock, S., Rubin, G. J., Murray, V., Rogers, M. B., Amlôt, R., & Williams, R. (2012). Secondary stressors and extreme events and disasters: A systematic review of primary research from 2010−2011. PLoS Currents, 4, 3492002.
Mandavia, A. D., & Bonanno, G. A. (2019). When natural disaster follows economic downturn: The incremental impact of multiple stressor events on trajectories of depression and posttraumatic stress disorder. Disaster Medicine and Public Health Preparedness, 13(2), 173–182.
Mistry, S. K., Ali, A. R. M., Hossain, M., Yadav, U. N., Ghimire, S., Rahman, M., ..., & Huque, R. (2021). Exploring depressive symptoms and its associates among Bangladeshi older adults amid COVID-19 pandemic: Findings from a cross-sectional study. Social Psychiatry and Psychiatric Epidemiology, 56(8), 1487−1497.
Morrow-Howell, N., Galucia, N., & Swinford, E. (2020). Recovering from the COVID-19 pandemic: A focus on older adults. Journal of Aging & Social Policy, 32(4–5), 526–535.
Musliner, K. L., Munk-Olsen, T., Eaton, W. W., & Zandi, P. P. (2016). Heterogeneity in long-term trajectories of depressive symptoms: Patterns, predictors and outcomes. Journal of Affective Disorders, 192, 199–211.
National Center for Health Statistics & Centers for Disease Control and Prevention. (2020). Provisional COVID-19 death counts by sex, age, and state. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku. Accessed 15 Mar 2023
Necho, M., Tsehay, M., Birkie, M., Biset, G., & Tadesse, E. (2021). Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. International Journal of Social Psychiatry, 67(7), 892–906.
Neelam, K., Duddu, V., Anyim, N., Neelam, J., & Lewis, S. (2021). Pandemics and pre-existing mental illness: A systematic review and meta-analysis. Brain, Behavior, & Immunity-Health, 10, 100177.
Oluwatayo, I. B., Ojo, A. O., & Adediran, O. A. (2022). Socioeconomic impacts of Households’ Vulnerability during COVID-19 Pandemic in South Africa: Application of Tobit and Probit Models. HighTech and Innovation Journal, 3(4), 385–393.
Paccagnella, O., & Pongiglione, B. (2022). Depression deterioration of older adults during the first wave of the COVID-19 outbreak in Europe. Social Science & Medicine, 299, 114828.
Peleg, K., Bodas, M., Hertelendy, A. J., & Kirsch, T. D. (2021). The COVID-19 pandemic challenge to the All-Hazards Approach for disaster planning. International Journal of Disaster Risk Reduction, 55, 102103.
Schwartz, R., Liu, B., Sison, C., Kerath, S. M., Breil, T., Murphy, L., & Taioli, E. (2016). Study design and results of a population-based study on perceived stress following Hurricane Sandy. Disaster Medicine and Public Health Preparedness, 10(3), 325–332.
Tang, B., Liu, X., Liu, Y., Xue, C., & Zhang, L. (2014). A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health, 14(1), 1–12.
Tsuboya, T., Aida, J., Hikichi, H., Subramanian, S. V., Kondo, K., Osaka, K., & Kawachi, I. (2016). Predictors of depressive symptoms following the Great East Japan earthquake: A prospective study. Social Science & Medicine, 161, 47–54.
United Nations. (2020). United nations policy brief: COVID-19 and the need for action on mental health. Available at: https://www.un.org/sites/un2.un.org/files/un_policy_brief-covid_and_mental_health_final.pdf. Accessed December 6, 2022.
van den Besselaar, J. H., Vroomen, J. L. M., Buurman, B. M., Hertogh, C. M., Huisman, M., Kok, A. A., & Hoogendijk, E. O. (2021). Symptoms of depression, anxiety, and perceived mastery in older adults before and during the COVID-19 pandemic: Results from the Longitudinal Aging Study Amsterdam. Journal of Psychosomatic Research, 151, 110656.
van der Velden, P. G., Wong, A., Boshuizen, H. C., & Grievink, L. (2013). Persistent mental health disturbances during the 10 years after a disaster: Four-wave longitudinal comparative study. Psychiatry and Clinical Neurosciences, 67(2), 110–118.
Wilson-Genderson, M., Heid, A. R., & Pruchno, R. (2018). Long-term effects of disaster on depressive symptoms: Type of exposure matters. Social Science & Medicine, 217, 84–91.
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M., Gill, H., Phan, L., ..., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64.
Yan, Y., Du, X., Lai, L., Ren, Z., & Li, H. (2022). Prevalence of depressive and anxiety symptoms among Chinese older adults during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Geriatric Psychiatry and Neurology, 35(2), 182–195.
Zhang, S. X., Miller, S. O., Xu, W., Yin, A., Chen, B. Z., Delios, A., ..., & Chen, J. (2022). Meta-analytic evidence of depression and anxiety in Eastern Europe during the COVID-19 pandemic. European Journal of Psychotraumatology, 13(1), 2000132.
Zhu, A. Y. F., & Chou, K. L. (2022a). Depression among poor older adults: The role of social support. Social Science & Medicine, 311, 115293.
Zhu, A. Y. F., & Chou, K. L. (2022b). The Effects of multidimensional poverty on life satisfaction among older adults in Hong Kong. Journal of Applied Gerontology, 42(5), 1022–1034.
Funding
Open access funding provided by The Education University of Hong Kong The work described in this paper was fully supported by a grant from the Research Grants Council of the Hong Kong Special Administrative Region, China (Project No. EdUHK 18612718).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
The ethical approval was obtained from the Human Research Ethics Committee (HREC) of The Education University of Hong Kong before the data collection.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The author declares no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, A.Y.F., Chou, K.L. Depression among older adults before and during the pandemic: Follow-up assessment of a three-wave longitudinal observation. Curr Psychol 43, 16544–16553 (2024). https://doi.org/10.1007/s12144-023-05601-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-023-05601-1