Abstract
Sleep-related attentional bias, wherein exaggerated attention is directed to sleep-related stimuli, has been proposed to be part of the cognitive processes that underpin the development and perpetuation of insomnia. Attention deficit hyperactivity disorder (ADHD) is commonly associated with clinically significant sleep disturbances, although the nature of the relationship between ADHD and sleep is not well understood. We hypothesised that ADHD symptoms would associate with greater attentional bias to sleep-related stimuli. We used an emotional Stroop task with sleep-related words to assess the presence of sleep attentional bias in a sample of 155 younger adults. ADHD symptoms and consistency with the presence of ADHD was assessed with the Adult ADHD Self Report Screener and insomnia symptoms and probability for the presence of insomnia disorder was assessed with the Sleep Condition Indicator. ADHD symptoms and consistency, and insomnia symptoms and probability for the presence of insomnia disorder, were not found to associate with sleep attentional bias scores. Sleep attentional bias also did not associate with chronotype or social jetlag, but habitual use of an alarm clock on work-free days associated with greater sleep attentional bias. As such, we did not find evidence to support the hypothesis that ADHD symptoms are associated with sleep attentional bias in a sample of healthy younger adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
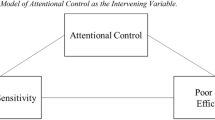
Sleep-related attentional bias, an attentional preference for sleep-related stimuli, has been observed in individuals diagnosed with insomnia disorder (Harris et al., 2015;Lundh et al., 1997; Taylor et al., 2003; Jones et al., 2005; MacMahon, et al., 2006; Ellis & Barclay, 2013; Akram et al., 2018). Such sleep attentional biases have also been reported to associate with poor subjective sleep quality in non-clinical populations (Spiegelhalder et al., 2008). It has been postulated that attentional biases occur when individuals are more likely to selectively allot information processing resources to sensory input related to their concerns (for example, see Mogg & Bradley, 2005 for attentional biases in anxiety disorders). In insomnia disorder, the attention-intention-effort model proposes that sleep-related stimuli will be more likely to induce threat through association with functional decline linked to insomnia, and lead to craving for sleep (Espie et al., 2006). As such, sleep attentional biases have been proposed as an important feature of the cognitive model of insomnia through a pathway in which worry about sleep leads to autonomic arousal and emotional distress, in turn leading to increased vigilance towards internal and external sleep-related threat cues (Harris et al., 2015; Milkins et al., 2016).
Sleep disturbances are reported to be common in attention deficit hyperactivity disorder (ADHD), with 70% of adults with ADHD reporting sleep-related concerns (Yoon et al., 2012; Bondopahyay et al., 2022; Bjorvatn et al., 2017) and a prevalence of insomnia disorder of 44% reported in adults with ADHD (Fadeuilhe et al., (2021a, 2021b). Clinical intervention for insomnia in adults with ADHD, such as psychoeducation, sleep hygiene and pharmacotherapy, may lead to improvement in ADHD symptoms, psychiatric comorbidities and overall quality of life (Fadeuilhe et al., 2021b). At present, the aetiology of sleep problems in ADHD is not well understood, and may comprise of neurocognitive, behavioral, homeostatic and circadian elements. As attentional sleep biases have been postulated to be an important component in the cognitive model of insomnia, and insomnia is highly prevalent in ADHD, it may be that attentional sleep biases contribute to sleep problems in ADHD. ADHD in adults is also associated with alterations in circadian rhythms in sleep–wake behaviours and molecular processes, including a marked tendency towards later chronotype and habitual sleep timing (Coogan & McGowan, 2017; Korman et al., 2019). It is also not currently clear if changes in chronotype and circadian function similar to those found in ADHD are associated with attentional sleep biases: MacMahon et al. (2006) have reported that patients with delayed sleep phase syndrome do not show greater sleep attentional biases, although there are no further reports in the literature examining circadian rhythms and sleep attentional biases.
As a disorder characterised by marked changes in attentional processes, ADHD may be associated with various attentional biases (Cremone et al., 2018; Pishyareh et al., 2015). For example, there is evidence that ADHD is associated with an attentional bias against sad faces (Shapero et al., 2021), for alcohol (Roberts et al., 2012) and for both positive and negative emotional words (Shushakova et al., 2018). However, there is no current examination of the presence of sleep attentional biases in either people with ADHD, or in relation to ADHD symptoms. As such, the current study tested the hypothesis that ADHD symptom severity in a non-clinical sample would associate with the presence of attentional sleep bias, that the presence of insomnia symptoms would associate with attentional sleep bias, and that the greatest attentional sleep bias would be present in participants with a combination of ADHD and insomnia symptoms. As secondary outcomes, we examined the association of sleep attentional bias with chronotype, social jetlag and habitual alarm clock usage.
Methods
Participants
We employed purposive sampling to recruit 165 (70% females) participants between the age range of 20- 35 years (mean age- 23.07, standard deviation- 3.77). Exclusion criteria were the presence of a significant medical or psychiatric history or a diagnosed sleep disorder. All participants were either under-graduate or post graduate students and provided informed consent. Ethical approval for the study was given by the Research Ethics Committee of Maynooth University.
Psychometrics
All participants completed an on-line questionnaire delivered through the Qualtrics platform. This questionnaire including questions relating to standard demographics such as age and gender.
ADHD symptoms
The presence of ADHD symptoms was assessed with the Adult ADHD Self Rating Scale (ASRS v 1.1), an 18 item self-report scale where a subject responds to a particular statement by selecting one of the 5 response options ranging from ‘never’, ‘rarely’, ‘sometimes’, ‘often’ and ‘very often’, and is based on the DSM-IV-TR criteria for adult ADHD (Adler et al., 2006). To produce a DSM-5 score from the ASRS, the 6 items from the Adult ADHD Self-Report Screening Scale for DSM-5 (ASRS-5) were also included in the measure. Two sets of scores for inattention and hyperactivity/impulsivity were derived from the ASRS 18 items in part A and part B. These scores were then divided into three categories, scores ranging from 0–16 (low ADHD inattention/hyperactivity), scores ranging from 17–23 (moderate ADHD inattention/hyperactivity and scores ranging 24 or above (high ADHD inattention/hyperactivity). Finally, a ADHD consistency/inconsistency category is evaluated from the ASRS v 1.1. The ASRS is described as having a negative predictive value for clinically-determined diagnosis of adult ADHD of 1 and a positive predictive value of 0.52 (Hines et al., 2012). As such, the screener has very strong properties for ruling out the presence of adult ADHD, and considerably more moderate properties for predicting the presence of adult ADHD.
Subjective Sleep Quality
Subjective sleep quality was assessed through two instruments. The Sleep Condition Indicator (SCI) is an eight-item screener based on the DSM-5 criteria for insomnia disorder (Espie et al., 2014). A total score of less than 16 indicated probability of insomnia features for the participant. The SCI has been reported to have a predictive value of ~ 0.85 for clinically diagnosed insomnia disorder according to DSM5 criteria (Wong et al., 2017). The Pittsburgh Sleep Quality Index (PSQI) is a commonly used and well validated questionnaire used to assesses subjective sleep quality a one month period (Buysee et al., 1989). The instrument is used to generate seven subscale scores relating to subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction, a a global PSQI score is produced through the summation of these sub-scale scores. Global PSQI scores of less than five indicates good sleeper status, and scores of equal or greater than 5 indicates bad sleeper status.
Trait Impulsivity
Trait impulsivity was assessed using the Barratt Impulsiveness Scale (BIS-11; Patton et al., 1995). The BIS-11 is a self-reported measure of 30 items scored as five point Likert-like responses. The BIS-11 has a three factor structure, producing subscale scores for “attentional impulsiveness”, “motor impulsiveness”, and “non-planning impulsiveness”, as well as a total trait impulsivity score.
Chronotype
Chronotype and social jetlag were derived from the Munich Chronotype Questionnaire (MCTQ; Roenneberg et al., 2012). This instrument enquires about habitual sleep habits and timing over the past 4 weeks on “work” days (those with scheduled commitments) and “free” days (those without formal work, study or other commitments). Alarm clock use on “work” and “free” days is asked about in a yes/no question. The main measures of sleep timing and chronotype produced by the the MCTQ are the times of mid-sleep (halfway between sleep onset and offset) on work (MSW). Sleep debt accumulated through the working week is corrected for to produce sleep-corrected MSF (MSFsc), which is taken as the lead indicator of the entrained circadian phase (Roenneberg et al., 2012). Social jetlag was calculated as the absolute difference between MSW and MSF, and is indicative of circadian misalignment arising out of a conflict between internal circadian time and social schedules (Roenneberg et al., 2012).
Sleep Attentional Biases
To assess sleep attentional biases we used a custom computerized sleep-related emotional Stroop task, presented via the Inquisit software system (Millisecond, Seattle, USA). We choose the emotional Stroop task to assess sleep attentional biases as a number of previous studies have presented evidence for the detection of sleep attentional biases in different populations using this approach (Lundh et al., 1997; Spiegelhalder et al., 2008, 2018; Zhou et al., 2018). Indeed, a recent meta-analysis has revealed that re-analysis of some previous findings from sleep emotional Stroop tasks has uncovered new evidence for the presence of sleep attentional biases in different sleep populations with moderate to large effect sizes (Akram et al., 2023).
Briefly, coloured words were randomly presented individually in the centre of a screen. Responses to these word stimuli were through participants pressing keyboard letters representing the colours of the words presented (red (D), blue (F), green (J) and yellow (K)). A fixation cross was presented on the screen for 500 ms before presentation of each word stimuli. Participants were first given 24 practice trials using words ‘one’- ‘ten’ as practice stimuli, followed by 2 blocks of 160 experimental trials (containing 4 categories of 10 words each, presented with 4 repetitions in random order). The 2 blocks of 160 trials were spaced in between one 2-min rest period. Word lists contained 10 sleep‐related derived from the study of Ellis and Barclay (2013), and 10 neutral, 10 positive and 10 negative words as per the Alcohol Emotional Stroop task (Bauer & Cox, 1998). The sleep‐related words were chosen specifically to lack affective connotations, and as previous research has demonstrated that participants with ADHD features are more susceptible to higher distractibility when faced with negative valenced emotional stimuli in an emotional attention task (Vetter et al., 2018). Details of the exact word lists used are in Supplementary Table 1. As performance characteristics of emotional Stroop tasks can be influenced by the lexical characteristics of the word stimuli used (Larsen, Mercer & Balota, 2006), we analysed the words used for lexical equivalence via the English Lexical Project analysis tool (https://elexicon.wustl.edu/index.html) for word length, normed word usage frequency, orthographic neighbourhood of used words, lexical reaction time and naming reaction time. The results of this analysis are detailed in Supplementary Table 2; we detected no statistically significant differences between the word types on any of these measures. The script for the emotional Stroop task used, as well as the data from the study, can be found at https://osf.io/zx3uy/.
The outputs obtained from the emotional Stroop test included reaction times for sleep, negative, positive and neutral words, and the interference index (the difference between the neutral and the sleep/negative/positive word reaction times). Only reaction times from correct trials were included in the analysis; reaction times from error trials were excluded from analysis. We used the sleep interference score (Mean RT Sleep – Mean RT Neutral per participant) as the principal measure of sleep attentional bias, with greater scores indicating more sleep attentional biases.
The study protocol straddled the introduction of Covid-19 pandemic restrictions on Spring 2020. Prior to the introduction of restrictions, the emotional Stroop task was conducted at a desktop PC in a sound proof cubicle (47% of participants). After the introduction of restriction, the Stroop tasks was delivered on the internet using the Inquisit web platform. Analysis of the mode of delivery revealed no difference between the two conditions; for example, comparing the sleep interference scores revealed a P = 0.99. As such, data from both conditions was collapsed and treated as one data set.
Data analysis
Statistical analysis was conducted with SPSS version 26 (IBM Corporation, USA). All data was assessed for normality and the presence of outliers using the Shapiro Wilk test and inspection of histograms. Legitimate values which were noted as outliers through box plots were winsorized to 1 + the highest value in that distribution and absolute outliers were removed from data set. Groupwise comparison of data was conducted using t-tests or ANOVAs for the primary measure of sleep vigilance, and MANOVA, for reaction times. Further, reaction time data from the Stroop tasks was assessed via mixed between-within group ANOVAs, with word type (neutral, positive, negative, sleep) as the within-subject factor and ADHD grouping oo insomnia grouping as the between-subjects factor. Correlation analysis was conducted with Spearman’s rho. To account for multiple correlation testing in inferential tests, alpha was adjusted to 0.01 for the primary outcome of interest, the sleep bias (vigilance) scores. Reaction time data were treated as secondary outcomes, and alpha was not adjusted from 0.05 for statistical significance. Results are presented in the text as mean values + standard error of the mean.
Results
Descriptive Statistics
29% of study participants were male, and the average age of participants was 23.05 years old (Table 1). 36% of participants were identified as being consistent with ADHD from their ASRS scores, and 33% of participants were identified as probable for insomnia disorder from the SCI scores; 15% of participants scored as being both ADHD consistent and insomnia probable. According to PSQI scores, 81% of participants scored 5 or greater indicating being a bad sleeper. 46% of participants reported habitually using an alarm clock on work-free days and 97% of participants reported using an alarm clock on “work” day mornings. The average timing of midsleep on free days (sleep corrected) was 05:06 and the mean social jetlag was 78 min (Table 1). ASRS scores were found to correlate moderately with SCI and PSQI scores (more ADHD symptoms associating with poorer sleep quality), and with MSFsc (later midsleep associating with greater ADHD scores; Table 2).
Sleep attentional bias according to ADHD and insomnia categories: hypothesis testing.
When examined according to ADHD-consistency based on ASRS scores (inconsistent/consistent), there was no statistically significant difference in the sleep bias scores on the Stroop test (-3.25 + 3.41 ms inconsistent vs 0.79 + 3.2 ms for consistent, P = 0.433; Fig. 1A). MANOVA revealed no effect of ADHD consistency on RT for any word type (Wilk’s Lambda, P = 0.648; Fig. 1 B-E). Further, mixed-between ANOVAs revealed no interaction between word-type x ADHD consistency on RT (F(3,435) = 0.172, P = 0.92; Fig. 1F). When performance on the Stroop task was examined according to insomnia disorder probability status (not probable/probable), there was no statistically significant difference on the sleep bias scores (0.85 + 3.01 ms improbable vs -7.02 + 4.45 ms for probable insomnia, P = 0.2; Fig. 2A). MANOVA revealed no effect of insomnia probability on RT for any word type (Wilk’s Lambda, P = 0.11; Fig. 2 B-E), and mixed-between ANOVAs revealed no interaction between word-type x insomnia probability on RT (F(3,435) = 2.04, P = 0.11; Fig. 2F). Further, no effects of PSQI good/bad sleeper status was found on any of the Stroop task scores examined (eg. sleep bias score -1.57 + 5.84 ms for good sleepers vs. -1.37 + 2.71 ms for bad sleepers, P = 0.98).
Violin-and-box plots showing groupwise comparisons according to ADHD-consistency status derived from ASRS response on (A) sleep attention bias scores (interference scores for sleep words), and reaction times to (B) sleep-related words, (C) negative words, (D) positive words and (E) neutral words. F Line graphs illustrating word-type x ADHD consistency analysis for reaction times (error bars indicate SEM)
Violin-and-box plots showing groupwise comparisons according to insomnia disorder probability status derived from SCI response on (A) sleep attention bias scores (interference scores for sleep words), and reaction times to (B) sleep-related words, (C) negative words, (D) positive words and (E) neutral words. F Line graphs illustrating word-type x insomnia probability analysis for reaction times (error bars indicate SEM)
For further analysis, ASRS scores were used to categorise participants according to inattention and hyperactivity/impulsivity status (low/moderate/high) and groupwise analysis on sleep vigilance scores was examined: there was no effect of either inattention status (F(2,148) = 1.21, P = 0.30; Fig. 3A) or hyperactivity/impulsivity status (F(2,148) = 0.61, P = 0.55; Fig. 3B).
Violin-and-box plots showing groupwise comparisons for sleep attentional bias scores based on participant classification from the ASRS inattention items (A), hyperactivity items (B) and according to whether participants were scored as both insomnia probable and ADHD-consistent, either insomnia probable or ADHD-consistent or neither (C). D-F show the analysis of group) x word type effects on reaction times (membership (inattentive group –D; hyperactivity group – E; combined insomnia/ADHD group – F). ** indicates P < 0.01 for between group main effect
We then examined sleep bias scores in individuals who were neither ADHD-consistent of insomnia probable, who were either ADHD-consistent or insomnia probable, and those who were both ADHD-consistent and insomnia probable; there was no effect of combined ADHD/insomnia status on sleep vigilance scores (F(2,148) = 0.31, P = 0.74; Fig. 3C). When examining reaction times for different word types, there was an effect of inattention category (F(1,144) = 4.82, P = 0.005) but no effect of word type (P = 0.541) or word type x inattention interaction (P = 0.723; Fig. 3 D). There were no statistically significant effects (P > 0.2 for all effect) for 2 way mixed ANOVAs for word type x either hyperactivity category (Fig. 3E) or combined ADHD/insomnia category (Fig. 3F).
Sleep attentional bias, ADHD symptoms and sleep quality: correlation analysis
We then examined scores as continuous scale variables, and consistent with the above did not find statistically significant correlations of sleep vigilance scores with ASRS total score, ASRS inattention score, ASRS hyperactivity/impulsivity score or BIS score for trait impulsivity (Fig. 4 A-D). Further, sleep vigilance scores did not associate significantly with SCI or PSQI total scores, or with MSFsc or social jetlag (Fig. 4 E–H).
Sleep attentional bias and alarm clock use: post-hoc analysis
Finally, we explored the association of sleep bias scores with self-reported alarm clock usage on work-free days. Participants who reported using an alarm clock to wake on work-free days showed more sleep attentional bias than those who did not (5.98 + 4.1 ms for alarm clock users vs. -8.93 + 2.98 ms, P = 0.005). Reaction times to sleep, neutral, positive and neutral words did not vary according to alarm clock use (P = 0.35, 0.93, 0.81, 0.73 respectively). Alarm clock on work-free days use did not vary according to insomnia probability status (P = 0.30, chi square test for independence), nor did it vary according to ADHD-consistency (P = 0.97). Alarm clock use on work days was not examined as 97% of participants reported using an alarm clock for wakening on work days (Fig. 5).
Violin-and-box plots showing groupwise comparisons of (A) sleep attentional bias scores, (B) reaction time to sleep-related words and (C) reaction times to neutral words according to if participant self-reported as habitually using an alarm clock on work days. ** denotes P < 0.01 by independent samples t-test
Discussion
In this study we examined whether subjectively reported ADHD symptoms associate with sleep attentional bias. Further, we examined whether insomnia symptoms and sleep quality associated with sleep attentional bias, as well as examining the associations of sleep attentional bias with chronotype, social jetlag and habitual alarm clock use. We did not find any association between ADHD-consistency and insomnia probability on sleep bias scores, nor did we find an effect of combined ADHD-consistency and insomnia probability. We did find that habitual alarm clock use was associated with greater sleep attentional bias.
Previous research has inconsistently reported the presence of attentional bias in insomnia disorder, although cognitive models of insomnia include bias to sleep related stimuli as component features (Akram et al., 2023; Harris et al., 2015). Given that sleep problems are commonly reported in adults with ADHD (Coogan & McGowan, 2017), we hypothesised that ADHD features would associate with sleep attentional bias. We were somewhat surprised that neither ADHD nor insomnia symptoms associated with sleep attentional bias, as previous literature has indicated that insomnia/poor quality sleep was associated with sleep attentional biases, as assessed by various tasks to estimate bias (Taylor et al., 2003; Jones et al., 2005; MacMahon et al., 2006; Ellis & Barclay, 2013). Whilst some previous studies used reaction times to sleep-related words on the emotional Stroop test as an indicator of sleep attentional bias, rather than the sleep word interference score (eg. Ellis & Barclay, 2013), a recent meta-analysis has recalculated those values as sleep bias scores and report that sleep attentional biases are indeed associated with poor sleeper status and with the presence of insomnia disorder (Akram et al., 2023). Further, we did not detect any groupwise differences on reaction times for sleep-related words according to either ADHD-consistency or insomnia probability; as such, we do not believe that the lack of associations detected is contingent on the measure used (sleep bias score vs. reaction time for sleep words). It is notable that a number of previous studies did not report an attentional bas towards sleep-related stimuli in individuals with insomnia (Lancee et al., 2017; Lundh et al., 1997; Spiegelhalder et al., 2008). One reason for discrepancy in the literature is the nature of the task that is used to assess this attention bias and the nature of the sleep related stimulus presented to the participant, with the emotional Stroop test reported to be less sensitive to sleep attentional bias compared to dot-probe, flicker or Posner tasks (Harris et al., 2015).
One further consideration is that the study of Ellis and Barclay (2013), which used an emotional Stroop task, sampled participants in the evening time (rather than the day-time in the current study); as such, greater homeostatic sleep pressure associated with later in the day may contribute to the detection of sleep attentional bias. A final consideration is that in our study, sleep quality and the probable insomnia status was determined by subjective measures, rather than objective tests such as actigraphy or polysomnography. Spiegelhalder et al. (2010) demonstrated an unexpected positive association between attention bias and improved markers of sleep duration and continuity measured by polysomnography when using a Dot probe task, although attention bias on an emotional Stroop task was not correlated with the polysomnography parameters.
Inattention category was associated with a main effect on reaction times that was not sensitive to word type, with those with lower levels of inattention showing slower reaction times to all word types. Hyperactivity category was not associated a main effect on reaction times, and neither inattention or hyperactivity category was associated with sleep bias scores. Shushakova et al. (2018) report that particpants with ADHD tended towards slower reaction times in response to emotional words; however, our results indicates that reaction times are similarly slower to neutral, positive, negative and sleep-related words in participants with low inattention. Posner et al. (2011) showed that reaction times were slowed by positive and negative distractor words in both healthy controls and people with ADHD. The most straightforward explanation of the current finding is that participants with low inattention will be most prone to cognitive distraction of the interfering words on the Stroop task, and as such display slower reaction times independent of word type (hence the lack of bias scores as reaction to neutral words are similarly slowed as test words). As sleep problems are associated with increased inattention (eg. McGowan et al., 2020), we suggest that future work on assessing sleep attentional biases in poor sleep and in sleep disorders should incorporate indicators of general inattention.
We did find a sleep attentional bias in participants who habitually used alarm clocks to wake on “work” days versus those who did not, indicating that participants whose sleep on work days was curtailed by their social demands were more cognitively oriented towards sleep-related stimuli (no bias effect was detected for positive or negative words). Interestingly, there was no relationship of social jetlag with sleep bias, indicating that alarm clock use in this context appears not to be a proxy for social jetlag. A recent report has identified the Munich Chronotype Questionnaire as the only sleep questionnaire that asks about the method of wakening (Robbins et al., 2021). As such, alarm clock usage, or other methods of wakening, may be underexplored factors in exploring cognitive processes in sleep disorders. Clock monitoring has been proposed as a factor that contributes to the persistence of insomnia disorder through amplification of pre-sleep worry (Tang et al., 2007), although it is not clear if habitual alarm clock use may influence clock monitoring behaviours. It is also not clear from the current data which, if any, other wakening method participants who did not use alarm clocks utilised to facilitate wakening on “work” days.
There are a number of important limitations in our study. Participants’ sleep measures were based on subjective reports rather than a combination of objective and subjective tools, thereby not controlling for potential personal biases in responses and the effect of individual differences in interpretation of inventory questions. ADHD features were evaluated through a screener questionnaire rather than a comprehensive diagnostic assessment, introducing the potential for confounding effects arising from participants’ misinterpretation of item questions and for limited specificity in categorisation of individuals as “ADHD consistent”. Further, we did not explore the participant’s psychological/mood states which might have affected their performance on the Stroop test, nor did we assess acute sleepiness at the time of testing. The performance of emotional Stroop tests has been shown to be influenced by the lexical characteristics of the stimuli used (Larsen et al., 2006); our analysis of the stimuli used in this study indicates that whilst there were not significant differences in lexical parameters according to word type, exact equivalence equally could not be assumed and this may have influenced test performance (although a similar observation could be made of previously published studies of sleep attentional biases). Other types of tests have previously been used to detect sleep attentional bias, such as dot-probe and Posner tasks (Akram et al., 2023; Harris et al., 2015), and it is possible that the use of these paradigms would have yielded different results. Participants were young adult university students, and as such findings might not generalise to other populations; we also note the high rate of ADHD-consistency from the ASRS scores and probable insomnia disorder from the SCI scores in the study population, perhaps reflecting a level of self-selection into the study from participants with ADHD and insomnia symptoms. Finally, the effect of alarm clock use on sleep attention bias was discovered during exploratory analysis, and was not tested as an a priori hypothesis.
Conclusion
The aetiology of sleep problems commonly reported in ADHD remains poorly understood. The examination of cognitive factors implicated in insomnia and other sleep disorders in sleep problems in ADHD will be of importance, given the cognitive nature of the core symptoms of ADHD. The current findings do not implicate sleep attentional bias as part of link between ADHD and sleep, although as noted there are doubts in the literature as to whether sleep attentional biases play substantive roles in insomnia.
Data availability
The data used for analysis and preparation of the presented results in this paper are available in the Supplementary Materials.
References
Adler, L. A., Spencer, T., Faraone, S. V., Kessler, R. C., Howes, M. J., Biederman, J., & Secnik, K. (2006). Validity of pilot Adult ADHD Self- Report Scale (ASRS) to Rate Adult ADHD symptoms. Annals of Clinical Psychiatry, 18(3), 145–148. https://doi.org/10.1080/10401230600801077
Akram, U., Barclay, N. L., & Milkins, B. (2018). Sleep-Related Attentional Bias in Insomnia: Time to Examine Moderating Factors? Frontiers in Psychology, 9, 2573. https://doi.org/10.3389/fpsyg.2018.02573
Akram, U., Barclay, N. L., Milkins, B., Stevenson, J., & Gardani, M. (2023). Sleep-related attentional and interpretive-bias in insomnia: A systematic review and meta-analysis. Sleep Medicine Reviews, 67, 101713. https://doi.org/10.1016/j.smrv.2022.101713
Bauer, D., & Cox, W. M. (1998). Alcohol-related words are distracting to both alcohol abusers and non-abusers in the Stroop colour-naming task. Addiction, 93(10), 1539–1542. https://doi.org/10.1046/j.1360-0443.1998.9310153910.x
Bjorvatn, B., Brevik, E. J., Lundervold, A. J., Halmøy, A., Posserud, M. B., Instanes, J. T., & Haavik, J. (2017). Adults with attention deficit hyperactivity disorder report high symptom levels of troubled sleep, restless legs, and cataplexy. Frontiers in Psychology, 8, 1621. https://doi.org/10.3389/fpsyg.2017.01621
Bondopadhyay, U., Diaz-Orueta, U., & Coogan, A. N. (2022). A systematic review of sleep and circadian rhythms in children with attention deficit hyperactivity disorder. Journal of Attention Disorders, 26(2), 149–222. https://doi.org/10.1177/1087054720978556
Buysse, D. J., Reynolds, C. F., 3rd., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Coogan, A. N., & McGowan, N. M. (2017). A systematic review of circadian function, chronotype and chronotherapy in attention deficit hyperactivity disorder. Attention Deficit Hyperactivity Disorders., 9(3), 129–147. https://doi.org/10.1007/s12402-016-0214-5
Cremone, A., Lugo-Candelas, C. I., Harvey, E. A., McDermott, J. M., & Spencer, R. M. (2018). Positive emotional attention bias in young children with symptoms of ADHD. Child Neuropsychology, 24(8), 1137–1145. https://doi.org/10.1080/09297049.2018.1426743
Ellis, N. L., & Barclay, J. G. (2013). Sleep-related attentional bias in poor versus good sleepers is independent of affective valence. Journal of Sleep Research, 2(4), 414–421. https://doi.org/10.1111/jsr.12035
Espie, C. A., Broomfield, N. M., Macmahon, K. M., Macphee, L. M., & Taylor, L. M. (2006). The attention-intention-effort pathway in the development of psychophysiological insomnia: A theoretical review. Sleep Medicine Reviews, 10, 215–245. https://doi.org/10.1016/j.smrv.2006.03.002
Espie, C. A., Kyle, S. D., Hames, P., Gardani, M., Fleming, L., & Cape, J. (2014). The Sleep Condition Indicator: a clinical screening tool to evaluate insomnia disorder. BMJ Open, 4(3), e004183. https://doi.org/10.1136/bmjopen-2013-004183
Fadeuilhe, C., Daigre, C., Richarte, V., Grau-López, L., Palma-Álvarez, R. F., Corrales, M., & Ramos-Quiroga, J. A. (2021a). Insomnia disorder in adult attention-deficit/hyperactivity disorder patients: clinical, comorbidity, and treatment correlates. Frontiers in Psychiatry, 12. https://doi.org/10.3389/fpsyt.2021.663889
Fadeuilhe, C., Daigre, C., Grau-López, L., Richarte, V., Palma-Álvarez, R. F., Corrales, M., ... & Ramos-Quiroga, J. A. (2021b). The impact of insomnia disorder on adult attention-deficit/hyperactivity disorder severity: A six-month follow-up study. Psychiatry Research, 11, 4349. https://doi.org/10.1016/j.psychres.2021.114349
Fayyad, J., De Graaf, R., Kessler, R., Alonso, J., Angermeyer, M., Demyttenaere, K., ... & Jin, R. (2007). Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. The British Journal of Psychiatry, 190(5), 402–409. https://doi.org/10.1192/bjp.bp.106.034389
Harris, K., Spiegelhalder, K., Espie, C. A., MacMahon, K. M. A., Cleland Woods, H., & Kyle, S. D. (2015). Sleep-related attentional bias in insomnia: A state-of-the-science review. Clinical Psychology Review, 42, 16–27. https://doi.org/10.1016/j.cpr.2015.08.001
Hines, J. L., King, T. S., & Curry, W. J. (2012). The adult ADHD self-report scale for screening for adult attention deficit-hyperactivity disorder (ADHD). Journal of the American Board of Family Medicine, 25(6), 847–853. https://doi.org/10.3122/jabfm.2012.06.120065
Jones, B. T., Macphee, L. M., Jones, B. C., Broomfield, N. M., & Espie, C. A. (2005). Sleep-related attentional bias in good, moderate, and poor (primary insomnia) sleepers. Journal of Abnormal Psychology, 114, 249–258. https://psycnet.apa.org/doi/10.1037/0021-843X.114.2.249
Korman, M., Levy, I., Maaravi-Hesseg, R., Eshed-Mantel, A., & Karni, A. (2019). Subclinical scores in self-report based screening tools for attention deficits correlate with cognitive traits in typical evening-type adults tested in the morning. Frontiers in Psychology, 10, 1397. https://doi.org/10.3389/fpsyg.2019.01397
Lancee, J., Yasiney, S. L., Brendel, R. S., Boffo, M., Clarke, P., & Salemink, E. (2017). Attentional bias modification training for insomnia: A double-blind placebo controlled randomized trial. PloS One, 12(4), e0174531. https://doi.org/10.1371/journal.pone.0174531
Larsen, R. J., Mercer, K. A., & Balota, D. A. (2006). Lexical characteristics of words used in emotional Stroop experiments. Emotion, 6(1), 62–72. https://doi.org/10.1037/1528-3542.6.1.62
Lundh, L. G., Froding, A., Gyllenhammar, L., Broman, J. E., & Hetta, J. (1997). Cognitive bias and memory performance in patients with persistent insomnia. Cognitive Behaviour Therapy, 26(1), 27–35. https://doi.org/10.1080/16506079708412033
MacMahon, K. M., Broomfield, N. M., & Espie, C. A. (2006). Attention bias for sleep-related stimuli in primary insomnia and delayed sleep phase syndrome using the dot-probe task. Sleep, 29(11), 1420–1427. https://doi.org/10.1093/sleep/29.11.1420
McGowan, N. M., Uzoni, A., Faltraco, F., Thome, J., & Coogan, A. N. (2020). The impact of social jetlag and chronotype on attention, inhibition and decision making in healthy adults. Journal of Sleep Research, 29(6), e12974. https://doi.org/10.1111/jsr.12974
Milkins, B., Notebaert, L., MacLeod, C., & Clarke, P. J. (2016). The potential benefits of targeted attentional bias modification on cognitive arousal and sleep quality in worry-related sleep disturbance. Clinical Psychological Science, 4(6), 1015–1027. https://doi.org/10.1177/2167702615626898
Mogg, K., & Bradley, B. P. (2005). Attentional bias in generalized anxiety disorder versus depressive disorder. Cognitive Therapy and Research, 29(1), 29–45. https://doi.org/10.1007/s10608-005-1646-y
Patton, J. H., Stanford, M. S., & Barratt, E. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology, 51(6), 768–774. https://doi.org/10.1002/1097-4679(199511)51:6%3C768::AID-JCLP2270510607%3E3.0.CO;2-1
Pishyareh, E., Tehrani-Doost, M., Mahmoodi-Gharaie, J., Khorrami, A., & Rahmdar, S. R. (2015). A comparative study of sustained attentional bias on emotional processing in ADHD children to pictures with eye-tracking. Iranian Journal of Child Neurology, 9(1), 64.
Posner, J., Maia, T. V., Fair, D., Peterson, B. S., Sonuga-Barke, E. J., & Nagel, B. J. (2011). The attenuation of dysfunctional emotional processing with stimulant medication: An fMRI study of adolescents with ADHD. Psychiatry Research, 193(3), 151–160. https://doi.org/10.1016/j.pscychresns.2011.02.005
Roberts, W., Fillmore, M. T., & Milich, R. (2012). Drinking to distraction: Does alcohol increase attentional bias in adults with ADHD? Experimental and Clinical Psychopharmacology, 20(2), 107–117. https://doi.org/10.1037/a0026379
Robbins, R., Quan, S. F., Barger, L. K., Czeisler, C. A., Fray-Witzer, M., Weaver, M. D., Zhang, Y., Redline, S., & Klerman, E. B. (2021). Self-reported sleep duration and timing: A methodological review of event definitions, context, and timeframe of related question. Sleep Epidemioliology, 1, 100016. https://doi.org/10.1016/j.sleepe.2021.100016
Roenneberg, T., Allebrandt, K. V., Merrow, M., & Vetter, C. (2012). Social jetlag and obesity. Current Biology, 22(10), 939–943. https://doi.org/10.1016/j.cub.2012.03.038
Shapero, B. G., Gibb, B. E., Archibald, A., Wilens, T. E., Fava, M., & Hirshfeld-Becker, D. R. (2021). Risk factors for depression in adolescents with ADHD: The impact of cognitive biases and stress. Journal of Attention Disorders, 25(3), 340–354. https://doi.org/10.1177/1087054718797447
Shushakova, A., Wiesner, C. D., Ohrmann, P., & Pedersen, A. (2018). Electrophysiological evidence of an attentional bias towards appetitive and aversive words in adults with attention-deficit/hyperactivity disorder. Clinical Neurophysiology, 129(9), 1937–1946. https://doi.org/10.1016/j.clinph.2018.06.019
Spiegelhalder, K., Espie, C., Nissen, C., & Riemann, D. (2008). Sleep-related attentional bias in patients with primary insomnia compared with sleep experts and healthy controls. Journal of Sleep Research, 17(2), 191–196. https://doi.org/10.1111/j.1365-2869.2008.00641.x
Spiegelhalder, K., Kyle, S. D., Feige, B., Prem, M., Nissen, C., Espie, C. A., & Riemann, D. (2010). The impact of sleep-related attentional bias on polysomnographically measured sleep in primary insomnia. Sleep, 33(1), 107–112. https://doi.org/10.1093/sleep/33.1.107
Spiegelhalder, K., Baglioni, C., Regen, W., Kyle, S. D., Nissen, C., Hennig, J., Doerr, J. P., Feige, B., & Riemann, D. (2018). Brain reactivity and selective attention to sleep-related words in patients with chronic insomnia. Behavioral Sleep Medicine, 16(6), 587–600. https://doi.org/10.1080/15402002.2016.1253014
Tang, N. K., Anne Schmidt, D., & Harvey, A. G. (2007). Sleeping with the enemy: Clock monitoring in the maintenance of insomnia. Journal of Behavior Therapy and Experimental Psychiatry, 38(1), 40–55. https://doi.org/10.1016/j.jbtep.2005.07.004
Taylor, L. M., Espie, C. A., & White, C. A. (2003). Attentional bias in people with acute versus persistent insomnia secondary to cancer. Behavioral Sleep Medicine, 1(4), 200–212. https://doi.org/10.1207/S15402010BSM0104_3
Vetter, N. C., Buse, J., Backhausen, L. L., Rubia, K., Smolka, M. N., & Roessner, V. (2018). Anterior insula hyperactivation in ADHD when faced with distracting negative stimuli. Human Brain Mapping, 39(7), 2972–2986. https://doi.org/10.1002/hbm.24053
Wong, M. L., Lau, K. N. T., Espie, C. A., Luik, A. I., Kyle, S. D., & Lau, E. Y. Y. (2017). Psychometric properties of the sleep condition indicator and insomnia severity index in the evaluation of insomnia disorder. Sleep Medicine, 33, 76–81. https://doi.org/10.1016/j.sleep.2016.05.019
Yoon, S. Y., Jain, U., & Shapiro, C. (2012). Sleep in attention-deficit/hyperactivity disorder in children and adults: Past, present, and future. Sleep Medicine Reviews, 16(4), 371–388. https://doi.org/10.1016/j.smrv.2011.07.001
Zhou, N., Zhao, C., Yang, T., Du, S., Yu, M., & Shen, H. (2018). Attentional bias towards sleep-related stimuli in insomnia disorder: A behavioural and ERP study. Journal of Sleep Research, 27(3), e12652. https://doi.org/10.1111/jsr.12652
Funding
Open Access funding provided by the IReL Consortium
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval for the study was given by the Research Ethics Committee of Maynooth University. Informed consent was given by all study participants. No funding was received for conducting this study. The authors have no conflicts of interest to disclose.
Conflict of interest
The authors have no potential conflicts to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bondopadhyay, U., Coogan, A.N. Sleep-related attentional bias does not associate with symptoms of ADHD in a sample of younger adults. Curr Psychol 43, 10557–10566 (2024). https://doi.org/10.1007/s12144-023-05150-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-023-05150-7